Root canal treatment (RCT), also known as endodontic therapy, is a specialized dental procedure designed to save a tooth whose pulp—the innermost soft tissue containing nerves and blood vessels—has become inflamed or infected. This inflammation or infection can arise due to deep tooth decay, trauma, cracks, or repeated dental procedures. If untreated, it can lead to severe pain, abscess formation, and eventual tooth loss.
The primary goal of root canal treatment is to remove diseased or dead pulp tissue, thoroughly disinfect the root canals, and then fill and seal them to prevent reinfection. Modern advancements in dental techniques and technology have made RCT one of the most predictable and successful treatments to preserve natural teeth, helping patients maintain their oral function and aesthetics.
This extensive guide explores causes and risk factors that often necessitate root canal treatment, common symptoms and signs, diagnostic procedures, available treatment options, prevention strategies, potential complications, and lifestyle considerations for living with and caring for a root canal treated tooth.
Causes of Pulpal Infection and Necrosis
-
Deep Dental Decay: Untreated caries eventually reach the pulp chamber, allowing bacterial infiltration leading to pulpitis and infection.
-
Dental Trauma: Physical injuries like cracks, fractures, or dislodgment can expose or damage the pulp.
-
Repeated Dental Treatments: Multiple restorations or aggressive dental work may irritate or damage the pulp.
-
Severe Gum Disease: Advanced periodontitis affecting the root surfaces can compromise pulp vitality.
-
Pulpal Necrosis: Resulting from prolonged ischemia or infection, leading to pulp death.
Risk Factors Increasing the Likelihood of RCT
-
Poor Oral Hygiene: Leading to frequent cavities and dental decay.
-
High Sugar Diet: Increases cariogenic bacterial activity.
-
History of Dental Trauma: Sports injuries, accidents, or parafunctional habits like bruxism.
-
Age: Older teeth may have reduced blood supply, increasing vulnerability.
-
Previous Extensive Dental Work: Crowns or large fillings can predispose pulp inflammation.
-
Smoking: Negatively impacts healing and immune response.
-
Systemic Health Conditions: Diabetes and autoimmune diseases can exacerbate oral infections.
Recognizing the clinical signs and symptoms of pulpal disease is crucial for timely intervention.
-
Severe Toothache: Persistent, throbbing pain often worsened by pressure or chewing.
-
Prolonged Sensitivity: Pain triggered by hot or cold stimuli that lingers even after the stimulus is removed.
-
Spontaneous Pain: Occurring without any apparent trigger.
-
Swelling and Tenderness: Around the affected tooth or adjacent gums.
-
Discoloration of Tooth: Darkening or graying due to pulp necrosis.
-
Presence of Abscess: Gum swelling with a pus-filled “pimple” indicating infection.
-
Bad Taste or Odor: From draining infection.
-
Loose Tooth: Due to inflammation affecting supporting structures.
Clinical Examination
-
Inspection for caries, cracks, swelling, or fistulas.
-
Palpation and percussion tests to check for tenderness.
-
Thermal and electric pulp tests to assess vitality.
-
Evaluation of periodontal status.
Radiographic Assessment
-
Periapical Radiographs: Essential for visualizing the extent of decay, presence of periapical radiolucency, and root anatomy.
-
Cone Beam Computed Tomography (CBCT): Used in complex cases to provide 3D images for detailed evaluation.
Additional Diagnostic Tools
-
Patient history focusing on pain characteristics and duration.
-
Assessment of occlusion and functional factors.
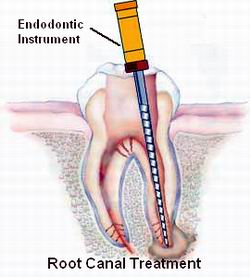
Standard Root Canal Therapy Procedure
-
Local Anesthesia: To ensure a pain-free experience.
-
Access Opening: Creating an opening through the crown into the pulp chamber.
-
Removal of Diseased Pulp: Cleaning out the infected or necrotic pulp tissue.
-
Shaping and Cleaning the Canals: Using hand or rotary files and irrigation solutions to disinfect and shape canals.
-
Filling and Sealing: Filling the canals with gutta-percha and sealing with cement to prevent bacterial re-entry.
-
Restoration: Placing a permanent filling or crown to restore tooth integrity and function.
Advanced Techniques
-
Use of dental operating microscopes for improved visualization.
-
Laser-assisted disinfection.
-
Bioceramic sealers for superior sealing.
Alternatives to RCT
-
Pulpotomy: Partial removal of pulp tissue in specific cases, mainly in pediatric dentistry.
-
Extraction: If the tooth is non-restorable or infection is extensive.
Preventive Strategies
-
Maintain meticulous oral hygiene: brushing twice daily and flossing once daily.
-
Regular dental check-ups and professional cleanings.
-
Use fluoride toothpaste and consider dental sealants.
-
Avoid excessive sugary and acidic foods.
-
Protective measures against trauma and bruxism.
Post-Treatment Management
-
Adhere to dentist’s instructions regarding pain control and oral care.
-
Avoid chewing hard or sticky foods on the treated tooth until restoration.
-
Attend follow-up appointments for monitoring.
-
Consider a full-coverage crown to protect the treated tooth from fracture.
Potential Complications
-
Persistent or recurrent infection due to incomplete cleaning.
-
Instrument separation inside canals.
-
Perforation of root canals or chambers.
-
Overfilling or underfilling canals.
-
Post-operative pain or swelling.
-
Tooth fracture if not adequately restored.
-
Allergic reactions to filling materials (rare).
Managing Complications
-
Retreatment or surgical endodontics if infection persists.
-
Pain management strategies.
-
Referral to specialists for complex cases.
Longevity and Success
-
With proper care, root canal treated teeth can last a lifetime.
-
They function like natural teeth, allowing normal chewing and speaking.
Oral Hygiene Importance
-
Maintaining excellent oral hygiene to prevent new infections.
-
Regular dental visits to detect any early issues.
Protective Restorations
-
Crowns significantly reduce risk of fracture.
-
Avoid biting hard objects or ice.
Psychological and Quality of Life Benefits
-
Relief from chronic pain and infection.
-
Preservation of natural teeth enhances confidence and nutrition.
1. What is root canal treatment?
Root canal treatment is a dental procedure used to treat infection or damage inside the tooth’s pulp (the soft tissue containing nerves and blood vessels). It involves removing the infected pulp, cleaning and disinfecting the root canals, and sealing them to save the tooth.
2. When is root canal treatment necessary?
It is necessary when the pulp becomes inflamed or infected due to deep decay, repeated dental procedures, cracks, or trauma. Symptoms often include severe tooth pain, sensitivity to hot or cold, swelling, or abscess formation.
3. How is root canal treatment performed?
The dentist or endodontist numbs the area, creates an access opening in the tooth, removes the damaged pulp, cleans and shapes the canals, and fills them with a biocompatible material called gutta-percha. The tooth is then sealed and usually restored with a crown.
4. Is root canal treatment painful?
Modern techniques and anesthesia make root canal treatment relatively painless. Many patients feel relief from pain after the infection is removed, and discomfort during the procedure is minimal.
5. How long does root canal treatment take?
The procedure can typically be completed in one to two visits, lasting 60 to 90 minutes each depending on the complexity and number of canals.
6. What is the success rate of root canal treatment?
Root canal treatment has a success rate of about 85-97%. With proper care and restoration, treated teeth can last a lifetime.
7. What should I expect after root canal treatment?
Some mild soreness or sensitivity is normal for a few days. Pain can be managed with over-the-counter medications, and maintaining good oral hygiene is important. Follow-up visits may be necessary to place a permanent crown.
8. Can a root canal-treated tooth get infected again?
Yes, reinfection can occur if the tooth isn’t properly sealed or if new decay develops. Regular dental checkups and good oral hygiene help prevent this.
9. Are there alternatives to root canal treatment?
The main alternative is tooth extraction, but saving the natural tooth with root canal treatment is preferred to maintain chewing function and jawbone health.
10. How much does root canal treatment cost?
Costs vary by location and complexity but generally range between $700 and $1,500. Dental insurance may cover part of the cost.
The other Dental Procedures are:
Few Popular Hospitals for Tooth Veneers are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.