Cervical Discectomy is a surgical procedure used to treat spinal conditions affecting the cervical spine (the neck region). The surgery involves the removal of a damaged or herniated intervertebral disc in the cervical spine. This procedure is typically performed to relieve pressure on the spinal cord or nerve roots, which can result in chronic pain, numbness, or weakness in the arms and hands.
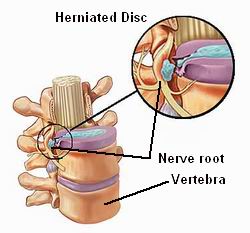
The cervical spine consists of seven vertebrae, separated by intervertebral discs that act as cushions and provide flexibility. Over time, these discs can become damaged or herniated due to injury, aging, or degenerative conditions. When this happens, it may cause nerve compression, resulting in pain or neurological symptoms.
Cervical discectomy is often recommended when non-surgical treatments like physical therapy, medications, or injections are ineffective in providing relief from pain or restoring function. It can be performed using various techniques, including anterior cervical discectomy (approaching from the front of the neck) or posterior cervical discectomy (approaching from the back), depending on the location and severity of the disc problem.

Cervical discectomy is commonly required for conditions that involve damage to the intervertebral discs, which are the shock-absorbing cushions between the vertebrae. The most common causes and risk factors for needing cervical discectomy include:
1. Degenerative Disc Disease
As we age, the intervertebral discs begin to lose their moisture content and elasticity, leading to a breakdown known as degenerative disc disease. This condition can cause discs to flatten or bulge, resulting in nerve compression and pain.
2. Herniated Disc
A herniated disc occurs when the nucleus pulposus (the inner gel-like substance of the disc) pushes through the annulus fibrosus (the outer layer) and presses against nearby nerves or the spinal cord. This herniation often results in pain, numbness, and weakness in the neck, arms, or hands.
3. Spinal Stenosis
Spinal stenosis is a condition where the spinal canal becomes narrowed, compressing the spinal cord or nerve roots. This narrowing can be caused by disc degeneration, bone spurs, or thickened ligaments and can lead to pain, numbness, and weakness in the arms, neck, or legs.
4. Trauma or Injury
Injury to the neck or spine, such as from a car accident, fall, or sports injury, can lead to damage or herniation of the cervical discs. If the damage causes nerve compression or significant pain, surgery may be necessary.
5. Risk Factors
Certain factors can increase the risk of needing cervical discectomy:
-
Age: As people age, the likelihood of disc degeneration and herniation increases.
-
Occupation or Activities: Jobs or hobbies that involve heavy lifting, repetitive motion, or prolonged sitting can strain the neck and contribute to disc problems.
-
Genetics: Family history can play a role in disc degeneration and herniation, with some individuals being genetically predisposed to these conditions.
-
Smoking: Smoking reduces blood flow to the discs, impairing their ability to heal and increasing the risk of degeneration.
Cervical spine issues that require discectomy usually present with a range of symptoms that affect the neck, arms, and hands. The symptoms can vary depending on the severity of the condition and the location of the damaged disc.
1. Neck Pain
The most common symptom of cervical disc issues is neck pain, which can range from mild to severe. This pain can be continuous or intermittent and may worsen with certain movements such as bending the neck forward or turning the head.
2. Radiating Pain in the Arms
When a herniated disc presses on the nerves, it can cause pain to radiate down into the arms, shoulders, and hands. This pain is often described as shooting, burning, or electric shock-like and can be accompanied by numbness and tingling.
3. Numbness and Tingling
Nerve compression can lead to paresthesia (numbness or tingling) in the hands, fingers, or arms. The sensation may feel like pins and needles or complete loss of sensation in the affected areas.
4. Weakness in the Arms or Hands
If the nerves responsible for muscle control in the arms or hands are compressed, it can lead to muscle weakness. This can make activities like gripping objects, lifting items, or even writing difficult.
5. Loss of Reflexes
Compression of the spinal nerves can result in diminished reflexes in the arms or hands, making it harder for your body to react to certain stimuli. This may manifest as a reduced or absent reflex in the biceps or triceps during a physical exam.
6. Difficulty in Walking or Balance Issues
In severe cases, cervical disc problems can affect the spinal cord, leading to problems with coordination and walking. Patients may feel unsteady or have difficulty maintaining balance, especially when walking or standing for extended periods.
To determine whether cervical discectomy is the appropriate treatment, a thorough diagnostic process is necessary. The goal of the diagnosis is to understand the root cause of the pain, the condition of the disc, and whether nerve compression is present.
1. Medical History
Your healthcare provider will begin by reviewing your medical history and symptoms. They will ask detailed questions about the nature of your pain, its location, how it started, and how it changes with different movements or activities.
2. Physical Examination
The doctor will conduct a physical exam to assess your neck, arms, and reflexes. This exam may include muscle strength tests, nerve sensation assessments, and range of motion evaluations to help identify the areas affected by the cervical spine issue.
3. Imaging Tests
-
X-rays: X-rays help evaluate the alignment of the spine, bone structure, and any visible signs of disc degeneration or abnormalities. However, they do not provide detailed images of soft tissues like discs or nerves.
-
MRI (Magnetic Resonance Imaging): MRI is the most effective test for evaluating soft tissues, such as discs, nerves, and spinal cord. MRI can reveal the extent of disc herniation, nerve compression, and spinal cord involvement.
-
CT Scan (Computed Tomography): A CT scan may be used to create detailed images of the bone structure in the cervical spine. It’s often used when further clarification of the spine’s condition is needed.
-
Electromyography (EMG): EMG tests the electrical activity of muscles and nerves. This test is used to identify nerve damage and to determine whether the nerve compression is causing muscle weakness.
Once a diagnosis is made, the treatment plan for cervical disc issues can include both non-surgical and surgical options. The primary goal of treatment is to relieve pain, restore function, and prevent further damage to the spine or nerves.
1. Non-Surgical Treatments
Before considering surgery, a variety of conservative treatments are typically attempted:
-
Physical Therapy: A targeted physical therapy program can help strengthen the muscles around the spine, improve flexibility, and relieve pain.
-
Medications: Over-the-counter NSAIDs (nonsteroidal anti-inflammatory drugs) or muscle relaxants can help manage pain and inflammation. If pain persists, oral steroids or epidural steroid injections may be recommended to reduce inflammation.
-
Cervical Collar: Wearing a cervical collar can provide support for the neck and limit movement, helping to reduce pain and promote healing in the short term.
-
Chiropractic Care: In some cases, chiropractic adjustments may help alleviate discomfort caused by misalignments or restrictions in the cervical spine.
2. Surgical Treatment: Cervical Discectomy
When conservative treatments fail to provide relief, Cervical Discectomy may be recommended. This procedure involves the removal of the damaged disc to relieve pressure on the spinal cord or nerves. The surgery can be done using different techniques:
-
Anterior Cervical Discectomy: This is the most common approach, where the surgeon removes the disc from the front of the neck. This approach provides excellent access to the disc space.
-
Posterior Cervical Discectomy: In some cases, the surgeon may approach the cervical spine from the back to remove the disc, especially if there is an issue with the spinal cord.
-
Fusion: After removing the disc, the surgeon may perform a cervical fusion, which involves joining the adjacent vertebrae to stabilize the spine. Alternatively, an artificial disc replacement may be performed to maintain motion.
3. Post-Surgical Rehabilitation
After surgery, physical therapy is often recommended to help patients regain strength, improve flexibility, and restore mobility. Patients may need to wear a cervical collar for a period of time and avoid certain movements to protect the spine as it heals.
While some risk factors for cervical spine issues cannot be avoided, there are several steps you can take to reduce the likelihood of needing cervical discectomy surgery.
1. Maintain Proper Posture
Good posture is essential for preventing cervical spine issues. Avoid slouching, and ensure that your work and sleep positions support your neck’s natural alignment.
2. Exercise Regularly
Regular exercise, especially neck and back strengthening exercises, can improve spinal health and reduce the risk of disc degeneration. Activities like swimming, walking, and strength training can help maintain a healthy spine.
3. Healthy Weight Management
Excess weight places added pressure on the spine, increasing the risk of developing disc problems. Maintaining a healthy weight reduces this strain and promotes overall spinal health.
4. Avoid Heavy Lifting
Improper lifting techniques can strain the cervical spine. Always use proper lifting techniques, keeping the back straight and using the legs to lift, rather than bending at the waist.
5. Quit Smoking
Smoking impairs blood flow to the spine, hindering the healing process and accelerating disc degeneration. Quitting smoking can help protect the health of the spine and improve recovery from surgery.
Like any surgery, cervical discectomy comes with potential risks and complications. These include:
1. Infection
Infection at the surgical site is a rare but serious complication. Patients are given antibiotics during and after surgery to reduce the risk of infection.
2. Nerve Damage
Though uncommon, nerve damage can occur during surgery, leading to persistent pain, numbness, or weakness.
3. Blood Clots
As with any major surgery, there is a risk of blood clots. To reduce this risk, patients are encouraged to move and walk as soon as possible after surgery.
4. Non-Union
In some cases, the bones may not fuse properly after surgery, leading to a condition known as pseudoarthrosis. This may require additional surgery.
After cervical discectomy surgery, patients can expect significant relief from symptoms like pain and numbness. However, the recovery process requires patience and adherence to rehabilitation guidelines.
1. Post-Operative Care
Patients should follow post-surgical instructions, including wearing a neck brace or collar, taking prescribed medications, and attending follow-up appointments to monitor progress.
2. Long-Term Spine Care
Maintaining a healthy spine after surgery involves continuing with physical therapy, managing body weight, practicing good posture, and avoiding activities that could strain the neck.
3. Emotional Support
Coping with chronic pain and recovery after surgery can take an emotional toll. Support from loved ones, counseling, or joining a support group can help manage the emotional challenges associated with surgery.
1. What is cervical discectomy?
Cervical discectomy is a surgical procedure performed to remove a damaged or herniated disc in the cervical (neck) region of the spine. The procedure is done to relieve pressure on the spinal cord or nerves caused by the disc. A herniated disc can cause pain, numbness, or weakness in the neck, arms, or hands. The surgeon removes part or all of the disc to alleviate these symptoms and restore normal function.
2. Why is cervical discectomy performed?
Cervical discectomy is performed to treat conditions such as:
-
Herniated disc: When the inner gel-like portion of a disc bulges out, pressing on nearby nerves or the spinal cord.
-
Degenerative disc disease: The wear and tear of discs over time, leading to pain and dysfunction.
-
Spinal stenosis: Narrowing of the spinal canal, which puts pressure on the spinal cord or nerves.
-
Radiculopathy: Nerve compression caused by a herniated disc, leading to symptoms such as pain, numbness, or weakness in the arm.
The goal of cervical discectomy is to relieve pressure on the spinal cord or nerves and improve symptoms like pain and numbness.
3. How is cervical discectomy performed?
Cervical discectomy is typically performed under general anesthesia. The surgeon makes a small incision in the front of the neck (anterior approach) to access the cervical spine. Once the disc is located, the damaged or herniated portion is removed, decompressing the affected nerve or spinal cord. In some cases, the surgeon may also remove the entire disc. After the disc removal, the spine may be stabilized with a bone graft or fusion, depending on the extent of the disc removal.
4. What are the benefits of cervical discectomy?
The benefits of cervical discectomy include:
-
Pain relief: The primary benefit is relief from neck, arm, or hand pain caused by a herniated or degenerated disc.
-
Improved mobility: By removing the source of pressure on the nerves or spinal cord, patients often experience increased mobility and reduced stiffness.
-
Restoration of function: For patients suffering from weakness or numbness in the arms or hands, cervical discectomy can help restore nerve function and improve strength.
5. How long does it take to recover from cervical discectomy?
Recovery time from cervical discectomy varies depending on the individual and the type of procedure performed. Generally, patients can expect the following:
-
Hospital stay: Most patients stay in the hospital for 1 to 2 days after the surgery.
-
Initial recovery: You may need to avoid heavy lifting and activities that strain the neck for 4 to 6 weeks.
-
Full recovery: Full recovery, including the return to more strenuous activities, may take 2 to 3 months. Some patients may also need physical therapy to improve range of motion and strength in the neck.
Your surgeon will provide specific instructions and a rehabilitation plan to optimize recovery.
6. Are there any risks or complications with cervical discectomy?
Like any surgery, cervical discectomy carries some risks, including:
-
Infection: Although rare, infection at the surgical site can occur.
-
Nerve injury: There's a small risk of nerve damage, which could lead to weakness, numbness, or loss of function.
-
Spinal cord injury: In rare cases, damage to the spinal cord could occur during surgery, which may affect motor or sensory functions.
-
Cerebrospinal fluid (CSF) leak: A CSF leak is rare but may happen if the dural sac surrounding the spinal cord is damaged.
-
Failed disc removal: If the disc is not fully removed or if the procedure is unsuccessful, symptoms may not improve.
-
Recurrence of disc herniation: The same or adjacent discs may experience further degeneration in the future.
Your surgeon will discuss these risks and take steps to minimize them during the procedure.
7. Will I need a spinal fusion after cervical discectomy?
In some cases, a spinal fusion is performed after cervical discectomy, particularly if the entire disc is removed or if the spine needs stabilization. The procedure involves using a bone graft or artificial material to fuse the adjacent vertebrae together, promoting bone healing. This helps to stabilize the spine and prevent movement at the operated level. However, not all patients require fusion. In some cases, the spine may remain stable without the need for fusion, depending on the extent of the disc removal and the patient's overall spinal health.
8. How soon can I return to work after cervical discectomy?
The timeline for returning to work depends on the nature of your job and your recovery progress. Most people can return to desk jobs or light activities within 1 to 2 weeks. However, for jobs that require physical labor or heavy lifting, it may take 4 to 6 weeks before returning to work. Your surgeon will provide guidance on when it is safe to return to work based on your recovery.
9. Can cervical discectomy help with neck pain and arm numbness?
Yes, cervical discectomy can effectively relieve neck pain and arm numbness caused by nerve compression from a herniated or degenerated disc. By removing the damaged disc and decompressing the nerve, the procedure can help reduce inflammation and restore normal nerve function. Most patients experience significant improvement in pain and numbness following the surgery.
10. How much does cervical discectomy surgery cost?
The cost of cervical discectomy surgery can vary based on factors such as the hospital or surgical center, geographic location, and whether a spinal fusion is required. On average, the cost for cervical discectomy surgery ranges from $15,000 to $50,000, including the surgeon’s fee, hospital stay, and follow-up care. Insurance coverage may reduce out-of-pocket costs, so it's important to check with your provider regarding coverage for cervical discectomy surgery.
The other Spine Surgery Procedures are:
Few Major Hospitals for Cervical Discectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.