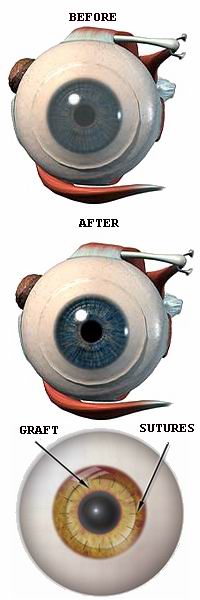
Corneal transplantation, also known as a corneal graft or keratoplasty, is a surgical procedure in which a damaged or diseased cornea is replaced with a healthy donor cornea. The cornea is the clear, dome-shaped surface at the front of the eye that plays a crucial role in focusing light and enabling clear vision. When the cornea becomes cloudy, scarred, or damaged due to conditions such as corneal dystrophies, infections, trauma, or certain eye diseases, it can severely impair vision. In cases where conservative treatments like medications or corrective lenses are no longer effective, a corneal transplant may be recommended.
During the procedure, the surgeon removes the affected portion of the cornea and replaces it with the donor tissue, which is secured using sutures. The donor cornea is carefully matched for size, shape, and other characteristics to ensure compatibility with the patient’s eye. Corneal transplantation is often performed under local anesthesia, with patients being awake but numb during the procedure. The success of the transplant depends on various factors, including the health of the eye, the underlying condition being treated, and the patient's adherence to post-operative care.
After surgery, patients may experience improved vision, although the recovery process can take several months as the cornea heals and adjusts. The procedure is considered safe and effective, with high success rates in restoring vision and improving the quality of life for individuals with corneal damage. However, long-term care, including the use of eye drops and regular follow-ups with an ophthalmologist, is essential to ensure the transplant remains successful and to monitor for potential complications, such as rejection of the donor tissue.
Corneal transplantation is typically performed when the cornea is severely damaged or diseased, and conventional treatments (glasses, contacts, or medication) have failed. Several conditions can lead to the need for a corneal transplant:
Causes of Corneal Transplantation:
-
Corneal Diseases:
-
Keratoconus: A condition in which the cornea becomes thin and bulges into a cone shape, leading to blurred or distorted vision. In advanced cases, a transplant may be required to restore clear vision.
-
Fuchs' Dystrophy: A progressive disorder affecting the corneal endothelium, leading to corneal swelling, cloudiness, and vision impairment. If untreated, a corneal transplant is often necessary to restore vision.
-
Stromal Dystrophies: Inherited disorders that cause deposits in the stroma (the middle layer of the cornea), leading to scarring and opacity. This can interfere with vision and necessitate a corneal transplant.
-
-
Trauma or Injury:
-
Corneal trauma, such as lacerations, chemical burns, or foreign body injuries, can severely damage the cornea, leading to scarring and permanent vision loss. In such cases, corneal transplantation may be the only option for restoring vision.
-
Corneal ulcers resulting from infections can also lead to permanent corneal damage. Severe infections like bacterial keratitis or herpes simplex keratitis can cause significant scarring and loss of vision, requiring a transplant.
-
-
Corneal Scarring:
-
Corneal scarring, resulting from injury or chronic eye conditions, can lead to blurred vision and reduced light transmission. Patients with extensive scarring may require a transplant to restore visual clarity.
-
-
Endothelial Cell Dysfunction:
-
The endothelial cells in the innermost layer of the cornea maintain its transparency by pumping fluid out of the cornea. Diseases like Fuchs' dystrophy and pseudophakic bullous keratopathy can lead to endothelial cell failure, causing the cornea to swell and become cloudy. When conservative treatments fail, a transplant may be necessary.
-
-
Genetic Conditions:
-
Inherited conditions such as thalassemia or sickle cell disease can cause corneal damage and require transplant surgery. Additionally, some inherited forms of keratoconus may worsen over time and necessitate corneal replacement.
-
-
Previous Eye Surgery:
-
Certain complications following cataract surgery, particularly those involving damage to the corneal endothelium, may require corneal transplantation if the cornea becomes cloudy or swollen. Glaucoma surgery can also result in complications that may necessitate a transplant.
-
-
Infections and Inflammation:
-
Infections of the eye, particularly if they involve the cornea, can lead to corneal scarring. Chronic inflammation or autoimmune diseases such as rheumatoid arthritis can also damage the cornea, potentially requiring a transplant.
-
Risk Factors for Corneal Transplantation:
-
Age:
-
Older adults are more likely to suffer from Fuchs' dystrophy and other age-related corneal issues that require transplantation.
-
-
Family History:
-
A family history of corneal diseases, such as keratoconus or Fuchs' dystrophy, can increase the risk of needing a transplant.
-
-
Eye Trauma:
-
Those who have suffered severe eye injuries are at increased risk for corneal damage that could lead to a transplant.
-
-
Systemic Health Conditions:
-
Conditions such as diabetes, autoimmune diseases, and vascular diseases can increase the risk of corneal damage. For instance, diabetic retinopathy and high blood pressure can damage the retina and cornea.
-
-
Infection:
-
Chronic or severe eye infections, particularly bacterial or viral infections, can lead to permanent damage to the cornea.
-
The need for corneal transplantation arises when a patient's cornea becomes damaged or diseased, leading to significant vision impairment. Common symptoms and signs that indicate the need for a transplant include:
1. Blurred Vision:
-
Cloudy or blurry vision is the most common symptom of corneal disease. The cornea's role in focusing light is compromised when it becomes opaque or scarred.
2. Sensitivity to Light (Photophobia):
-
Increased light sensitivity occurs when the cornea becomes cloudy, making it difficult for the eye to focus light properly. This can be especially problematic in bright environments.
3. Distorted Vision:
-
People with keratoconus or corneal scarring often experience distorted vision, where straight lines appear wavy or images are doubled. This can severely affect daily activities like reading or driving.
4. Eye Pain or Discomfort:
-
Pain or irritation in the eye may result from corneal injury, infections, or endothelial dysfunction. In severe cases, the pain can be constant and debilitating.
5. Decreased Night Vision:
-
Poor vision in low-light conditions is often a sign of corneal damage. The clouding of the cornea interferes with the light entering the eye, making it harder to see in dim light.
6. Recurrent Eye Infections:
-
Individuals with corneal ulcers or persistent eye infections may experience recurring pain, redness, and discharge, which can damage the cornea and require surgical intervention.
The diagnosis of corneal transplantation need begins with a thorough clinical evaluation and diagnostic tests to assess the health of the cornea.
1. Visual Acuity Test:
-
This standard eye test measures the clarity of a patient’s vision. A decrease in visual acuity may suggest that the cornea is no longer functioning properly and a transplant may be needed.
2. Slit-Lamp Examination:
-
The slit-lamp allows the ophthalmologist to examine the cornea and other parts of the eye in detail. This examination can help detect cloudiness, scarring, or corneal thinning, which are indications for transplant surgery.
3. Corneal Topography:
-
Corneal topography is used to map the curvature of the cornea. This test helps diagnose conditions like keratoconus, which can lead to corneal transplantation if left untreated.
4. Pachymetry:
-
Pachymetry measures the thickness of the cornea. Corneal thickness can affect the healing process after surgery and can be an indicator of corneal disease, such as Fuchs’ dystrophy.
5. Fluorescein Dye Test:
-
The fluorescein dye test involves applying a special dye to the eye, which highlights any damage or scarring on the cornea. This test is especially useful for detecting corneal ulcers or areas of decreased transparency.
Corneal transplantation is typically recommended for patients with severe corneal damage. The type of transplant performed will depend on the condition of the cornea and the underlying disease.
1. Penetrating Keratoplasty (PK):
-
Penetrating keratoplasty is the traditional method of corneal transplantation. It involves removing the entire thickness of the cornea and replacing it with a donor cornea. This type of transplant is typically used when the entire cornea is affected by disease or injury.
2. Lamellar Keratoplasty:
-
Lamellar keratoplasty involves the partial replacement of the cornea, either the outer layers or inner layers, depending on the disease. Deep anterior lamellar keratoplasty (DALK) and Descemet’s membrane endothelial keratoplasty (DMEK) are common techniques for treating specific types of corneal disease, such as Fuchs’ dystrophy or keratoconus.
3. Descemet’s Membrane Endothelial Keratoplasty (DMEK):
-
DMEK is a modern technique that replaces the innermost layer of the cornea, known as the Descemet’s membrane and the endothelial layer. This is typically used for patients with Fuchs’ dystrophy or corneal endothelial dysfunction.
4. Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK):
-
DSAEK is a newer form of endothelial keratoplasty, where a thin layer of corneal tissue is replaced. It provides faster recovery and fewer complications than traditional penetrating keratoplasty.
While certain causes of corneal disease cannot be prevented, the following measures can help manage risk factors and improve the likelihood of a successful corneal transplant:
1. Regular Eye Exams:
-
Early detection is essential for preventing corneal disease. Individuals with a family history of corneal disorders or those at risk for eye trauma should have regular eye exams to monitor eye health.
2. Protecting the Eyes from Injury:
-
Wearing protective eyewear during activities like sports or construction work can prevent corneal injuries and reduce the risk of requiring a transplant.
3. Managing Underlying Conditions:
-
Individuals with diabetes, autoimmune diseases, or high blood pressure should keep these conditions well-controlled to avoid corneal complications.
4. Post-Transplant Care:
-
After a corneal transplant, patients must adhere to prescribed medications, including immunosuppressive drugs to prevent graft rejection. Antibiotics and anti-inflammatory medications are often prescribed to prevent infections and reduce inflammation.
Like any surgery, corneal transplantation carries some risk of complications. Some of the potential complications include:
1. Graft Rejection:
-
The most significant complication of corneal transplant surgery is graft rejection. The body may recognize the donor tissue as foreign and attempt to reject it. Immunosuppressive medications are used to minimize this risk.
2. Infection:
-
Infections can occur after surgery, leading to graft failure. Prompt treatment with antibiotics can help reduce the risk of infection.
3. Elevated Intraocular Pressure (IOP):
-
Some patients may experience increased IOP, which can lead to glaucoma. Regular monitoring of eye pressure is essential for detecting and managing this condition.
4. Cataract Formation:
-
Cataracts may form after a corneal transplant, especially in older adults. In some cases, cataract surgery may be necessary after the transplant.
After undergoing a corneal transplant, patients need to follow a strict regimen to ensure proper healing and avoid complications:
1. Post-Surgical Care:
-
Eye drops to prevent infection and inflammation, as well as shielding the eye while sleeping, are common post-surgery recommendations. Patients may also be asked to wear protective eyewear to avoid injury.
2. Follow-Up Appointments:
-
Regular follow-up visits are crucial to monitor the healing process and ensure the graft is not rejected. During these visits, vision tests, corneal mapping, and other assessments will be done.
3. Lifestyle Changes:
-
After corneal transplantation, it’s important to avoid activities that can put strain on the eyes, such as heavy lifting or rubbing the eyes. Patients should also be cautious with sun exposure and wear UV-blocking sunglasses.
4. Long-Term Care:
-
Patients will need regular monitoring to ensure that the graft remains clear and to detect any signs of rejection. Good eye care practices and maintaining overall eye health are essential for the long-term success of the transplant.
1. What is corneal transplantation?
Corneal transplantation, also known as corneal graft surgery, is a procedure in which a damaged or diseased cornea (the clear, dome-shaped surface of the eye) is replaced with a healthy donor cornea. The goal of corneal transplantation is to restore vision, reduce pain, and improve the overall function of the eye when the cornea becomes cloudy or scarred due to disease, injury, or genetic conditions.
2. Why is corneal transplantation necessary?
Corneal transplantation is necessary when the cornea becomes damaged, diseased, or scarred, leading to blurred vision, pain, or even blindness. Conditions that may require a corneal transplant include:
-
Keratoconus: A condition where the cornea becomes thin and cone-shaped.
-
Corneal scarring: Caused by injury, infection, or previous surgeries.
-
Fuchs' dystrophy: A condition that affects the corneal endothelium (inner layer), leading to corneal swelling and clouding.
-
Corneal edema: Swelling in the cornea, often caused by an endothelial dysfunction.
-
Infections: Such as herpes simplex virus or fungal infections that damage the cornea.
3. What are the different types of corneal transplants?
There are several types of corneal transplants, depending on which part of the cornea is replaced:
-
Penetrating Keratoplasty (PKP): In this procedure, the entire thickness of the cornea is replaced with a donor cornea.
-
Lamellar Keratoplasty: Only the outer layers of the cornea are replaced, while the deeper layers remain intact. This is typically done for conditions like keratoconus or corneal scars.
-
Descemet’s Stripping Endothelial Keratoplasty (DSEK): This procedure involves replacing only the inner layers of the cornea (Descemet’s membrane and the endothelium), commonly used for endothelial dysfunction such as Fuchs’ dystrophy.
-
Descemet’s Membrane Endothelial Keratoplasty (DMEK): A more advanced form of DSEK where only the Descemet's membrane and endothelial cells are transplanted.
4. How is corneal transplantation performed?
Corneal transplantation is performed under local anesthesia with sedation. The procedure typically involves the following steps:
-
Preparation: The patient is given numbing eye drops and sedatives to ensure comfort during the surgery.
-
Incision: The surgeon makes a small incision in the cornea.
-
Removal of damaged cornea: The diseased or damaged corneal tissue is removed.
-
Donor cornea placement: A donor cornea is carefully stitched into place to replace the removed tissue.
-
Closure: The incision is closed with fine sutures, and the eye is bandaged to protect it.
The surgery usually takes about 1-2 hours, and it is typically done on an outpatient basis.
5. Is corneal transplantation painful?
Corneal transplantation is not painful during the surgery because the eye is numbed with local anesthesia. After the surgery, some patients may experience mild discomfort, a foreign body sensation, or mild pain, but this is usually manageable with prescribed pain relief and anti-inflammatory eye drops. It is important to follow post-operative care instructions to minimize discomfort and promote healing.
6. How long does it take to recover from corneal transplantation?
The recovery time after corneal transplantation can vary, but generally:
-
First few days: Mild discomfort, blurry vision, and sensitivity to light are common. Patients are given medications to manage pain and prevent infection.
-
1-2 weeks: Most patients can resume normal activities, though they should avoid strenuous physical activity and rubbing their eyes.
-
1 month: Vision begins to stabilize, though it may still fluctuate as the eye heals.
-
3-12 months: Full recovery and final vision results can take several months. It may take up to a year for the eye to fully heal and for vision to stabilize.
Regular follow-up visits with the ophthalmologist are essential to monitor healing and ensure there are no complications.
7. What are the risks and complications of corneal transplantation?
Like any surgical procedure, corneal transplantation carries some risks, including:
-
Rejection: The body may reject the donor cornea, leading to inflammation and potential loss of vision. Anti-rejection medications are used to prevent this.
-
Infection: Post-surgical infections can occur, although they are rare.
-
Glaucoma: Elevated intraocular pressure can develop, leading to glaucoma.
-
Cataract formation: Some patients may develop cataracts after surgery.
-
Graft failure: In rare cases, the donor cornea may fail or the transplant may not "take."
-
Scarring: The cornea may form scarring after the transplant, which can affect vision.
Your surgeon will carefully monitor you during the recovery period to minimize risks and complications.
8. How successful is corneal transplantation?
Corneal transplantation is generally a highly successful procedure, with a success rate of 85-90% for the graft remaining clear and functional after one year, especially in patients with no underlying systemic conditions. The success rate can vary depending on the type of transplant, the patient’s general health, and the presence of conditions like glaucoma, diabetes, or previous eye surgeries.
9. Will I need glasses or contact lenses after corneal transplantation?
Most patients will require some form of vision correction after corneal transplantation, especially during the initial recovery phase when vision may be blurry. Over time, as the eye heals and stabilizes, vision may improve, and some patients may not need glasses or contact lenses. However, many people will still need glasses or contact lenses for tasks like reading or driving, depending on the degree of visual recovery and the type of corneal transplant performed.
10. How can I prevent complications after corneal transplantation?
To prevent complications after corneal transplantation:
-
Follow-up care: Regular follow-up visits with your ophthalmologist are essential to monitor healing, check for graft rejection, and manage any potential complications.
-
Medication adherence: Take all prescribed medications, including anti-rejection eye drops, exactly as directed by your doctor.
-
Protect your eye: Avoid rubbing the eye or engaging in activities that may put strain on the healing cornea. Wear an eye shield at night for protection.
-
UV protection: Protect your eyes from UV light by wearing sunglasses with UV protection, as UV exposure can harm the transplanted cornea.
By closely following your ophthalmologist's instructions, you can help ensure the success of the transplant and reduce the risk of complications.
The other Organ Transplant Procedures are:
Few Major Hospitals for CABG are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals Cabg | Doctors For Cabg | Surgeons For Cabg | Surgery Cabg | Cost Of Cabg | Treatment Cabg | Destinations For Cabg | Cabg In India | Recovery Cabg | Cabg Information | Cabg In Thailand | Cabg In Malaysia | Cabg In Singapore | Cabg | Coronary Artery Bypass Surgery | Heart Bypass | Bypass Surgery | Congenital Heart Disease | Cardiothoracic Surgery | Blockage Of Arteries | Cardiopulmonary Bypass | Off-Pump Surgery | Coronary Artery | Double Heart Bypass Surgery | Triple Heart Bypass Surgery | Cad | Coronary Artery Bypass Grafting | Cardiology | Risks Of Cabg | Cabg In Apollo Hospitals | Cabg Overseas | Cabg Low Cost | Cabg In Wockhardt Hospitalssurgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



