Stem cell transplantation, often referred to as hematopoietic stem cell transplantation (HSCT) or bone marrow transplantation, is a sophisticated medical procedure used to treat patients whose bone marrow or immune system is damaged or destroyed by disease, chemotherapy, or radiation. The goal of the transplant is to infuse healthy stem cells into a patient’s body so they can produce new blood cells and rebuild a functioning immune system.
Stem cells are immature blood-forming cells that reside in the bone marrow and can develop into the body’s three major types of blood cells: red blood cells, white blood cells, and platelets. A stem cell transplant is commonly used in the treatment of blood cancers such as leukemia, lymphoma, and multiple myeloma. It is also used in non-cancerous conditions such as aplastic anemia, severe immunodeficiencies, and inherited blood disorders like thalassemia.
There are two main types of stem cell transplantation:
-
Autologous Transplantation: Using the patient’s own stem cells.
-
Allogeneic Transplantation: Using stem cells from a donor, often a sibling, matched unrelated donor, or umbilical cord blood.
With the advancement of medical research, reduced-intensity conditioning regimens, better donor registries, and effective post-transplant care, stem cell transplantation is now safer and more accessible than ever before.
SCT is not a preventive or first-line therapy, but a therapeutic intervention reserved for patients with certain high-risk, refractory, or relapsed hematologic and immunologic conditions. The “causes” for undergoing SCT are, therefore, the underlying diseases that destroy or disrupt the normal bone marrow function.
Malignant Hematological Conditions
-
Acute Leukemias (AML, ALL) – rapidly progressing blood cancers that often relapse post-chemotherapy.
-
Chronic Leukemias (CML, CLL) – especially when resistant to tyrosine kinase inhibitors or associated with high-risk genetic markers.
-
Lymphomas (NHL, HL) – aggressive or recurrent cases where autologous SCT may serve as consolidation or salvage therapy.
-
Multiple Myeloma – a plasma cell cancer frequently treated with autologous transplant after induction chemotherapy.
Non-Malignant Conditions
-
Aplastic Anemia – failure of the bone marrow to produce blood cells.
-
Thalassemia Major – genetic hemoglobin disorder often treated with lifelong transfusions unless cured by SCT.
-
Sickle Cell Disease – severe forms may benefit from curative transplant if a matched donor is available.
-
Myelodysplastic Syndrome (MDS) – a pre-leukemic condition with poor prognosis that may progress to AML.
Primary Immunodeficiencies & Inherited Metabolic Disorders
-
SCID (Severe Combined Immunodeficiency)
-
Wiskott-Aldrich Syndrome
-
Hurler Syndrome and other lysosomal storage diseases
Autoimmune Disorders (Experimental)
-
Severe, refractory cases of systemic lupus erythematosus (SLE), multiple sclerosis (MS), or systemic sclerosis may benefit from autologous SCT.
Risk Factors for Needing SCT
-
Failure to achieve remission with first-line treatment.
-
High-risk cytogenetics or molecular mutations (e.g., TP53, FLT3).
-
Multiple relapses.
-
Age under 65 (especially for allogeneic SCT, though reduced-intensity regimens allow older adults).
-
Availability of a fully or partially matched donor.
Symptoms vary depending on the underlying condition but are usually severe or progressive by the time SCT is considered.
In Malignant Diseases
-
Fatigue, pallor, dyspnea on exertion
-
Fever, frequent infections due to leukopenia
-
Unexplained bruises, petechiae, or bleeding from gums/nose
-
Enlarged lymph nodes, spleen, or liver
-
Weight loss, night sweats
-
Bone pain or neurological symptoms in cases of CNS involvement
In Bone Marrow Failure or Genetic Disorders
-
Severe anemia requiring transfusions
-
Recurrent life-threatening infections
-
Growth retardation and skeletal deformities (especially in thalassemia)
-
Pain crises in sickle cell disease
-
Jaundice or iron overload symptoms due to chronic transfusion therapy
Prompt identification of these symptoms and timely referral to a transplant center can improve prognosis significantly.
Before a patient is considered for transplantation, an in-depth diagnostic and eligibility assessment is carried out.
Diagnostic Tests
-
Bone Marrow Aspiration and Biopsy – to assess disease burden, morphology, and response.
-
Cytogenetic Studies – e.g., Philadelphia chromosome, karyotyping.
-
Molecular Testing – FLT3, NPM1, JAK2, BCR-ABL, TP53, etc.
-
Flow Cytometry – immunophenotyping for lymphomas and leukemias.
-
Imaging – CT scans, MRI, PET-CT for disease staging and organ assessment.
-
Lumbar Puncture – if CNS involvement is suspected.
Transplant Eligibility Evaluation
-
HLA Typing – to find a matched donor (HLA-A, B, C, DRB1, DQB1).
-
Organ Function Tests – heart, liver, kidney, and lung evaluation.
-
Infectious Screening – CMV, EBV, HIV, Hepatitis B/C, VZV.
-
Psychosocial and Nutritional Assessment – crucial for long-term success.
A multidisciplinary transplant team decides on the conditioning regimen, type of transplant (autologous/allogeneic), donor source, and anticipated outcomes.
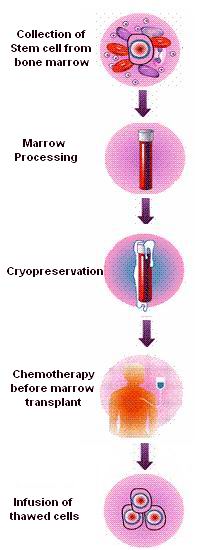
Pre-Transplant Conditioning
This phase involves chemotherapy (and sometimes radiation) to:
-
Destroy cancer cells or diseased marrow.
-
Suppress the immune system to allow donor cell engraftment.
Types:
-
Myeloablative Conditioning (MAC) – high intensity; suitable for young, healthy patients.
-
Reduced Intensity Conditioning (RIC) – used in older adults or those with comorbidities.
Stem Cell Sources
-
Peripheral Blood Stem Cells (PBSC) – now the most common source.
-
Bone Marrow Harvest – requires general anesthesia.
-
Umbilical Cord Blood – suitable for pediatric patients or those without a matched donor.
Transplant Infusion (Day 0)
-
Stem cells are thawed (if frozen) and infused intravenously.
-
The process is painless, much like a blood transfusion.
Engraftment Phase
-
Stem cells migrate to bone marrow and begin producing new blood cells.
-
ANC (absolute neutrophil count) recovery > 500/mm³ for 3 days is considered engraftment.
-
Usually occurs within 10–30 days depending on source and conditioning.
Infection Prophylaxis
-
Neutropenic precautions and strict hygiene.
-
Prophylactic antivirals (acyclovir), antifungals (fluconazole), and antibiotics (levofloxacin).
-
Pneumocystis jirovecii prophylaxis (trimethoprim-sulfamethoxazole).
GVHD Prevention (Allogeneic SCT)
-
Immunosuppressants (cyclosporine, tacrolimus, sirolimus).
-
Methotrexate or mycophenolate mofetil.
-
Post-transplant cyclophosphamide (for haploidentical transplants).
Nutritional and Psychosocial Support
-
High-calorie, neutropenic-safe diet.
-
Psychological counseling for anxiety, depression, body image changes.
Vaccinations
-
Re-vaccination schedule begins 6–12 months post-transplant:
-
DTP, polio (IPV), HepB, MMR, pneumococcal, influenza
-
Acute Complications
-
Mucositis – painful oral ulcers from chemotherapy.
-
Neutropenic Fever/Sepsis
-
Acute GVHD – manifests as:
-
Skin rash
-
Diarrhea
-
Liver dysfunction (elevated bilirubin)
-
Chronic Complications
-
Chronic GVHD – can affect skin, lungs, liver, joints, and eyes.
-
Organ Toxicities – heart (cardiomyopathy), lungs (pulmonary fibrosis), liver (veno-occlusive disease).
-
Infertility and Endocrine Disorders
-
Osteoporosis – from steroids or hormonal deficiency.
-
Secondary Cancers
-
Psychosocial Issues – PTSD, fear of recurrence, survivor's guilt
Despite risks, many of these complications are manageable and predictable with early intervention.
Life after SCT is a marathon, not a sprint. With successful engraftment, the journey toward recovery begins.
Post-Transplant Timeline
-
0–100 Days: Risk of acute infections, GVHD, close monitoring required.
-
3–6 Months: Immune system gradually rebuilds.
-
1 Year+: Full recovery possible; transition to survivorship care.
Lifestyle Adjustments
-
Avoid raw foods, crowded places, and unvaccinated individuals initially.
-
Return to school/work may take 6–12 months.
-
Safe sex practices until full immune reconstitution.
Quality of Life
-
With advances in care, most survivors report high satisfaction and return to normal life.
-
Long-term monitoring for relapse, late effects, fertility, and mental health is crucial.
1. What is Stem Cell Transplantation?
Stem cell transplantation is a medical procedure used to replace damaged or destroyed bone marrow with healthy stem cells. These stem cells can develop into red blood cells, white blood cells, and platelets. It is commonly used to treat certain cancers like leukemia, lymphoma, multiple myeloma, and some non-cancerous blood disorders such as aplastic anemia.
2. What are the different types of stem cell transplants?
There are three main types of stem cell transplantation:
-
Autologous transplant: Uses the patient’s own stem cells.
-
Allogeneic transplant: Uses stem cells from a genetically matched donor, usually a sibling or an unrelated donor.
-
Syngeneic transplant: Uses stem cells from an identical twin (rare).
3. Who is a suitable candidate for stem cell transplantation?
Candidates typically include patients with certain cancers (e.g., leukemia, lymphoma, myeloma) or non-malignant conditions (e.g., thalassemia, severe aplastic anemia). Eligibility depends on the patient’s age, overall health, disease status, and availability of a suitable donor.
4. What are the sources of stem cells for transplantation?
Stem cells for transplantation can be collected from:
-
Bone marrow (traditional method)
-
Peripheral blood (most common today)
-
Umbilical cord blood (used especially in pediatric cases)
5. How is the stem cell transplant procedure performed?
The process involves several steps:
-
Conditioning: High-dose chemotherapy or radiation to destroy diseased cells.
-
Infusion: Stem cells are infused into the patient’s bloodstream, similar to a blood transfusion.
-
Engraftment: The transplanted cells travel to the bone marrow and begin to produce new blood cells.
6. What are the major risks and complications associated with stem cell transplantation?
Risks may include:
-
Graft-versus-host disease (GVHD) in allogeneic transplants
-
Infections due to low immunity
-
Organ damage
-
Relapse of the underlying disease
-
Infertility and long-term side effects
7. What is graft-versus-host disease (GVHD)?
GVHD is a condition where the donor stem cells attack the recipient’s tissues. It can range from mild to life-threatening and commonly affects the skin, liver, and gastrointestinal tract. Immunosuppressive medications are used to manage or prevent GVHD.
8. How long is the recovery period after a stem cell transplant?
Recovery varies but typically includes:
-
Initial hospital stay: 2 to 4 weeks
-
Home recovery: Several months of careful monitoring
-
Full recovery can take 6 months to a year or more, depending on the individual’s condition and transplant type.
9. Can stem cell transplantation cure cancer?
In many cases, stem cell transplantation offers the potential for long-term remission or cure, especially in blood cancers. However, outcomes vary based on disease type, stage, response to treatment, and individual patient factors.
10. What is the success rate of stem cell transplantation?
Success rates depend on many variables such as:
-
Type of transplant (autologous vs. allogeneic)
-
Patient’s age and general health
-
Disease status at the time of transplant
Generally, autologous transplants have fewer complications and higher success rates. Allogeneic transplants can offer curative potential but carry higher risks. Overall survival rates have significantly improved due to advances in technology and supportive care.
The other Oncology Procedures are
Few Major Hospitals for treatment of Stem Cell Transplantation are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



