Liver transplantation is a life-saving surgical procedure in which a diseased or failing liver is replaced with a healthy liver from a donor. The liver plays a critical role in filtering toxins from the blood, producing important proteins, storing energy, and helping with digestion. When the liver becomes severely damaged due to disease or injury, it may no longer be able to perform these functions, leading to liver failure. Liver transplant is often the last treatment option for patients with end-stage liver disease (ESLD) or acute liver failure.
Liver transplantation can offer significant improvements in quality of life, survival rates, and recovery when other treatment options, such as medications or liver support systems, fail. Cirrhosis, hepatitis, and liver cancer are the most common conditions that may require a liver transplant. The donor liver can come from a deceased donor or, in some cases, a living donor (where a portion of the liver is donated by a living individual, usually a close relative).
The success of a liver transplant depends on a variety of factors, including the donor match, the health status of the recipient, and post-transplant care. While liver transplants have a high success rate, they come with significant risks, including graft rejection, infection, and complications from immunosuppressive medications. Lifelong monitoring and careful management are essential for long-term success after a liver transplant.
The need for a liver transplant typically arises from chronic liver disease or acute liver failure, where the liver's function deteriorates to the point that it can no longer meet the body's needs. Below are some of the leading causes and risk factors associated with the need for a liver transplant:
1. Chronic Liver Disease (Cirrhosis)
Cirrhosis is a condition where the liver becomes severely scarred due to long-term damage. This scarring interferes with the liver's ability to function properly. Common causes of cirrhosis include:
-
Chronic alcohol abuse
-
Hepatitis B or Hepatitis C infection
-
Non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH)
-
Autoimmune hepatitis
-
Primary biliary cirrhosis or primary sclerosing cholangitis
-
Wilson’s disease (a genetic disorder leading to copper buildup in the liver)
2. Liver Cancer (Hepatocellular Carcinoma)
Liver cancer, also known as hepatocellular carcinoma (HCC), often develops as a complication of chronic liver diseases such as cirrhosis or chronic hepatitis. HCC is the most common type of liver cancer and is one of the leading reasons for liver transplantation.
3. Acute Liver Failure
Acute liver failure occurs when the liver suddenly loses its ability to function. This can happen within days or weeks and is typically caused by:
-
Acetaminophen (Tylenol) overdose
-
Viral hepatitis (especially hepatitis A and hepatitis B)
-
Drug-induced liver injury from medications or recreational drugs
-
Autoimmune hepatitis
-
Pregnancy-related liver issues, such as acute fatty liver of pregnancy or HELLP syndrome
4. Metabolic Disorders
Certain metabolic diseases can cause liver damage and failure, including:
-
Hemochromatosis (a condition where iron builds up in the body)
-
Alpha-1 antitrypsin deficiency (a genetic disorder affecting liver function)
-
Tyrosinemia (a rare genetic disorder affecting the liver’s ability to break down amino acids)
5. Biliary Atresia (in Children)
Biliary atresia is a condition that occurs in infants where the bile ducts are either absent or blocked, leading to liver damage. This condition is the most common reason for liver transplant in children.
6. Genetic and Inherited Diseases
Some genetic and inherited diseases can lead to liver failure and may require a transplant. These include cystic fibrosis, Alagille syndrome, and Glycogen storage diseases.
7. Obesity and Diabetes
Obesity and type 2 diabetes increase the risk of developing non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH), which can progress to cirrhosis and liver failure. NASH is now a leading cause of liver transplantation.
Liver disease, especially in the case of cirrhosis or liver cancer, often develops gradually over time, and the symptoms may not be noticeable until the disease has advanced. The following signs and symptoms are common in individuals with end-stage liver disease or acute liver failure:
1. Jaundice
Jaundice is characterized by a yellowing of the skin and the whites of the eyes due to the buildup of bilirubin, a byproduct of red blood cell breakdown that the liver usually processes. Jaundice occurs when the liver is unable to metabolize and clear bilirubin effectively.
2. Abdominal Swelling (Ascites)
Ascites is the accumulation of fluid in the abdominal cavity, leading to abdominal swelling. This is a common symptom of liver failure caused by cirrhosis or liver cancer, often accompanied by weight gain and discomfort.
3. Fatigue and Weakness
Fatigue and weakness are common in individuals with liver disease due to the liver’s inability to carry out essential functions, such as detoxification and energy production. Chronic tiredness can become severe in advanced liver disease.
4. Confusion and Cognitive Impairment (Hepatic Encephalopathy)
When the liver is unable to filter toxins from the blood, these toxins can accumulate in the brain, leading to confusion, memory loss, difficulty concentrating, and in severe cases, coma. This condition is known as hepatic encephalopathy.
5. Nausea, Vomiting, and Loss of Appetite
Liver dysfunction can lead to digestive problems, including nausea, vomiting, and a significant loss of appetite. These symptoms are common in individuals with cirrhosis, acute liver failure, or liver cancer.
6. Swollen Legs and Ankles
Due to the liver’s inability to process fluids and maintain proper balance, individuals with liver failure often experience fluid retention, leading to swelling in the legs, ankles, and feet.
7. Dark Urine and Pale Stools
Dark-colored urine and pale or clay-colored stools are often indicative of liver problems. Dark urine occurs due to the buildup of bilirubin, while pale stools may result from a lack of bile reaching the digestive system due to blockages or bile duct damage.
The diagnosis of liver disease and the need for a liver transplant is made after a comprehensive assessment by a liver specialist (hepatologist). The diagnostic process typically includes the following:
1. Physical Examination
A physical exam helps identify visible symptoms of liver disease, such as jaundice, ascites, abdominal tenderness, and swelling in the legs. The doctor may also assess for signs of liver enlargement or liver tenderness.
2. Blood Tests
-
Liver Function Tests: These tests measure the levels of enzymes, proteins, and substances in the blood that indicate liver function. Elevated levels of AST, ALT, bilirubin, and albumin can indicate liver disease.
-
Hepatitis Testing: Blood tests can detect hepatitis viruses (A, B, C) that can cause liver damage.
-
Prothrombin Time: This test measures how well the blood is clotting. A prolonged prothrombin time can indicate liver failure.
3. Imaging Studies
-
Ultrasound: A non-invasive test used to examine the liver’s size, texture, and the presence of tumors or blockages in the liver or bile ducts.
-
CT Scan and MRI: Advanced imaging techniques help assess the extent of liver damage, identify liver cancer, and evaluate the liver’s blood supply.
4. Liver Biopsy
A liver biopsy involves removing a small sample of liver tissue for examination under a microscope. This procedure is used to evaluate the severity of liver damage, determine the cause of liver disease, and help decide if a transplant is necessary.
5. Liver Scoring Systems
Various scoring systems, such as the Model for End-Stage Liver Disease (MELD) score, are used to assess the severity of liver disease and predict the likelihood of survival without a transplant. A higher MELD score typically indicates more severe liver dysfunction and the need for a transplant.
The treatment options for liver disease depend on the underlying cause and the stage of the disease. For individuals with end-stage liver disease, a liver transplant is often the only viable option. Other treatment approaches before a transplant include:
1. Medical Management
For individuals with chronic liver diseases such as hepatitis, cirrhosis, or NAFLD, medications may be used to manage symptoms, slow disease progression, and prevent complications:
-
Antiviral drugs for hepatitis B or C.
-
Diuretics to manage fluid retention.
-
Liver protectants and anti-inflammatory medications to reduce liver damage.
2. Lifestyle Modifications
-
Dietary changes: A low-sodium diet is often recommended to manage fluid retention. Reducing alcohol intake and eating a balanced diet can prevent further liver damage.
-
Weight loss: For those with non-alcoholic fatty liver disease (NAFLD) or NASH, weight loss through diet and exercise can improve liver function.
-
Smoking cessation: Quitting smoking is crucial for preventing further liver damage and improving overall health.
3. Liver Transplantation
When liver disease becomes irreversible and other treatments fail, a liver transplant is considered. The transplant procedure involves removing the diseased liver and replacing it with a healthy donor liver. The patient will need to undergo a series of tests and screenings to ensure compatibility with the donor liver.
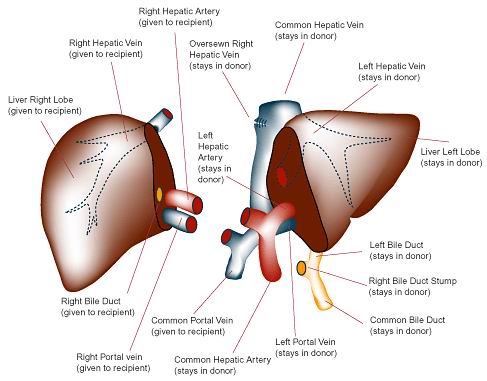
4. Living Donor Liver Transplant
In some cases, a portion of the liver can be donated by a living donor. The donor’s liver regenerates after surgery, and the recipient receives a healthy portion of the liver to restore function. This option is increasingly being used for patients with urgent liver failure.
While liver transplantation is sometimes necessary for end-stage liver disease, there are steps that can help manage liver health and potentially delay the need for a transplant:
1. Prevent Hepatitis
Vaccination and antiviral therapy can help prevent hepatitis infections. Hepatitis B and C are major contributors to cirrhosis and liver failure. Avoiding risky behaviors, such as unprotected sex or sharing needles, can reduce the risk of hepatitis.
2. Manage Risk Factors
Managing conditions like diabetes, hypertension, and obesity can help prevent liver diseases such as NAFLD and NASH. Regular check-ups, a healthy diet, and exercise can help control these risk factors.
3. Regular Liver Monitoring
People with a history of liver disease or those at risk for conditions like cirrhosis should undergo regular liver function tests and imaging studies to monitor liver health and detect any signs of deterioration early.
While liver transplantation is a life-saving procedure, it carries certain risks and complications:
-
Graft rejection: The immune system may attack the transplanted liver, requiring immunosuppressive medications to prevent rejection.
-
Infections: Due to immunosuppressive therapy, transplant patients are at higher risk for infections.
-
Liver damage: The transplanted liver can still develop coronary artery disease, tumors, or other complications over time.
-
Post-transplant diabetes: Some patients may develop new-onset diabetes after transplantation due to the use of immunosuppressive drugs.
Living with a liver transplant requires lifelong monitoring and care:
-
Immunosuppressive medications to prevent rejection of the new liver.
-
Regular medical check-ups to monitor liver function, blood pressure, and the presence of infections.
-
Dietary adjustments, especially low-sodium or low-fat diets, and exercise to maintain health and prevent complications.
-
Emotional support: Coping with the psychological and emotional effects of transplant surgery is vital for overall recovery.
1. What is a liver transplant?
A liver transplant is a surgical procedure in which a diseased or failing liver is replaced with a healthy liver from a donor. The procedure is typically performed when the liver is no longer able to perform its vital functions, often due to conditions such as cirrhosis, liver cancer, or acute liver failure. A liver transplant can significantly improve the patient’s health and quality of life, restoring normal liver function.
2. Why is a liver transplant necessary?
A liver transplant is necessary when the liver has failed or is severely damaged and cannot function properly. Common conditions that may lead to liver failure and require a transplant include:
-
Cirrhosis: Scarring of the liver tissue due to chronic liver disease.
-
Hepatitis: Chronic infection caused by hepatitis B or C.
-
Liver cancer: When cancer develops in the liver.
-
Acute liver failure: Sudden liver dysfunction caused by infections, toxins, or drug overdose.
-
Genetic liver diseases: Such as Wilson’s disease or hemochromatosis.
When the liver is no longer functioning effectively, a transplant is often the best option to restore health and prevent life-threatening complications.
3. What are the types of liver transplants?
There are two main types of liver transplants:
-
Living donor liver transplant: A portion of the liver is donated by a living person, often a relative or close friend. Both the donor and recipient’s liver will regenerate over time.
-
Deceased donor liver transplant: The liver is obtained from a person who has passed away. The transplant is performed when a matching donor is found.
In both cases, the goal is to replace the diseased liver with a healthy one that can function properly.
4. How is a liver transplant performed?
Liver transplantation involves the following steps:
-
Anesthesia: The patient is placed under general anesthesia to ensure they are unconscious during the surgery.
-
Incision: A large incision is made in the abdomen to access the liver.
-
Removal of the diseased liver: The surgeon carefully removes the damaged liver.
-
Implantation of the donor liver: The healthy donor liver is placed into the patient’s body and connected to the major blood vessels and bile ducts.
-
Closure: The incision is closed, and the patient is taken to the intensive care unit (ICU) for close monitoring.
The surgery typically lasts 6 to 8 hours, and the patient stays in the hospital for several days to weeks for recovery.
5. Is a liver transplant painful?
While liver transplant surgery is major surgery and can cause discomfort, it is generally not painful during the procedure because the patient is under general anesthesia. After surgery, patients may experience pain or discomfort at the incision site, along with fatigue, swelling, or bruising. Pain medication and other supportive treatments are provided to manage discomfort during the recovery period.
6. How long does it take to recover from a liver transplant?
The recovery period after a liver transplant can vary, but generally:
-
Immediate recovery: The patient will be closely monitored in the hospital’s ICU for several days, typically 5 to 10 days, to ensure the new liver is functioning properly and to detect any complications.
-
Short-term recovery: Most patients spend 2 to 4 weeks in the hospital after surgery.
-
Long-term recovery: Full recovery can take 6 to 12 months. Patients need to follow a carefully monitored regimen that includes regular check-ups, medications, and dietary adjustments to ensure the success of the transplant and prevent rejection.
During recovery, patients are often advised to gradually return to normal activities and exercise, as their energy levels improve.
7. What are the risks and complications of a liver transplant?
While liver transplantation is a life-saving procedure, there are risks and potential complications, including:
-
Rejection: The body may recognize the new liver as foreign and attempt to reject it. Immunosuppressive medications are prescribed to prevent this.
-
Infection: The immune system is suppressed after the transplant, increasing the risk of infections.
-
Graft failure: The new liver may fail to function properly or may not be fully accepted by the body.
-
Bile duct problems: The bile ducts may become blocked or leak after transplantation.
-
Post-surgical bleeding: This can occur after any surgery.
-
Cancers: Long-term use of immunosuppressive medications may increase the risk of certain cancers, particularly skin cancer.
Your doctor will carefully monitor your health post-transplant to minimize these risks and manage any complications.
8. How long will a liver transplant last?
The average lifespan of a transplanted liver is 10 to 20 years, although it can vary depending on factors such as the quality of the donor liver, the patient’s overall health, and how well the patient follows their post-transplant care plan. With proper care, some patients may live much longer with a transplanted liver. Regular monitoring and adherence to immunosuppressive medications are key to the long-term success of the transplant.
9. Will I need to take medications after a liver transplant?
Yes, after a liver transplant, patients must take immunosuppressive medications to prevent the body from rejecting the new liver. These medications suppress the immune system to ensure the new organ is accepted. Patients will also need medications to manage other aspects of their health, such as controlling blood pressure, cholesterol, and preventing infections. Long-term use of these medications requires careful monitoring to prevent side effects and ensure the transplant remains successful.
10. Can I lead a normal life after a liver transplant?
Yes, most patients can return to a normal, active life after a liver transplant, though it may take time to fully recover. After the transplant, patients typically regain their energy levels, and many can resume their work, exercise, and other daily activities. However, they will need to maintain a healthy lifestyle, follow their doctor’s recommendations, and take medications regularly to ensure the new liver remains healthy and functional. Patients should also avoid alcohol and any activities that could put stress on the liver or immune system.
The other Organ Transplant Procedures are
Few Major Hospitals for Liver Transplantation are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


