Lung transplantation is a life-saving procedure in which a patient’s diseased or damaged lungs are replaced with healthy donor lungs. This procedure is typically reserved for patients with end-stage lung diseases who no longer respond to other treatments such as medications or oxygen therapy. Lung transplantation offers patients the opportunity to improve their quality of life and potentially extend their lifespan.
Lung transplantation is one of the most complex types of organ transplantation, requiring meticulous planning, surgical expertise, and lifelong care. While lung transplants are not the first-line treatment for lung diseases, they are often considered when other medical therapies and interventions fail to improve the patient's condition.
This surgery is typically performed in specialized transplant centers, with the decision to proceed often based on the patient's eligibility, the severity of their condition, and the availability of a suitable donor lung.
Lung Transplantation Statistics
Lung transplants have been successfully performed since the late 20th century, and outcomes have improved significantly over time. The number of lung transplants performed worldwide has steadily increased, thanks to advances in surgical techniques, post-transplant care, and immunosuppressive medications. According to the International Society for Heart and Lung Transplantation, thousands of lung transplants are performed annually, with varying success rates based on the underlying disease and patient condition.
Lung transplantation is often a treatment of last resort for patients with severe, chronic lung diseases. The need for a transplant typically arises when the lungs are no longer functioning adequately, and the patient is unable to breathe independently. Several conditions can lead to end-stage lung disease, and the causes and risk factors for these diseases vary widely:
Causes of Lung Disease Leading to Transplantation
-
Chronic Obstructive Pulmonary Disease (COPD): COPD is the most common cause of lung transplantation worldwide. It is primarily caused by long-term exposure to harmful substances, such as smoking and air pollution. COPD results in progressive airflow limitation, making breathing difficult.
-
Pulmonary Fibrosis: This condition involves the scarring of lung tissue, which leads to the progressive stiffening of the lungs. It is often idiopathic (of unknown cause), though it can be linked to autoimmune diseases, environmental exposures, or certain medications.
-
Cystic Fibrosis (CF): CF is a genetic disorder that causes thick, sticky mucus to build up in the lungs and other organs, leading to chronic respiratory infections and damage to lung tissue. It is one of the most common indications for lung transplantation in young adults.
-
Pulmonary Hypertension: This condition involves high blood pressure in the arteries of the lungs, leading to heart strain and eventual heart and lung failure. Pulmonary hypertension can result from various underlying conditions, such as left heart disease, lung disease, or blood clots.
-
Alpha-1 Antitrypsin Deficiency: This genetic disorder causes lung damage due to a deficiency in the alpha-1 antitrypsin protein, which helps protect the lungs from damage.
-
Emphysema: A type of COPD, emphysema causes damage to the alveoli (air sacs in the lungs), resulting in difficulty breathing. Emphysema can be caused by smoking or genetic factors.
-
Other Causes: Conditions such as bronchiectasis, interstitial lung diseases, and autoimmune disorders like rheumatoid arthritis and scleroderma can also lead to end-stage lung disease requiring transplantation.
Risk Factors for Lung Disease
-
Smoking: The primary risk factor for COPD, emphysema, and pulmonary fibrosis, smoking significantly damages lung tissue and impairs lung function.
-
Environmental Exposures: Long-term exposure to pollutants, chemicals, dust, or toxins can damage lung tissue and increase the risk of diseases like pulmonary fibrosis and COPD.
-
Family History: A genetic predisposition can contribute to certain lung diseases, such as cystic fibrosis and alpha-1 antitrypsin deficiency.
-
Age: The risk of developing chronic lung diseases increases with age, particularly for diseases like COPD and pulmonary fibrosis.
-
Respiratory Infections: Chronic respiratory infections, such as those caused by bacteria or viruses, can damage the lungs and lead to conditions like bronchiectasis.
Lung diseases that may require a transplant often present with progressive symptoms. Common symptoms include:
-
Shortness of Breath: Difficulty breathing, especially with physical activity, is one of the most common symptoms of advanced lung disease. As the condition worsens, even simple activities may cause significant breathlessness.
-
Chronic Cough: A persistent cough, often accompanied by the production of mucus or phlegm, is common in conditions like COPD and bronchiectasis.
-
Fatigue: Patients with severe lung disease often feel fatigued or exhausted, as the body works harder to get enough oxygen.
-
Chest Pain or Tightness: Some lung conditions can cause discomfort or tightness in the chest, particularly in conditions like pulmonary hypertension or advanced COPD.
-
Wheezing: Wheezing or a high-pitched whistling sound when breathing is common in conditions like asthma and COPD.
-
Cyanosis: A bluish tint to the skin, particularly around the lips and fingertips, indicates low oxygen levels in the blood.
-
Frequent Respiratory Infections: Recurrent pneumonia, bronchitis, or other respiratory infections are common in patients with lung disease, particularly in cystic fibrosis.
Diagnosing the underlying lung disease and determining whether a patient is a suitable candidate for lung transplantation requires a combination of medical evaluations and diagnostic tests:
-
Medical History and Physical Exam: A detailed history of symptoms, past medical conditions, and family history, along with a physical examination, is the first step in diagnosing lung disease.
-
Pulmonary Function Tests (PFTs): These tests measure lung volumes, airflow, and gas exchange to assess how well the lungs are functioning. A decrease in lung capacity or forced expiratory volume (FEV1) is an indication of severe lung impairment.
-
Chest X-Ray and CT Scan: These imaging tests provide detailed images of the lungs and can identify structural abnormalities, scarring, or evidence of infection.
-
Arterial Blood Gas (ABG) Test: This test measures the oxygen and carbon dioxide levels in the blood, which can indicate the severity of lung disease.
-
Bronchoscopy: A procedure where a flexible tube is inserted into the airways to examine the lungs and take tissue samples for biopsy.
-
Lung Biopsy: In some cases, a biopsy may be necessary to confirm the diagnosis of conditions like interstitial lung disease or to evaluate the extent of damage.
-
Heart and Lung Function Tests: Since lung disease can affect the heart, comprehensive assessments of both lung and heart function are necessary.
If conventional treatments fail to improve the patient’s condition, the medical team may consider lung transplantation. A referral to a transplant center is often made for further evaluation and to determine transplant eligibility.
The primary treatment for advanced, end-stage lung disease is lung transplantation. However, other medical and surgical treatments may be used before transplant:
-
Medications: Depending on the condition, medications may be prescribed to manage symptoms and slow disease progression. For example:
-
Inhalers for bronchodilation (COPD, asthma)
-
Corticosteroids and immunosuppressants for inflammatory lung diseases
-
Antibiotics for respiratory infections
-
-
Oxygen Therapy: For patients with low blood oxygen levels, supplemental oxygen therapy is often prescribed to improve breathing and maintain oxygen saturation.
-
Mechanical Ventilation: In cases of severe respiratory failure, a mechanical ventilator may be used to assist with breathing.
-
Ventricular Assist Devices (VADs): In some cases, patients may need mechanical devices to help the heart pump blood while waiting for a transplant.
-
Lung Transplantation: The definitive treatment for end-stage lung disease involves replacing the patient’s diseased lungs with healthy donor lungs. This procedure is typically performed under general anesthesia and requires the patient to be placed on the transplant waiting list until a suitable donor is found.
Preventing and managing lung disease is crucial in reducing the need for a lung transplant:
-
Smoking Cessation: Quitting smoking is the most important step in preventing diseases like COPD and emphysema.
-
Avoiding Environmental Pollutants: Reducing exposure to harmful chemicals, dust, and air pollutants can prevent lung damage and help maintain lung health.
-
Vaccinations: Keeping up with recommended vaccinations, including flu and pneumonia vaccines, can prevent respiratory infections that may worsen lung conditions.
-
Early Detection: Regular check-ups and screenings can help detect lung disease early, allowing for more effective treatment and management.
-
Adherence to Treatment Plans: Strict adherence to prescribed medications and therapies, such as inhalers or oxygen therapy, is essential to managing chronic lung conditions.
Complications of Lung Transplantation
Lung transplantation, while life-saving, comes with potential risks and complications:
-
Rejection of the Donor Lung: The immune system may recognize the transplanted lung as foreign and attempt to reject it. Immunosuppressive drugs are used to prevent rejection.
-
Infections: Due to the need for immunosuppressive medications, patients are more vulnerable to infections, including pneumonia, bronchitis, and viral infections.
-
Chronic Rejection: Over time, some patients may experience chronic allograft dysfunction (CLAD), a condition where the donor lung deteriorates due to rejection.
-
Organ Failure: The use of immunosuppressive drugs can affect other organs, particularly the kidneys and liver, leading to organ dysfunction.
-
Graft Dysfunction: Problems with the transplanted lung itself, such as a failure to properly integrate into the patient’s respiratory system, can occur.
Life after a lung transplant requires careful management to ensure the success of the transplant and to maintain overall health:
-
Immunosuppressive Therapy: To prevent organ rejection, patients must take immunosuppressive medications for the rest of their lives. These drugs help protect the transplanted lung but increase the risk of infections and other complications.
-
Regular Follow-Up Appointments: Continuous monitoring of lung function, medication levels, and overall health is essential for long-term success.
-
Healthy Lifestyle: Maintaining a healthy diet, exercising regularly, and avoiding infections (e.g., by wearing masks in crowded places) are vital for transplant recipients.
-
Mental Health Support: The psychological burden of undergoing a transplant and adjusting to life with a donor lung can be significant. Counseling and support groups can help patients cope.
-
Monitoring for Complications: Patients must remain vigilant for signs of rejection or infection, including changes in breathing patterns, coughing, fever, or fatigue.
1. What is lung transplantation?
Lung transplantation is a surgical procedure in which a patient’s diseased or damaged lungs are replaced with healthy lungs from a donor. The procedure is typically recommended for patients with end-stage lung disease, such as chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, or cystic fibrosis, when other treatments have failed to provide relief.
2. Why is lung transplantation necessary?
Lung transplantation is necessary when the lungs can no longer function effectively due to conditions such as:
-
Chronic obstructive pulmonary disease (COPD): A group of lung diseases that cause airflow obstruction and breathing problems.
-
Pulmonary fibrosis: Scarring of lung tissue, which leads to difficulty breathing.
-
Cystic fibrosis: A genetic condition that causes mucus to build up in the lungs, leading to breathing difficulties and infections.
-
Idiopathic pulmonary hypertension: High blood pressure in the lungs’ arteries that causes strain on the heart and lungs.
-
Other severe lung diseases: Such as emphysema, sarcoidosis, or lung cancer.
A lung transplant helps improve the patient’s ability to breathe and significantly improves their quality of life.
3. What are the types of lung transplants?
There are two primary types of lung transplants:
-
Single lung transplant: One lung is transplanted into the patient, often used for conditions like emphysema or pulmonary fibrosis.
-
Double lung transplant: Both lungs are transplanted, typically used for diseases like cystic fibrosis or pulmonary hypertension where both lungs are severely affected.
In some cases, a heart-lung transplant may be performed if both the heart and lungs are damaged.
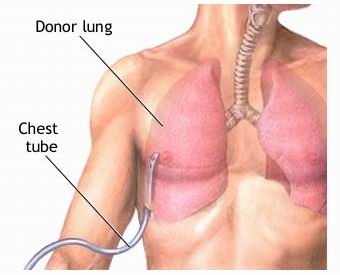
4. How is a lung transplant performed?
Lung transplantation is a major surgery that involves the following steps:
-
Anesthesia: The patient is placed under general anesthesia to ensure they are unconscious and pain-free during the procedure.
-
Incision: A large incision is made in the chest, and the rib cage is temporarily opened to access the lungs.
-
Removal of diseased lungs: The patient’s diseased lungs are carefully removed, and the donor lungs are placed in the chest cavity.
-
Connection: The donor lungs are connected to the patient’s airways and blood vessels.
-
Closure: The incision is closed, and the patient is transferred to the ICU for monitoring.
The procedure typically lasts 4 to 6 hours, and the patient is monitored closely in the hospital for several days after the surgery.
5. Is lung transplantation painful?
Lung transplantation is performed under general anesthesia, so the patient experiences no pain during the surgery. After the procedure, patients may experience some discomfort or pain at the incision site, as well as difficulty breathing initially due to swelling and healing. Pain and discomfort can typically be managed with medication. Patients are closely monitored during recovery, and pain control is a priority.
6. What is the recovery time after lung transplantation?
Recovery after lung transplantation varies by patient, but typically:
-
Initial recovery: Patients stay in the hospital’s ICU for 5 to 10 days to monitor lung function, manage pain, and prevent complications.
-
Short-term recovery: The patient will remain in the hospital for 2 to 3 weeks for continued monitoring and support, including respiratory therapy to help with breathing and lung function.
-
Long-term recovery: Full recovery and rehabilitation can take 6 months to 1 year. Patients will need to adhere to a strict regimen of medications, physical therapy, and regular check-ups.
-
Follow-up care: Regular follow-up visits are essential to monitor the patient’s lung function and to ensure the body is accepting the new lungs.
7. What are the risks and complications of lung transplantation?
Lung transplantation carries several risks and potential complications, including:
-
Rejection: The body’s immune system may attack the transplanted lungs, leading to rejection. Immunosuppressive medications are used to prevent this.
-
Infections: Due to the use of immunosuppressive drugs, patients are more susceptible to infections, particularly in the respiratory system.
-
Chronic rejection: Over time, the transplanted lungs may begin to show signs of chronic rejection, leading to a gradual loss of lung function.
-
Blood clots: There is a risk of blood clots forming in the lungs or blood vessels.
-
Lung function decline: The transplanted lungs may not function as well as expected, requiring further interventions or treatments.
8. How long does a lung transplant last?
The average lifespan of a transplanted lung is around 5 to 10 years, although some patients live much longer with proper care. The longevity of the transplant depends on factors such as the patient’s adherence to medication, overall health, and the quality of the donor lungs. Over time, the transplanted lungs may lose some function, and the patient may require further medical intervention.
9. Will I need to take medications after a lung transplant?
Yes, after a lung transplant, patients must take immunosuppressive medications to prevent their immune system from rejecting the new lungs. These medications suppress the immune response and help the body accept the transplanted lungs. Patients will also need medications to manage other conditions, such as infections or high blood pressure. Long-term use of immunosuppressive drugs requires regular monitoring to adjust dosages and prevent side effects.
10. Can lung transplant recipients lead a normal life?
Yes, many lung transplant recipients can return to a normal life after the recovery period, though it may take time to regain strength and stamina. After transplant recovery, patients are typically able to resume work, exercise, and daily activities. However, they must continue taking medications to prevent rejection, avoid infections, and follow a healthy lifestyle to preserve the health of the new lungs. Regular follow-up care is essential to monitor lung function and ensure the success of the transplant.
The other Organ Transplant Procedures are:
Few Major Hospitals for Lung Transplantation are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


