Stroke risk increases due to several modifiable and non-modifiable factors. When medications and lifestyle changes are not sufficient, or when structural issues in the heart or blood vessels are identified, surgical treatment becomes necessary.
Common Causes of Stroke:
-
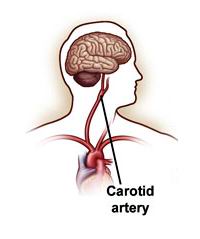
Atherosclerosis: Buildup of fatty plaques in arteries, especially in the carotid arteries in the neck
-
Atrial fibrillation (AFib): Irregular heart rhythm leading to blood clots
-
Patent Foramen Ovale (PFO): A small opening in the heart that can allow clots to pass to the brain
-
Cerebral aneurysms or arteriovenous malformations (AVMs): Weak blood vessels that may rupture
Risk Factors That May Warrant Surgical Intervention:
-
Previous mini-stroke or TIA
-
Severe carotid artery narrowing (typically over 70%)
-
Heart conditions leading to embolic strokes
-
High risk of recurrent stroke
-
Family history of stroke or aneurysm rupture
Atherosclerosis: Buildup of fatty plaques in arteries, especially in the carotid arteries in the neck
Atrial fibrillation (AFib): Irregular heart rhythm leading to blood clots
Patent Foramen Ovale (PFO): A small opening in the heart that can allow clots to pass to the brain
Cerebral aneurysms or arteriovenous malformations (AVMs): Weak blood vessels that may rupture
Previous mini-stroke or TIA
Severe carotid artery narrowing (typically over 70%)
Heart conditions leading to embolic strokes
High risk of recurrent stroke
Family history of stroke or aneurysm rupture
Preventing stroke through surgery is often considered in patients where medical therapy alone is not enough, or where structural defects pose a significant risk.
Identifying individuals who might benefit from stroke-prevention surgery involves recognizing early warning signs of reduced blood flow or vascular abnormalities.
Indicating Stroke Risk:
-
Transient ischemic attacks (TIAs): Temporary episodes of numbness, weakness, slurred speech, or vision changes
-
Frequent dizziness or loss of balance
-
Sudden confusion or trouble understanding speech
-
Unexplained fainting or seizures
-
Numbness or weakness on one side of the body
-
Severe headache, especially if caused by an aneurysm
Identifying individuals who might benefit from stroke-prevention surgery involves recognizing early warning signs of reduced blood flow or vascular abnormalities.
Symptoms Indicating Stroke Risk:
-
Transient ischemic attacks (TIAs): Temporary episodes of numbness, weakness, slurred speech, or vision changes
-
Frequent dizziness or loss of balance
-
Sudden confusion or trouble understanding speech
-
Unexplained fainting or seizures
-
Numbness or weakness on one side of the body
-
Severe headache, especially if caused by an aneurysm
Before recommending surgery, doctors perform a comprehensive series of diagnostic tests to evaluate the condition of the brain, heart, and blood vessels. These tests help identify blockages, aneurysms, abnormal blood flow, or structural defects that increase stroke risk.
Common Diagnostic Tests:
-
Carotid Ultrasound (Doppler Study): Checks for narrowing or blockages in the carotid arteries
-
CT Angiography or MR Angiography: Creates detailed images of blood vessels in the brain and neck
-
Cerebral Angiogram: An invasive test that maps out blood flow and pinpoints aneurysms or AVMs
-
Echocardiogram (with Bubble Study): Detects PFO or other heart defects that may cause clots to travel to the brain
-
Electrocardiogram (ECG): Identifies atrial fibrillation or other rhythm issues
-
Blood tests: Used to evaluate cholesterol levels, clotting disorders, and inflammatory markers
When lifestyle modification and medication are not enough, several surgical and minimally invasive procedures are available to significantly reduce stroke risk:
1. Carotid Endarterectomy (CEA):
-
A surgery to remove plaque buildup from the carotid arteries (major arteries in the neck).
-
Recommended for patients with 70% or more narrowing of the carotid artery.
-
Reduces the risk of stroke in patients who have had a TIA or mild stroke.
-
Performed under general or local anesthesia.
-
Involves making a small incision, removing the plaque, and stitching the artery closed.
2. Carotid Artery Stenting (CAS):
-
A less invasive alternative to CEA.
-
A stent (mesh tube) is inserted via catheter into the narrowed carotid artery to keep it open.
-
Ideal for patients who are high-risk for open surgery due to age or other medical conditions.
-
Faster recovery time but may carry a slightly higher risk of stroke during the procedure.
3. Patent Foramen Ovale (PFO) Closure:
-
A PFO is a hole in the heart present in some adults.
-
In patients who suffer cryptogenic strokes (stroke of unknown cause), PFO closure may reduce recurrence.
-
Performed using a catheter-based procedure, placing a device that seals the hole.
-
Especially effective in younger stroke patients with no other apparent cause.
4. Aneurysm Clipping and Coiling:
-
For patients with brain aneurysms or AVMs, surgery may prevent rupture and future strokes.
-
Clipping involves placing a metal clip at the base of the aneurysm.
-
Coiling is a minimally invasive technique using platinum coils inserted via catheter to fill the aneurysm.
-
Decision depends on size, location, and risk of rupture.
5. Left Atrial Appendage Closure (LAAC):
-
A procedure used in patients with atrial fibrillation who are at high risk of forming blood clots in the heart.
-
Involves placing a device (e.g., Watchman device) to close off the appendage of the heart where clots tend to form.
Each procedure is selected based on individual risk assessment, imaging results, and overall health.
6. Prevention and Management of Stroke Risk
While surgery plays a critical role in high-risk individuals,ongoing prevention and management are equally important.
-
Control high blood pressure, cholesterol, and diabetes
-
Stop smoking and limit alcohol intake
-
Follow a heart-healthy diet (low sodium, high fiber, lean proteins)
-
Stay physically active and maintain a healthy weight
-
Take prescribed antiplatelet or anticoagulant medications
-
Undergo regular screenings for heart rhythm disorders like AFib
Post-Surgical Management:
-
Follow post-operative care instructions strictly
-
Attend follow-up appointments for imaging and testing
-
Continue medications as prescribed
-
Report any recurrence of symptoms immediately
-
Work with a neurologist and cardiologist for integrated care
Stroke prevention doesn’t stop at surgery—it involves lifelong vigilance and healthy habits.
While generally safe, every surgical or interventional procedure comes with potential risks. Complications may vary depending on the specific type of surgery performed and the patient’s overall health.
Possible Complications Include:-
Stroke during the procedure (especially with carotid stenting)
-
Bleeding or hematoma at the catheter site
-
Infection at the incision or insertion point
-
Allergic reaction to contrast dye (used during angiography)
-
Nerve damage (rare, associated with carotid endarterectomy)
-
Device migration or incomplete closure in stenting or PFO procedures
-
Recurrence of symptoms if follow-up care is not properly followed
These risks are minimized with skilled surgical teams, careful patient selection, and ongoing post-procedure monitoring.
While generally safe, every surgical or interventional procedure comes with potential risks. Complications may vary depending on the specific type of surgery performed and the patient’s overall health.
Possible Complications Include:
-
Stroke during the procedure (especially with carotid stenting)
-
Bleeding or hematoma at the catheter site
-
Infection at the incision or insertion point
-
Allergic reaction to contrast dye (used during angiography)
-
Nerve damage (rare, associated with carotid endarterectomy)
-
Device migration or incomplete closure in stenting or PFO procedures
-
Recurrence of symptoms if follow-up care is not properly followed
These risks are minimized with skilled surgical teams, careful patient selection, and ongoing post-procedure monitoring.
What Patients Should Do Post-Surgery:
Living with a history of stroke or stroke risk factors requires a comprehensive, long-term strategy. Surgery is just one part of the picture—lifestyle, medications, and regular health checks are equally vital.
-
Stick to prescribed medications like blood thinners or statins.
-
Adopt a brain-healthy lifestyle: low salt diet, regular walking or light exercise, good sleep.
-
Monitor blood pressure and blood sugar regularly.
-
Stay engaged with healthcare providers—neurologists, cardiologists, vascular surgeons.
-
Address mental health—anxiety or depression after a stroke scare is common.
Support groups, education, and a positive outlook can go a long way in helping patients live fear-free and empowered.
The other major cardiac procedures are:
Few Major Hospitals for Surgery for Stroke Prevention are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Carotid Endarterectomy | vascular surgeon | carotid artery | plaque | CAD | Carotid Artery Disease | atherosclerosis | basilar artery | Transient Ischemic Attack | TIA | mini stroke | Endarterectomy | Angioplasty | stenting | tingling | numbness | blurred vision | paralysis | weakness in arm or leg | difficulty swallowing | asymptomatic carotid artery disease | Hospitals Surgery for Stroke Prevention | Surgery for Stroke Prevention | Doctors Surgery for Stroke Prevention | cost Surgery for Stroke Prevention | Treatment Surgery for Stroke Prevention | Destinations Surgery for Stroke Prevention | Surgery for Stroke Prevention India | Surgery for Stroke Prevention Recovery | Risks Surgery for Stroke Prevention | Surgery for Stroke Prevention Information | Surgery for Stroke Prevention Thailand | Surgery for Stroke Prevention Malaysia | Surgery for Stroke Prevention abroad | Surgery for Stroke Prevention overseas | Surgery for Stroke Prevention low cost
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.