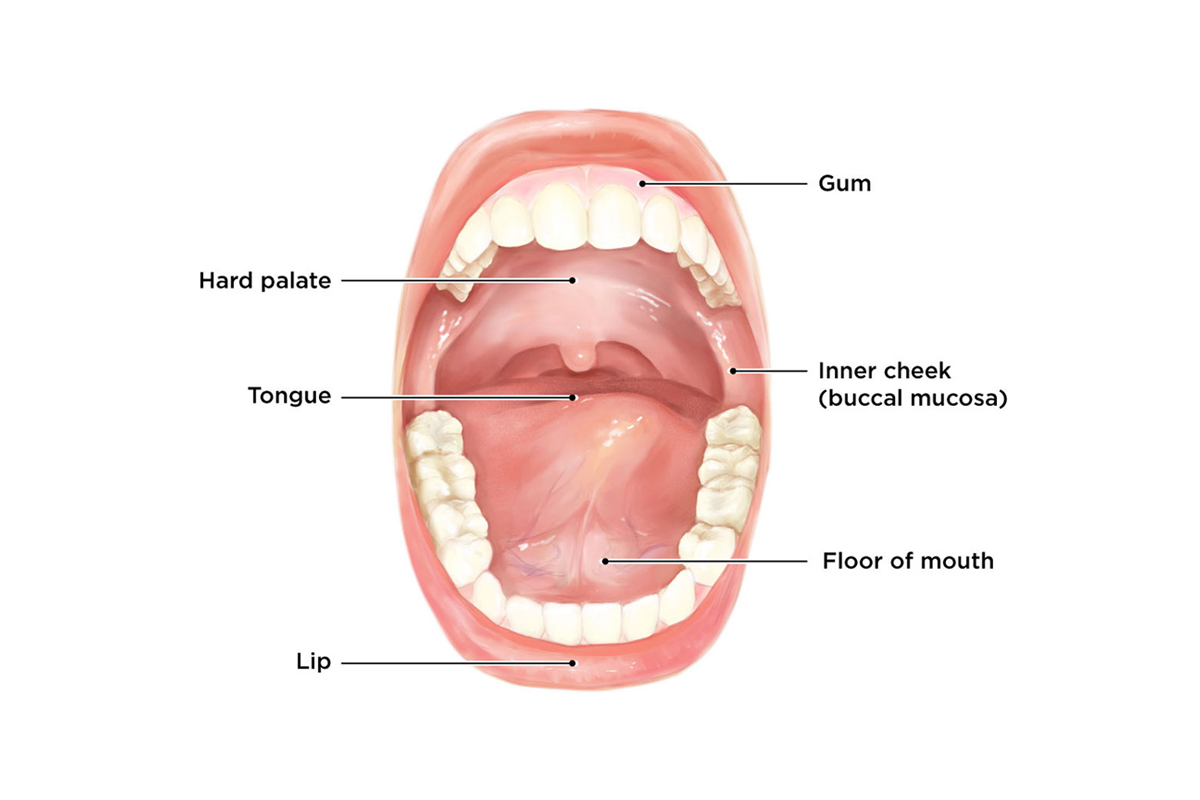
Mouth tumors refer to abnormal growths that occur anywhere in the oral cavity, including the lips, tongue, floor of the mouth, palate, cheeks, gums, and jawbones. These growths range from benign (non-cancerous) lesions to malignant (cancerous) tumors. Oral cancer, predominantly oral squamous cell carcinoma, accounts for a significant number of global cancer cases and poses serious health risks if not diagnosed and treated early.
Understanding mouth tumors is essential, as early detection greatly increases the chance of successful treatment and improves survival rates. Tumors in the mouth can cause functional problems such as difficulty speaking, chewing, swallowing, and may alter facial aesthetics, which can profoundly affect a person’s quality of life.
This detailed guide covers the causes and risk factors of mouth tumors, common symptoms and signs, diagnostic processes, treatment modalities, prevention strategies, potential complications, and guidance on living with and beyond mouth tumors.
Causes and Risk Factors of Mouth Tumors
Primary Causes
-
Tobacco Use:
Smoking cigarettes, cigars, pipes, and the use of smokeless tobacco introduces carcinogens directly to oral tissues, causing cellular mutations and cancer development. Tobacco remains the single largest risk factor worldwide. -
Excessive Alcohol Consumption:
Alcohol acts synergistically with tobacco, damaging oral mucosa and facilitating carcinogen absorption. Chronic alcohol abuse significantly increases oral cancer risk. -
Human Papillomavirus (HPV) Infection:
High-risk HPV types, especially HPV-16, have been linked to a rising number of oropharyngeal and some oral cavity cancers, particularly among younger populations. -
Chronic Irritation and Inflammation:
Ill-fitting dentures, chronic trauma from broken teeth, and poor oral hygiene can cause persistent inflammation that may predispose to tumor formation. -
Sun Exposure:
Particularly affects the lower lip, increasing the risk of lip cancer due to UV radiation. -
Nutritional Deficiencies:
Diets low in fruits, vegetables, and antioxidants may weaken mucosal defenses. -
Genetics and Family History:
Genetic predispositions and inherited mutations in tumor suppressor genes can increase susceptibility. -
Immune System Suppression:
Patients with HIV/AIDS or those on immunosuppressive medications have a heightened risk.
Additional Risk Factors
-
Age (most patients diagnosed over 40 years old).
-
Male gender has traditionally higher incidence but gap narrowing.
-
Occupational exposures (asbestos, wood dust).
-
Poor dental care and oral hygiene.
Early tumors may be asymptomatic or mimic benign lesions, making vigilance critical.
-
Non-Healing Ulcers:
Any ulcer or sore in the mouth that persists beyond two weeks without healing warrants investigation. -
Leukoplakia and Erythroplakia:
White or red patches, respectively, often precancerous, detected during routine oral exams. -
Lumps or Swellings:
Firm or soft growths, sometimes painful or tender. -
Persistent Pain:
Localized or radiating pain, which may be mild or severe. -
Numbness or Tingling:
Indicating nerve involvement or tumor infiltration. -
Difficulty Swallowing (Dysphagia):
Tumors obstructing the oropharynx or esophagus. -
Changes in Speech:
Slurred or muffled speech due to tongue or palate involvement. -
Loose Teeth or Poor Denture Fit:
Caused by bone destruction or tumor infiltration. -
Enlarged Neck Lymph Nodes:
Suggestive of metastasis. -
Unexplained Bleeding or Bad Breath:
From tumor ulceration or necrosis.
Clinical Evaluation
-
Complete history focusing on risk factors, duration of symptoms, and functional impairment.
-
Visual and tactile inspection under bright light.
-
Assessment of lymph nodes for enlargement or tenderness.
Imaging Studies
-
Panoramic Radiograph (OPG):
Evaluates bone involvement and dental status. -
Computed Tomography (CT) Scan:
Provides detailed information about bone destruction, tumor margins, and spread. -
Magnetic Resonance Imaging (MRI):
Superior for soft tissue delineation, assessing tumor depth, and nerve involvement. -
Positron Emission Tomography (PET) Scan:
Detects metastasis and recurrent disease.
Biopsy Procedures
-
Incisional Biopsy:
Removal of a small tissue sample from the lesion for histopathology. -
Excisional Biopsy:
Complete removal if lesion is small and accessible. -
Fine Needle Aspiration Cytology (FNAC):
Used mainly for enlarged lymph nodes.
Additional Tests
-
Blood tests to evaluate general health.
-
HPV typing for oropharyngeal tumors.
Treatment depends on tumor type, location, stage, and patient factors.
Surgery
-
Primary treatment for most oral cancers.
-
Wide local excision with clear margins.
-
Neck dissection for metastatic lymph nodes.
-
Reconstruction using local flaps, free flaps, or grafts to restore oral function and aesthetics.
Radiotherapy
-
Used alone or as adjunct to surgery.
-
Intensity-modulated radiotherapy (IMRT) targets tumors precisely while sparing normal tissues.
-
Side effects include mucositis, xerostomia (dry mouth), and osteoradionecrosis.
Chemotherapy
-
Often combined with radiotherapy for advanced disease.
-
Common drugs include cisplatin, 5-FU.
-
Can be neoadjuvant (pre-surgical) or adjuvant (post-surgical).
Targeted Therapy and Immunotherapy
-
EGFR inhibitors (e.g., cetuximab) target specific cancer cell pathways.
-
Immune checkpoint inhibitors show promise for recurrent/metastatic tumors.
Multidisciplinary Care
-
Collaborative management by surgeons, medical and radiation oncologists, speech therapists, dietitians, and psychologists.
Prevention Strategies
-
Complete cessation of tobacco and alcohol use.
-
HPV vaccination for eligible populations.
-
Regular dental and medical check-ups for early detection.
-
Sun protection for lips.
-
Nutritional improvements emphasizing fruits and vegetables.
-
Oral hygiene maintenance and dental care.
Management Approaches
-
Early treatment initiation.
-
Supportive care including pain control, nutritional support.
-
Rehabilitation including speech and swallowing therapy.
-
Psychological counseling to address mental health needs.
Tumor-Related
-
Local invasion causing destruction of oral tissues.
-
Spread to lymph nodes or distant metastasis.
-
Infection, bleeding, and necrosis.
Treatment-Related
-
Surgical complications: nerve damage, facial disfigurement, functional deficits.
-
Radiotherapy side effects: mucositis, xerostomia, dental caries, osteonecrosis.
-
Chemotherapy toxicity: nausea, immunosuppression, organ toxicity.
-
Psychological distress and impact on quality of life.
Rehabilitation
-
Speech therapy to restore articulation.
-
Swallowing therapy to manage dysphagia.
-
Prosthetic rehabilitation for lost teeth and oral structures.
Follow-Up
-
Regular surveillance for recurrence.
-
Management of long-term side effects.
-
Nutritional and psychological support.
Lifestyle Adaptations
-
Avoiding risk factors.
-
Maintaining oral hygiene.
-
Joining support groups.
1. What are mouth tumors?
Mouth tumors are abnormal growths or masses that develop in the tissues of the oral cavity, including the lips, tongue, cheeks, gums, and roof or floor of the mouth. They can be benign (non-cancerous) or malignant (cancerous).
2. What causes mouth tumors?
Causes vary and can include tobacco use, excessive alcohol consumption, human papillomavirus (HPV) infection, prolonged sun exposure (for lip tumors), poor oral hygiene, and genetic factors.
3. What are the common symptoms of mouth tumors?
Symptoms may include a persistent sore or lump in the mouth, pain or difficulty swallowing, unexplained bleeding, numbness, white or red patches, or changes in speech or chewing.
4. How are mouth tumors diagnosed?
Diagnosis involves a thorough oral examination, imaging tests (like X-rays, CT scans, or MRIs), and biopsy where a small tissue sample is taken for microscopic evaluation.
5. Are all mouth tumors cancerous?
No, not all mouth tumors are cancerous. Many are benign and may only require monitoring or minor treatment. However, some tumors are malignant and require aggressive treatment.
6. What treatment options are available for mouth tumors?
Treatment depends on the tumor type and stage and may include surgical removal, radiation therapy, chemotherapy, or a combination. Benign tumors may be removed surgically or observed.
7. Can mouth tumors be prevented?
While not all can be prevented, risks can be lowered by avoiding tobacco and excessive alcohol, practicing good oral hygiene, protecting lips from sun exposure, and getting regular dental checkups.
8. What is the prognosis for patients with malignant mouth tumors?
Prognosis depends on the tumor size, location, stage at diagnosis, and overall patient health. Early detection significantly improves outcomes.
9. How often should I get screened for mouth tumors?
Routine dental checkups should include an oral cancer screening at least once a year, especially for individuals with risk factors like tobacco use or HPV infection.
10. When should I see a doctor about a suspicious lesion in my mouth?
If you notice any persistent sore, lump, or unusual patch in your mouth lasting more than two weeks, or experience unexplained pain or bleeding, consult a healthcare professional promptly.
The other Dental Procedures are:
Few Popular Hospitals for treatment of Mouth Tumors are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.