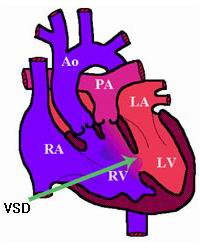
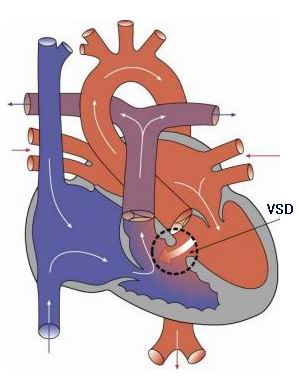
A Ventricular Septal Defect (VSD) is a congenital heart defect characterized by an abnormal hole in the septum, the wall that separates the heart's two lower chambers, known as the ventricles. This defect allows oxygenated blood from the left ventricle to mix with deoxygenated blood from the right ventricle, causing inefficient blood flow and overloading the heart. While small VSDs may not cause significant symptoms and can close on their own as a child grows, larger VSDs can lead to serious complications such as heart failure, pulmonary hypertension, and cyanosis (a bluish tint to the skin due to insufficient oxygen in the blood). In such cases, surgical closure of the VSD is necessary to restore normal heart function and improve the child’s health. VSD closure is typically performed through open-heart surgery or a minimally invasive catheter-based procedure to repair or close the defect, improving blood flow and preventing further heart damage.
Causes of Ventricular Septal Defect (VSD)
VSD is a congenital condition, meaning it occurs during fetal development. It is caused by abnormalities in the formation of the heart's septum. The causes of VSDs include:
-
Genetic Factors
VSDs may be associated with genetic mutations that affect heart development. A family history of congenital heart defects increases the likelihood of having a child with VSD. Genetic syndromes like Down syndrome or DiGeorge syndrome also increase the risk of VSDs. -
Maternal Health Conditions
Conditions such as diabetes, infections, or poor nutrition during pregnancy may affect fetal heart development and lead to defects like VSD. -
Chromosomal Abnormalities
Abnormalities in chromosomes, such as Down syndrome, Turner syndrome, and Edward syndrome, are associated with an increased risk of congenital heart defects, including VSDs. -
Environmental Factors
Exposure to certain medications, drugs, alcohol, or environmental toxins during pregnancy can contribute to the development of VSDs in the fetus.
The symptoms of VSD depend on the size of the hole and whether it is associated with other congenital heart defects. While small VSDs may not cause noticeable symptoms, larger defects can lead to a variety of heart-related issues:
-
Heart Murmur
A heart murmur, an abnormal sound caused by blood flowing through the hole in the septum, is often the first clue that a VSD is present. It is typically detected by a pediatrician or cardiologist during a routine exam. -
Cyanosis (Bluish Skin)
Cyanosis is a common symptom of larger VSDs. It occurs when oxygenated and deoxygenated blood mix, reducing the oxygen levels in the blood and causing a bluish tint to the skin, lips, or nails. -
Fatigue and Weakness
Babies and children with a VSD may appear unusually tired or weak, especially during feeding or physical activity, due to inefficient blood circulation. -
Rapid Breathing
Infants with a significant VSD may experience difficulty breathing and may breathe rapidly (tachypnea) due to the overload of blood in the lungs and reduced oxygen circulation. -
Poor Feeding and Failure to Thrive
Babies with larger VSDs may have difficulty feeding due to shortness of breath, which can result in poor growth and failure to thrive. -
Swelling (Edema)
In severe cases, swelling in the legs, abdomen, or other areas of the body may develop due to fluid buildup, which occurs when the heart cannot efficiently pump blood. -
Frequent Respiratory Infections
Children with untreated VSDs are more susceptible to respiratory infections due to fluid buildup in the lungs or the body's inability to distribute oxygenated blood properly.
Diagnosing VSD typically involves a combination of physical examinations, imaging tests, and diagnostic procedures to assess the defect and determine the best course of treatment. Common diagnostic tools include:
-
Physical Examination
A pediatrician or cardiologist may detect a heart murmur during a physical exam. The doctor will also assess the baby’s growth, listen for abnormal heart sounds, and check for signs of cyanosis or respiratory distress. -
Echocardiogram (Ultrasound of the Heart)
An echocardiogram is the primary test for diagnosing VSD. This non-invasive imaging technique uses sound waves to create real-time images of the heart. It can show the size of the VSD and the impact it has on heart function. -
Chest X-ray
A chest X-ray helps to evaluate the size and shape of the heart and lungs. It may show signs of enlarged heart chambers or fluid accumulation in the lungs. -
Electrocardiogram (ECG)
An ECG records the heart's electrical activity and can help detect arrhythmias (irregular heartbeats) that might result from a VSD. -
Cardiac MRI or CT Scan
Advanced imaging like cardiac MRI or CT angiography can provide high-resolution images of the heart’s structure, helping to assess the extent of the VSD and any associated heart conditions. -
Cardiac Catheterization
In rare cases, cardiac catheterization is performed. This procedure involves inserting a catheter into the heart through a blood vessel to measure pressure and visualize blood flow within the heart’s chambers.
The approach to treating a VSD depends on several factors, including the size of the defect, presence of symptoms, patient age, and risk of complications.
1. Observation and Monitoring:
-
Small VSDs with no symptoms may not require immediate intervention.
-
Regular checkups are essential to monitor for spontaneous closure or signs of complications.
2. Medications:
-
Diuretics to remove excess fluid and ease the heart’s workload
-
ACE inhibitors to lower blood pressure in the lungs and improve heart function
-
Beta-blockers for heart rhythm management
-
Antibiotics may be prescribed before dental or surgical procedures to prevent infective endocarditis in some cases
3. Surgical Closure:
-
Indicated for large VSDs, especially when associated with heart failure, poor growth, or pulmonary hypertension
-
Performed through open-heart surgery, where the defect is closed with a synthetic patch or stitches
-
Usually done in infancy or early childhood; success rates are very high with low risk
4. Transcatheter Device Closure:
-
A minimally invasive alternative to open surgery, suitable for certain types of muscular or perimembranous VSDs
-
Involves placing a closure device via a catheter inserted through a vein
-
Reduces hospital stay and recovery time
-
Not suitable for all VSD types, especially large or complex ones
While VSDs cannot usually be prevented since they occur during fetal development, certain measures may reduce the risk or help manage the condition effectively.
Prevention Tips:
-
Prenatal care is crucial – regular checkups, ultrasounds, and screenings during pregnancy help detect congenital defects early.
-
Control chronic conditions like diabetes before and during pregnancy.
-
Avoid alcohol, tobacco, and harmful medications while pregnant.
-
Get vaccinated for rubella and other infections that may affect fetal development.
-
Genetic counseling may be helpful for parents with a family history of congenital heart disease.
Management Post-Diagnosis:
-
Lifelong monitoring may be required even after successful treatment to check for residual defects or arrhythmias.
-
Follow a heart-healthy lifestyle, including regular physical activity, a balanced diet, and avoiding tobacco.
-
Psychological support for families and children with heart defects can improve coping and emotional well-being.
If untreated or poorly managed, a VSD can lead to serious and sometimes life-threatening complications:
-
Congestive Heart Failure (CHF):
Due to excessive blood flow to the lungs and overwork of the heart -
Pulmonary Hypertension:
Increased pressure in lung arteries, which can become irreversible if not managed -
Endocarditis:
Infection of the heart lining or valves, more common in people with heart defects -
Arrhythmias:
Irregular heartbeats due to stretching and damage to heart tissue -
Delayed Growth and Development:
Particularly in infants and young children with large defects -
Eisenmenger’s Syndrome:
A rare but severe condition where long-standing VSD leads to irreversible pulmonary hypertension and cyanosis (bluish discoloration)
Living with VSD—especially after treatment—is often completely normal. Most children who undergo VSD closure go on to live healthy, active lives with few or no restrictions.
Life After Surgery or Device Closure:
-
Recovery time after surgery may vary, but most children return to normal activity within weeks.
-
Regular checkups are necessary to monitor heart function and ensure the defect has been completely closed.
-
Antibiotics may be required before certain procedures to prevent endocarditis.
Lifestyle and Activity:
-
Children with treated or small VSDs usually have no limitations on physical activity.
-
A nutritious diet, stress management, and avoiding smoking or alcohol are essential for long-term heart health.
-
Adults with previously repaired VSDs should continue cardiac follow-ups, especially if they plan to become pregnant or engage in intense physical activity.
The other major cardiac procedures are:
Few Major Hospitals for VSD are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Ventricular Septal Defect | VSD | ventricular septum | right endocardial cushion | muscular septum | conal septum | membraneous septum | outlet/infundibular septum | cyanosis | lack of appetite | prolonged fever | Polyester patch | cardiac catheterization | catheter | septum | hole in the septum | Nitinol Frame | Nitinol release wire | Hospitals VSD | Doctors VSD | Surgery VSD | Cost VSD | Treatment VSD | Destinations VSD | Risks VSD | VSD India | VSD Recovery | VSD Information | VSD Thailand | VSD Malaysia | VSD Singapore | VSD abroad | VSD overseas | VSD low cost | VSD in Apollo Hospital
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.