Intra Cytoplasmic Sperm Injection (ICSI) is an advanced form of in vitro fertilization (IVF) used to treat severe male infertility. ICSI involves the direct injection of a single sperm into an egg in a laboratory setting, bypassing the natural fertilization process. It is particularly beneficial for men with low sperm count, poor sperm motility, or sperm morphology issues that prevent them from achieving fertilization through conventional IVF methods.
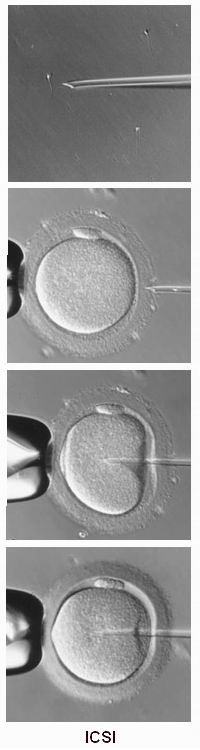
The process begins with the extraction of eggs from the woman, which are then fertilized in the laboratory. Unlike standard IVF, where sperm is placed with the egg and fertilization is left to occur naturally, ICSI uses a fine needle to inject a sperm directly into an egg, ensuring that fertilization occurs even if the sperm’s quality is compromised.
ICSI is often the treatment of choice in cases where male infertility is the primary issue, but it can also be used in female infertility cases if other causes, such as polycystic ovary syndrome (PCOS) or egg quality issues, are present. ICSI is also used when previous IVF attempts have failed.
Over the years, ICSI has become a standard procedure in many fertility clinics worldwide, with a high success rate, particularly in severe cases of male infertility.
ICSI is primarily used in cases where male infertility plays a significant role in the inability to conceive. Understanding the underlying causes and risk factors that lead to the need for ICSI is essential to evaluate its necessity and potential benefits.
Causes of Male Infertility Leading to ICSI
-
Low Sperm Count (Oligospermia):
-
A significant reduction in the number of sperm produced can severely impact fertility. ICSI can help achieve fertilization even with very few sperm present.
-
-
Poor Sperm Motility (Asthenozoospermia):
-
If the sperm are unable to swim properly toward the egg, fertilization is unlikely. ICSI allows even non-motile sperm to be injected directly into the egg, overcoming this issue.
-
-
Abnormal Sperm Morphology (Teratozoospermia):
-
Some men produce sperm that is abnormally shaped and unable to fertilize an egg naturally. ICSI can bypass this challenge by selecting the best sperm for injection into the egg.
-
-
Obstructive Azoospermia:
-
In cases where sperm production is normal but there is a blockage in the reproductive tract preventing sperm from being ejaculated, sperm can be extracted directly from the testicles (using a procedure like testicular sperm extraction (TESE)) for use in ICSI.
-
-
Non-Obstructive Azoospermia:
-
This condition occurs when sperm production in the testes is very low or absent. ICSI can help with sperm retrieved directly from the testicles, even in cases of minimal sperm production.
-
-
Previous IVF Failure:
-
When traditional IVF has failed due to fertilization issues, ICSI can be considered as it increases the chances of successful fertilization.
-
-
Genetic Issues:
-
In some cases, male infertility is caused by genetic factors, such as Y chromosome microdeletions or cystic fibrosis, that affect sperm production and function. ICSI may be recommended in these cases, although genetic counseling may be required.
-
-
Female Factor Infertility:
-
Though ICSI is a technique designed to address male infertility, it can also be used in certain cases of female infertility, particularly when the quality of eggs is compromised.
-
Risk Factors for Needing ICSI
-
Age of the Male Partner:
-
As men age, sperm quality tends to decline, leading to lower motility, morphology, and overall count. This may necessitate the use of ICSI for successful fertilization.
-
-
Previous Failed Fertility Treatments:
-
Couples who have attempted traditional IVF but faced issues with fertilization may benefit from ICSI as an alternative approach.
-
-
History of Infertility:
-
Couples with a long-standing history of unexplained infertility, or where the male partner has known fertility issues, may be more likely to require ICSI.
-
-
Lifestyle Factors:
-
Smoking, excessive alcohol use, poor diet, and stress are risk factors that can affect sperm quality and increase the likelihood that ICSI may be necessary.
-
While ICSI itself does not present direct symptoms or signs, there are several factors that might indicate the need for this treatment. The primary indications for ICSI are related to male infertility issues that hinder the natural fertilization process.
Symptoms Indicating the Need for ICSI
-
Inability to Conceive:
-
Couples who have been trying to conceive for a year or more without success, especially when male infertility factors like low sperm count or motility are identified, may be advised to consider ICSI.
-
-
Male Infertility Diagnosis:
-
If a sperm analysis reveals low sperm count, poor sperm motility, or abnormal sperm morphology, ICSI may be recommended as the next step for fertilization.
-
-
Previous Failed IVF Attempts:
-
If traditional IVF methods fail to achieve fertilization, ICSI is often the next step, as it bypasses the need for sperm to reach and penetrate the egg naturally.
-
-
Sexual Dysfunction:
-
Men with erectile dysfunction or ejaculation issues may face challenges in sperm collection. In such cases, sperm can be retrieved directly from the testes and used in ICSI.
-
-
Genetic Concerns:
-
Couples concerned about passing on genetic disorders to their children may choose ICSI to select the healthiest sperm for fertilization. Additionally, sperm testing for genetic abnormalities can be part of the ICSI process.
-
The diagnosis process for ICSI involves identifying the underlying cause of infertility, particularly male infertility. A thorough evaluation is necessary to determine if ICSI is appropriate for a couple’s treatment plan.
Diagnostic Steps:
-
Semen Analysis:
-
A semen analysis is the primary diagnostic test for male infertility. This test evaluates sperm count, motility, and morphology. If the sperm quality is poor or the count is very low, ICSI may be considered.
-
-
Hormonal and Blood Tests:
-
Hormonal levels in the male partner, including testosterone, FSH (follicle-stimulating hormone), and LH (luteinizing hormone), may be tested to assess overall reproductive health.
-
-
Genetic Testing:
-
Genetic screening can be performed to evaluate for any potential genetic causes of infertility, such as Y chromosome microdeletions or other hereditary issues that affect sperm production.
-
-
Testicular Biopsy or Sperm Extraction:
-
In cases of azoospermia (lack of sperm in the ejaculate), sperm may be extracted directly from the testes via surgical sperm retrieval techniques, such as TESE (testicular sperm extraction) or PESA (percutaneous sperm aspiration).
-
-
Female Fertility Testing:
-
Female fertility factors must also be evaluated to determine whether egg quality or other factors contribute to infertility. If the female partner’s fertility is compromised, egg retrieval and IVF/ICSI may be considered.
-
ICSI is part of a broader infertility treatment plan, typically used in conjunction with IVF (In Vitro Fertilization). Here are the treatment options involved in ICSI:
-
Ovarian Stimulation for the Female Partner:
-
The first step in an ICSI treatment cycle is stimulating the female partner’s ovaries to produce multiple eggs using hormone injections. These eggs are then retrieved through a minimally invasive procedure.
-
-
Sperm Collection:
-
For male partners, sperm is collected via masturbation or surgical sperm retrieval techniques (in cases of azoospermia). The sperm is then processed in the laboratory to select the healthiest sperm for injection.
-
-
ICSI Procedure:
-
The sperm is injected directly into the egg using a fine needle, bypassing the need for the sperm to fertilize the egg naturally. The embryo is then cultured in the lab for a few days.
-
-
Embryo Transfer:
-
After fertilization, the resulting embryos are monitored for growth. One or more healthy embryos are selected and transferred into the woman’s uterus using a catheter. The procedure is painless and non-invasive.
-
-
Pregnancy Monitoring:
-
After the embryo transfer, the woman’s pregnancy is closely monitored through blood tests and ultrasound scans to confirm implantation and fetal development.
-
Though ICSI is highly effective, proper management is essential for optimal success and minimizing risks.
Prevention Measures:
-
Male Fertility Health:
-
Maintaining a healthy lifestyle, including avoiding smoking, alcohol consumption, and stress, can help improve sperm quality and potentially reduce the need for ICSI.
-
-
Early Fertility Screening:
-
Early diagnosis and treatment of male infertility issues can improve outcomes for IVF/ICSI treatments.
-
-
Genetic Counseling:
-
Couples undergoing ICSI may benefit from genetic counseling to understand potential genetic risks and implications for the child.
-
Management of ICSI Treatment:
-
Monitoring Hormonal Levels:
-
Regular monitoring of the female partner’s hormonal levels and egg production during the stimulation phase is essential for ensuring optimal response to treatment.
-
-
Managing Emotional Health:
-
IVF/ICSI treatments can be emotionally taxing. Providing psychological support and counseling to the couple throughout the treatment process can help manage stress and anxiety.
-
Though ICSI is considered safe and effective, it carries certain risks and potential complications:
-
Ovarian Hyperstimulation Syndrome (OHSS):
-
This condition occurs when the ovaries become swollen and painful due to excessive response to the hormonal stimulation used in IVF. It can cause bloating, abdominal pain, and, in severe cases, fluid accumulation.
-
-
Multiple Pregnancies:
-
Although only one embryo is typically transferred, there is a risk of multiple pregnancies (twins or triplets) due to the success of ICSI, which can carry increased health risks for both the mother and babies.
-
-
Ectopic Pregnancy:
-
In rare cases, the embryo may implant outside the uterus, typically in the fallopian tube, resulting in an ectopic pregnancy.
-
-
Emotional and Psychological Impact:
-
The emotional strain of going through IVF/ICSI treatment can lead to stress, anxiety, and even depression for both partners.
-
-
Failed ICSI Cycles:
-
Despite the high success rates of ICSI, there are instances where the procedure may fail, resulting in miscarriage or lack of pregnancy.
-
Living with the emotional, physical, and psychological aspects of ICSI treatment can be a challenge for couples. However, it also provides a sense of hope for those struggling with infertility.
Living Post-Treatment:
-
Emotional Adjustment:
-
Couples may experience a variety of emotions, from joy and excitement to anxiety and fear of failure. Ongoing emotional support is critical throughout the process.
-
-
Long-Term Family Planning:
-
For couples who achieve pregnancy through ICSI, the journey may continue with the joy of expanding their family. For others, frozen embryos may provide future opportunities for additional pregnancies.
-
-
Genetic Considerations:
-
For couples who are concerned about the genetic implications of their infertility treatment, genetic counseling can provide insight into potential risks for the child.
-
1. What is Intra Cytoplasmic Sperm Injection (ICSI)?
Intra Cytoplasmic Sperm Injection (ICSI) is an advanced form of in vitro fertilization (IVF) where a single sperm is directly injected into an egg to achieve fertilization. It is used to overcome male infertility issues, especially when there are problems with sperm count, motility, or morphology.
2. Why is ICSI used?
ICSI is primarily used in cases of male infertility, such as:
-
Low sperm count or oligospermia.
-
Poor sperm motility or asthenozoospermia.
-
Abnormal sperm morphology or teratozoospermia.
-
Previous IVF failure due to poor fertilization.
ICSI allows fertilization to occur even when the sperm quality is compromised.
3. How is ICSI performed?
The ICSI procedure involves the following steps:
-
Ovarian stimulation: The woman undergoes hormone therapy to stimulate the ovaries to produce multiple eggs.
-
Egg retrieval: Once the eggs are mature, they are retrieved from the ovaries.
-
Sperm collection: A sperm sample is collected from the male partner. In cases where there is no sperm in the ejaculate, sperm may be retrieved directly from the testes or epididymis.
-
Sperm injection: A single sperm is injected directly into the cytoplasm of each mature egg.
-
Embryo culture: The fertilized eggs are monitored and cultured for several days before being transferred to the woman's uterus.
4. How is ICSI different from traditional IVF?
In traditional IVF, sperm is placed in a dish with the eggs and fertilization occurs naturally. In ICSI, a single sperm is directly injected into an egg using a fine needle. This makes ICSI particularly useful in cases of male infertility where sperm quality or quantity is an issue, whereas traditional IVF may be less effective in these cases.
5. What are the success rates of ICSI?
The success rates of ICSI depend on several factors, including the woman’s age, egg quality, and the male partner’s sperm quality. On average, the fertilization rate for ICSI is high, typically around 60-70%. Success rates for pregnancy and live birth depend on factors like embryo quality and the health of the recipient. Generally, ICSI success rates are similar to traditional IVF when the procedure is performed under optimal conditions.
6. What are the risks of ICSI?
While ICSI is generally considered safe, there are some risks associated with the procedure:
-
Ovarian Hyperstimulation Syndrome (OHSS): A potential complication from ovarian stimulation, leading to swollen ovaries and fluid retention.
-
Multiple pregnancies: As with IVF, there is an increased chance of twins or more, especially if multiple embryos are transferred.
-
Sperm DNA damage: In rare cases, sperm used in ICSI may have damaged DNA, which can affect embryo development or increase the risk of genetic conditions.
-
Possible long-term risks: Some studies suggest a slightly higher risk of birth defects or genetic conditions with ICSI, although these risks are still being studied.
7. Is ICSI suitable for everyone?
ICSI is often recommended for men with severe male infertility, but it may not be suitable for all patients. It is typically recommended when there are issues with sperm quality, quantity, or previous IVF failures. Women with certain health conditions or those who have been diagnosed with unexplained infertility may also benefit from ICSI. A thorough consultation with a fertility specialist is necessary to determine if ICSI is the right treatment option.
8. How long does the ICSI procedure take?
The entire ICSI process typically takes about 2-3 weeks:
-
Ovarian stimulation: About 10-14 days of hormone therapy to stimulate the ovaries.
-
Egg retrieval: Typically done under sedation and takes about 20-30 minutes.
-
ICSI procedure: The sperm injection itself is done in a few hours, usually within a day of egg retrieval.
-
Embryo transfer: 3-5 days after fertilization, when the embryos are ready for transfer to the woman’s uterus.
9. What is the cost of ICSI?
The cost of ICSI varies depending on the fertility clinic, location, and additional services required. On average, the cost of an ICSI cycle ranges between $5,000 to $15,000, excluding medications and additional procedures such as sperm retrieval or embryo freezing. It’s important to check with individual fertility clinics for exact pricing and available payment options.
10. Can ICSI be used for egg or sperm freezing?
Yes, ICSI can be used in conjunction with egg or sperm freezing (cryopreservation). If the patient wishes to preserve fertility for future use, embryos can be frozen after the ICSI procedure. Similarly, sperm can be frozen and stored before the ICSI process if the male partner is not available for sperm collection on the day of egg retrieval or if sperm quality is a concern.
- Laser Assisted Hatching
- In Vitro Fertilization (IVF)
- Surgical sperm retrival ...etc
- Jindal Heart Institute & Test Tube Baby Centre
- Jinemed Hospital
- Florence Nightingale Group
- Apollo Fertility and IVF Center
- Jaslok Hospital and Research Centre
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



