Surgical sperm retrieval is a procedure used to obtain sperm from men who are unable to produce sperm in their ejaculate, a condition known as azoospermia. This technique is part of assisted reproductive technologies (ART) and is commonly used in conjunction with in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
Surgical sperm retrieval is typically performed when there is an issue that prevents sperm from reaching the ejaculate. This may include blockages in the vas deferens, epididymis, or seminal vesicles, or conditions such as testicular failure, genetic factors, or hormonal imbalances.
Unlike traditional sperm collection through ejaculation, surgical sperm retrieval requires a minor surgical procedure to obtain sperm directly from the testicles or epididymis. There are various techniques available for sperm retrieval, including percutaneous epididymal sperm aspiration (PESA), testicular sperm aspiration (TESA), testicular sperm extraction (TESE), and micro-TESE. The choice of technique depends on the underlying cause of azoospermia and the condition of the testicles.
Surgical sperm retrieval is often used for men who have had a vasectomy, men with congenital absence of the vas deferens (CAVD), or those with blockages or damage to their sperm transport systems.
Surgical sperm retrieval is typically performed in cases of azoospermia, where there is a lack of sperm in the ejaculate. The causes of azoospermia can vary, and some risk factors that may necessitate surgical sperm retrieval include the following:
1. Obstructive Azoospermia:
-
Vasectomy: Men who have undergone a vasectomy, a procedure that cuts or blocks the vas deferens, which is the tube that carries sperm from the testicles to the urethra, may experience obstructive azoospermia. Surgical sperm retrieval allows sperm to be obtained directly from the testicles or epididymis.
-
Congenital Absence of the Vas Deferens (CAVD): Some men are born with a genetic condition that causes the absence of the vas deferens, resulting in azoospermia. In such cases, sperm may still be present in the epididymis, and surgical sperm retrieval can help retrieve it.
-
Infections and Blockages: Infections, such as epididymitis or orchitis, or damage to the vas deferens or epididymis from trauma or surgery, can cause blockages that prevent sperm from reaching the ejaculate. Surgical sperm retrieval is used to bypass these blockages and collect viable sperm.
2. Non-Obstructive Azoospermia:
-
Testicular Failure: In men with non-obstructive azoospermia, the issue lies with sperm production in the testicles rather than a blockage in the transport system. Low sperm count or no sperm production may be the result of genetic disorders (such as Klinefelter syndrome or Y chromosome microdeletions), hormonal imbalances, or testicular injury. In some cases, surgical sperm retrieval can still be used to extract sperm directly from the testicle, particularly with micro-TESE.
3. Genetic and Hormonal Factors:
-
Hormonal Imbalances: Low levels of testosterone or high levels of FSH (Follicle Stimulating Hormone) may impair sperm production in the testicles. Hormonal imbalances are often treated first to improve sperm production, but if sperm is still absent in the ejaculate, surgical sperm retrieval can help.
-
Genetic Conditions: Some genetic conditions can lead to non-obstructive azoospermia. In such cases, sperm may still be present in the testicles or epididymis, making surgical retrieval possible.
Surgical sperm retrieval itself does not produce symptoms, as it is a procedure performed under anesthesia. However, there are certain symptoms or signs related to the underlying causes that may prompt the need for this procedure:
1. Symptoms of Male Infertility (Leading to Surgical Sperm Retrieval):
-
Inability to Conceive: The most common reason men undergo surgical sperm retrieval is the inability to produce sperm in the ejaculate. Couples who have been trying to conceive unsuccessfully for a year or more may be diagnosed with male infertility.
-
Absence of Sperm in Semen: The most obvious symptom prompting surgical sperm retrieval is the absence of sperm in the semen during a semen analysis.
-
Pain or Swelling in the Testicles or Scrotum: Men may experience discomfort or pain in the testicles or scrotum due to conditions such as varicocele, epididymitis, or testicular trauma. These conditions can contribute to infertility and may require surgical sperm retrieval.
-
Sexual Dysfunction: Erectile dysfunction or low libido can sometimes be associated with infertility issues, although these symptoms are more likely to be a result of an underlying hormonal imbalance rather than the need for sperm retrieval.
2. Post-Procedure Symptoms:
-
Mild Discomfort and Swelling: After surgical sperm retrieval, men may experience mild discomfort, swelling, or bruising in the scrotal area. These symptoms are usually temporary and subside within a few days.
-
Spotting or Bleeding: Minor bleeding at the incision site or within the scrotum may occur after the procedure but typically resolves quickly.
-
Infection or Fever: In rare cases, infection or fever may develop following the procedure. It is important to follow post-procedure care instructions to minimize the risk of infection.
Diagnosis of Surgical Sperm Retrieval
The diagnosis for the need for surgical sperm retrieval involves a comprehensive fertility evaluation, which includes both medical history and various diagnostic tests.
1. Semen Analysis:
-
A semen analysis is the first step in diagnosing azoospermia. If sperm are absent in the ejaculate, further tests are performed to determine the underlying cause of infertility.
2. Hormonal and Genetic Testing:
-
Blood tests are conducted to measure hormone levels such as testosterone, FSH, and LH. Abnormal levels may indicate testicular failure or hormonal imbalances that can affect sperm production.
-
Genetic testing is performed to identify any genetic conditions that may be causing azoospermia, such as Klinefelter syndrome or Y chromosome microdeletions.
3. Ultrasound Imaging:
-
A scrotal ultrasound is used to evaluate the testicles, epididymis, and vas deferens for any abnormalities, blockages, or cysts that may affect sperm production or transport.
-
Transrectal ultrasound may be used if a blockage in the seminal vesicles or vas deferens is suspected.
4. Biopsy or Sperm Retrieval Test:
-
In cases of non-obstructive azoospermia, a testicular biopsy may be performed to assess sperm production within the testicle. TESE (testicular sperm extraction) is often performed if sperm is not found in the ejaculate, and TESA or micro-TESE may be considered as well.
Surgical sperm retrieval techniques vary based on the underlying cause of azoospermia and the condition of the testicles or epididymis. Below are the common treatment options used in sperm retrieval:
1. PESA (Percutaneous Epididymal Sperm Aspiration):
-
PESA involves using a fine needle to aspirate sperm directly from the epididymis. This technique is typically used in cases of obstructive azoospermia where sperm production is normal but there is a blockage in the reproductive tract.
2. TESA (Testicular Sperm Aspiration):
-
TESA is a procedure where sperm is aspirated directly from the testicles using a fine needle. It is often used when there is a blockage in the vas deferens or epididymis, but sperm production is normal.
3. TESE (Testicular Sperm Extraction):
-
TESE is a more invasive technique where testicular tissue is surgically removed and examined under a microscope for viable sperm. This procedure is typically used for men with non-obstructive azoospermia, such as those with genetic defects or hormonal imbalances.
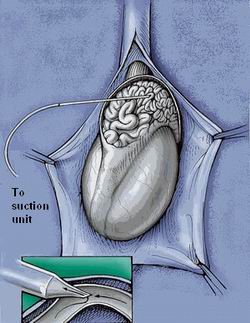
4. Micro-TESE (Microsurgical Testicular Sperm Extraction):
-
Micro-TESE is an advanced procedure performed under microscope guidance to retrieve sperm from the testicles. It is particularly useful for men with severe non-obstructive azoospermia and is associated with a higher sperm retrieval rate compared to traditional TESE.
5. IVF/ICSI:
-
The sperm retrieved from any of these techniques is then used for in vitro fertilization (IVF) or ICSI (intracytoplasmic sperm injection), where a single sperm is injected directly into an egg for fertilization.
While surgical sperm retrieval cannot prevent infertility, there are several management strategies to improve the chances of successful retrieval and subsequent pregnancy:
1. Lifestyle Modifications:
-
Healthy Diet and Exercise: A balanced diet rich in vitamins and antioxidants, along with regular physical activity, can improve overall reproductive health and sperm quality.
-
Avoiding Toxins: Avoid smoking, excessive alcohol consumption, and exposure to environmental toxins, as these can negatively affect sperm production.
2. Managing Underlying Health Conditions:
-
Hormonal Treatment: Hormonal imbalances can be treated with medications to restore normal sperm production, especially in cases of hypogonadism or low testosterone.
-
Surgery for Blockages: In some cases, blockages in the reproductive tract can be surgically corrected, improving the chances of natural conception.
3. Emotional and Psychological Support:
-
Fertility treatments can be emotionally and mentally taxing. Counseling and support groups can help men and couples cope with the emotional challenges of infertility.
While surgical sperm retrieval is generally safe, there are some risks associated with the procedure:
1. Infection:
-
Any surgical procedure carries a risk of infection, especially at the site of needle insertion. Antibiotics may be prescribed to reduce this risk.
2. Bleeding and Bruising:
-
Minor bruising and bleeding at the site of the procedure are common but typically resolve on their own within a few days.
3. Damage to Testicles or Epididymis:
-
While rare, there is a small risk of damage to the testicles or epididymis during the procedure, which could affect future fertility.
4. Low Sperm Retrieval Rates:
-
In cases of non-obstructive azoospermia, there is a possibility that no sperm will be retrieved during the procedure, requiring alternative methods like TESE or micro-TESE.
Living with the need for surgical sperm retrieval can be emotionally challenging, but it provides a chance for men with infertility issues to father biological children. Some key aspects to consider:
1. Psychological Support:
-
Infertility can be stressful for both partners. Psychological counseling and support groups can help individuals and couples cope with the emotional toll of infertility treatments.
2. Future Family Planning:
-
Men who undergo surgical sperm retrieval may want to consider sperm freezing (cryopreservation) for future use, ensuring they have viable sperm stored if they wish to have more children later.
3. Long-Term Fertility:
-
Follow-up evaluations and counseling regarding long-term fertility and family-building options are crucial. This includes assessing the genetic health of sperm and exploring potential genetic counseling if needed.
1. What is Surgical Sperm Retrieval?
Surgical sperm retrieval is a procedure used to collect sperm directly from the male reproductive tract when sperm is absent or low in the ejaculate due to various reasons such as male infertility, obstruction, or absence of the vas deferens. This procedure is typically performed when less invasive sperm collection methods like ejaculation are not possible.
2. Why is Surgical Sperm Retrieval needed?
Surgical sperm retrieval is necessary in cases where:
-
Obstructive azoospermia: Blockages prevent sperm from being released during ejaculation.
-
Congenital absence of the vas deferens: A genetic condition, commonly seen in men with cystic fibrosis.
-
Vasectomy: After a vasectomy, sperm may still be present in the testicles but not in the ejaculate.
-
Failed sperm production: In some cases of male infertility, sperm may need to be retrieved surgically if they are not being ejaculated.
3. How is Surgical Sperm Retrieval performed?
Surgical sperm retrieval is typically performed using one of the following techniques:
-
Testicular Sperm Extraction (TESE): A small sample of tissue is taken directly from the testicle to retrieve sperm.
-
Percutaneous Epididymal Sperm Aspiration (PESA): A needle is used to aspirate sperm directly from the epididymis, the tube where sperm are stored.
-
Micro-epididymal Sperm Aspiration (MESA): A more advanced technique using a microscope to retrieve sperm from the epididymis.
-
Testicular Sperm Aspiration (TESA): Sperm is aspirated from the testicle using a needle.
These procedures are performed under local anesthesia or sedation, depending on the method used.
4. How long does the surgical sperm retrieval procedure take?
The surgical sperm retrieval procedure typically takes about 30 minutes to 1 hour, depending on the technique used. TESE and TESA are minimally invasive and can be completed in a relatively short amount of time, while MESA or PESA may require more precision and can take longer.
5. Is the surgical sperm retrieval procedure painful?
The procedure is generally well-tolerated with the use of local anesthesia, and most patients experience minimal discomfort. Some may feel mild pain or discomfort in the days following the procedure, which can typically be managed with over-the-counter pain medications. Sedation may be used in more complex procedures, reducing the discomfort further.
6. What are the success rates of Surgical Sperm Retrieval?
The success rates of sperm retrieval depend on several factors, including the method used, the cause of infertility, and the overall health of the male partner. In cases of obstructive azoospermia, sperm retrieval success rates can range from 50% to 80%. However, in cases where sperm production is absent or impaired, the success rates may be lower. The retrieved sperm can then be used for in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
7. What are the risks of Surgical Sperm Retrieval?
Surgical sperm retrieval is a relatively safe procedure, but like any surgery, there are some risks, including:
-
Infection: A risk of infection at the incision or puncture site.
-
Bleeding: Some minor bleeding may occur after the procedure.
-
Pain: Mild to moderate pain or discomfort during the recovery period.
-
Damage to surrounding tissue: In rare cases, the sperm retrieval process may cause damage to the testicular tissue or surrounding structures.
The risks are minimal when the procedure is performed by a skilled specialist.
8. How is the sperm used after retrieval?
Once sperm is successfully retrieved, it is assessed for quality and motility. If viable, the sperm is frozen (cryopreserved) for future use or used immediately for assisted reproductive techniques, such as:
-
In vitro fertilization (IVF): The sperm is combined with an egg in a laboratory setting.
-
Intracytoplasmic sperm injection (ICSI): A single sperm is injected directly into the egg to assist with fertilization.
The choice of technique depends on the sperm quality and the specific fertility needs of the couple.
9. Can sperm retrieval be performed after a vasectomy?
Yes, sperm retrieval can be performed after a vasectomy. If a man has had a vasectomy and wants to have children, surgical sperm retrieval techniques such as TESE or PESA can be used to collect sperm directly from the testicles or epididymis. In some cases, men may also consider a vasectomy reversal, but sperm retrieval offers an alternative when a reversal is not an option or does not work.
10. What happens if sperm cannot be retrieved during surgery?
In some cases, sperm may not be successfully retrieved during the procedure, particularly if the male has a condition like non-obstructive azoospermia, where sperm production is absent or very low. If sperm retrieval is unsuccessful, alternative options may include using donor sperm or exploring other methods of sperm retrieval like testicular biopsy. A fertility specialist will discuss the next steps and help determine the best options for the couple.
- Intra Cytoplasmic Sperm Injection (ICSI)
- Testicular Sperm Aspiration (TESA)
- IVF Surrogacy … etc
- Singapore Urology and Fertility Centre
- Jindal Heart Institute & Test Tube Baby Centre
- Lilavati Assisted Conception Unit
- Apollo Fertility and IVF Center
- Yanhee International Hospital
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



