Obesity is a global epidemic with profound health, social, and economic consequences. When conventional weight loss methods such as diet, exercise, and behavioral therapy fail to achieve sustainable results, bariatric surgery emerges as a potent intervention for severe obesity and related comorbidities. One widely used surgical option is the gastric lap band, a minimally invasive adjustable device designed to restrict food intake and facilitate weight loss.
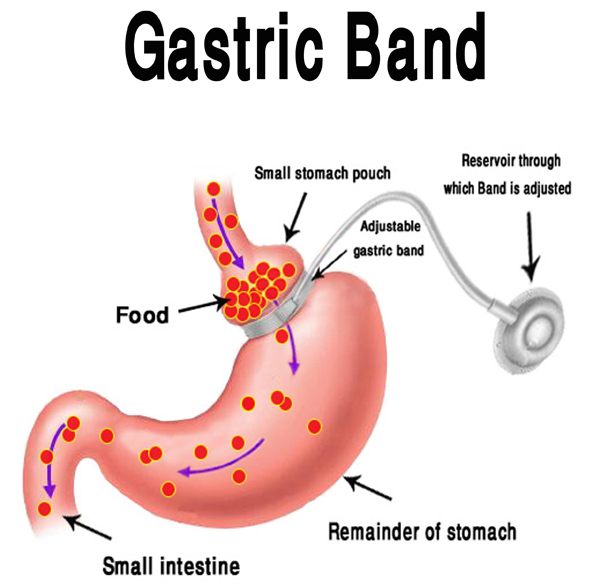
The gastric lap band procedure involves placing a silicone band around the upper portion of the stomach, creating a small pouch that limits food consumption and promotes early satiety. The band’s adjustability allows personalized control over the degree of restriction, optimizing outcomes and minimizing complications.
This article provides a comprehensive overview of gastric lap band This comprehensive guide delves into the underlying causes and risk factors leading to the use of gastric lap band surgery, clinical presentation and indications, detailed diagnostic workup, surgical options and techniques, postoperative care, potential complications, and strategies for living with and maintaining results after the procedure.
Underlying Causes Leading to Surgery
-
Morbid obesity: Defined as a body mass index (BMI) of 40 or higher, or 35+ with serious obesity-related health conditions such as type 2 diabetes, hypertension, obstructive sleep apnea, or cardiovascular disease.
-
Failure of conservative treatment: Inability to achieve or maintain weight loss through diet, exercise, medications, or behavioral changes.
-
Impact of obesity-related comorbidities: The presence of diabetes, joint disease, gastroesophageal reflux disease (GERD), fatty liver disease, and other conditions that impair quality and longevity of life.
-
Psychosocial challenges: Depression, low self-esteem, social isolation, and decreased mobility associated with obesity.
Risk Factors Predisposing to Morbid Obesity
-
Genetics and family history: Predisposition to weight gain and metabolic dysregulation.
-
Sedentary lifestyle and poor diet: High-calorie, nutrient-poor food intake combined with low physical activity.
-
Psychological factors: Emotional eating, stress, and certain psychiatric conditions.
-
Metabolic and hormonal disorders: Hypothyroidism, polycystic ovary syndrome (PCOS), insulin resistance.
-
Socioeconomic and environmental influences: Limited access to healthy food or safe exercise environments.
Candidates for gastric lap band surgery typically present with:
-
Excessive weight relative to height: BMI ≥40, or ≥35 with significant health problems.
-
Physical limitations: Reduced mobility, joint pain, difficulty performing daily activities.
-
Symptoms of comorbid conditions: Fatigue, dyspnea, nocturnal apnea, elevated blood sugar or blood pressure.
-
Psychological distress: Feelings of hopelessness, poor body image, social withdrawal.
-
Previous unsuccessful weight loss attempts: History of multiple failed diets or medical treatments.
-
Health screening findings: Abnormal labs or imaging related to obesity complications.
Comprehensive Medical and Psychological Assessment
-
Detailed history: Including obesity duration, previous interventions, family history, lifestyle habits, and psychological status.
-
Physical exam: BMI calculation, airway assessment, and evaluation of obesity-related sequelae.
-
Laboratory tests: CBC, comprehensive metabolic panel, lipid profile, HbA1c, thyroid function.
-
Cardiopulmonary evaluation: ECG, chest X-ray, sleep studies if indicated.
-
Imaging: Abdominal ultrasound to evaluate liver and gallbladder.
Nutritional and Behavioral Assessment
-
Dietary analysis and identification of eating behaviors.
-
Psychological evaluation to assess motivation and mental health.
-
Identification of contraindications such as untreated psychiatric illness or substance abuse.
Multidisciplinary Team Review
-
Input from bariatric surgeons, endocrinologists, dietitians, psychologists, and anesthesiologists.
-
Patient education on procedure, risks, benefits, lifestyle changes, and long-term commitment.
Surgical Technique Overview
-
The gastric lap band surgery is performed laparoscopically through 4-5 small incisions.
-
A silicone band is placed laparoscopically around the upper stomach, creating a small pouch that limits intake.
-
The band is connected via tubing to an access port implanted beneath the skin, allowing postoperative adjustments by adding or removing saline.
-
Surgery typically takes 45–60 minutes under general anesthesia.
-
Patients usually stay 1-2 days in hospital and return to normal activities within 1-2 weeks.
Mechanism of Action
-
The small stomach pouch fills quickly, triggering early satiety signals.
-
The adjustable band allows titration of restriction to balance hunger control and comfort.
-
Gradual weight loss is achieved through reduced caloric intake and altered eating habits.
Advantages of Gastric Lap Band
-
Minimally invasive with lower surgical risk than more extensive bariatric surgeries.
-
Adjustable and reversible.
-
No alteration of digestive tract or absorption.
-
Lower risk of nutritional deficiencies.
Comparison with Other Bariatric Surgeries
-
Gastric bypass: More rapid weight loss, but higher risk and complexity.
-
Sleeve gastrectomy: Permanent, removes part of stomach, not adjustable.
-
Biliopancreatic diversion: Malabsorptive, high complication risk.
Preoperative Preventive Measures
-
Smoking cessation to improve healing.
-
Control of comorbid conditions.
-
Nutritional optimization.
Postoperative Dietary Guidelines
-
Start with liquid diet progressing to pureed and then solid foods over weeks.
-
Small, frequent meals with emphasis on protein.
-
Avoidance of high-calorie liquids and carbonated beverages.
-
Chewing food thoroughly and eating slowly.
Lifestyle and Behavior Modifications
-
Regular physical activity adapted to patient’s capacity.
-
Psychological support for emotional eating.
-
Regular follow-ups with bariatric team.
Band Adjustment and Monitoring
-
Scheduled band fills or deflations based on symptoms and weight loss.
-
Monitoring for signs of band intolerance, reflux, or complications.
-
Lifelong commitment to medical surveillance.
Early Complications
-
Infection: At port site or surgical site.
-
Bleeding: Rare but possible.
-
Band slippage: Can cause obstruction, vomiting.
-
Anesthesia-related risks.
Late Complications
-
Band erosion: Implant migrates into stomach.
-
Esophageal dilation: Due to excessive restriction.
-
Gastroesophageal reflux disease (GERD).
-
Port problems: Leakage, dislocation, infection.
-
Nutritional deficiencies: Though less common than in bypass.
Managing Complications
-
Early recognition and intervention.
-
Imaging or endoscopy to confirm diagnosis.
-
Band removal or revision surgery in severe cases.
Adjusting to Life After Surgery
-
Understanding the role of the band as a tool, not a cure.
-
Commitment to dietary and behavioral changes.
-
Coping with body image changes and psychological adaptation.
Ongoing Medical Care
-
Regular consultations for band adjustments.
-
Nutritional assessments and supplementation.
-
Monitoring for weight loss progress and comorbidity resolution.
Psychological and Social Impact
-
Improved self-esteem and quality of life.
-
Support groups and counseling recommended.
-
Addressing challenges such as weight plateaus or emotional eating.
Long-Term Outcomes
-
Average excess weight loss of 40-60%.
-
Significant improvement in diabetes, hypertension, and sleep apnea.
-
Need for possible revisional surgery in some cases.
1. What is a gastric lap band?
A gastric lap band is an adjustable silicone band placed around the upper part of the stomach to create a small pouch, which limits food intake and promotes weight loss.
2. Who is a good candidate for gastric lap band surgery?
Ideal candidates are adults with a body mass index (BMI) of 40 or higher, or a BMI of 35+ with obesity-related health conditions such as diabetes or hypertension, who have struggled with other weight loss methods.
3. How is the gastric lap band procedure performed?
The surgery is minimally invasive and performed laparoscopically. The surgeon places an adjustable band around the stomach via small incisions, which reduces stomach capacity.
4. Is gastric lap band surgery safe?
Generally, it is considered safe with a lower risk compared to more invasive bariatric surgeries, but as with any surgery, there are risks such as infection, band slippage, or erosion.
5. How much weight can I expect to lose?
Patients typically lose about 40-50% of their excess body weight within 1 to 2 years after surgery, depending on adherence to diet and lifestyle changes.
6. How is the lap band adjusted?
The band is connected to a port under the skin. Saline can be added or removed through this port to tighten or loosen the band and control food intake.
7. What is the recovery time after surgery?
Most patients go home the same day or next day and return to normal activities within 1 to 2 weeks. Full recovery and adjustment period can take several weeks.
8. Are there dietary restrictions after lap band surgery?
Yes, patients must follow a specialized diet starting with liquids, progressing to pureed and then solid foods. Portion control and mindful eating are essential lifelong habits.
9. What are possible complications?
Complications may include band slippage, erosion, infection, acid reflux, or difficulty swallowing. Regular follow-ups are important to monitor and manage these risks.
10. Can the gastric lap band be removed?
Yes, the lap band is reversible and can be removed if necessary, but patients should discuss potential risks and benefits with their surgeon.
Gastric Lap Band
Many people across the world are now opting for Weight-loss surgeries. This definitely is not a solution for people who want a quick fix or who do not want to diet. Patients who undergo this surgery must adhere to a strict diet plan combined with a minimum of 30 minute exercise everyday after the surgery.
The other Weight loss surgeries that are commonly opted for are:
- Gastric Bypass Surgery- This is a procedure where the surgeon re-routes the digestive system which causes rapid weight loss
- Gastroplasty- This is a procedure where the surgeon re-routes the digestive system and also restricts the amount of food that is eaten by making the stomach smaller
Both the above said procedures are open surgeries where the doctor makes a five to six inch long incision with a 3-4 day stay at the Hospital. Neither of these procedures are reversible. A potential fatal complication involved when doing a Gastric Bypass and Gastroplasty is Anastomotic Leak. This leak happens at the staple line and is quite rare, happening in less than 2 percent of the cases.
A Gastric Lap Band Procedure on the other hand, is minimally invasive, performed by a laparoscope with small incisions and is completely reversible.
Procedure
The Gastric Lap band is a hollow band that is made of Sylastic. This is a kind of plastic that does not have any reactions to internal tissues. The band consists of an inflatable tube, which when filled with saline solution can be adjusted to change the size of the stomach pouch.
The procedure is done under General Anesthesia. Three to five small incisions (1.5-2 inches long) are made and with the help of a Laproscope the gastric lap band is placed around the Upper third portion of the stomach pouch. The band is adjusted through a small access port that is placed just under the skin. Saline solution is injected into the band through this port. These ports are available in various designs and are usually placed based on the preference of the bariatric surgeon. The positioning is usually done near the left rib margin.
When injecting the saline solution, a specialized needle should be used to avoid damage to the port. The port can either be sutured or stabled into place. Immediately after surgery the band is empty. After about 6 weeks the surgeon adds small amounts of saline. The amount of saline that is added will vary from one person to another.
This stoma or pouch that is created would be able to hold about 100-220grams of food during each meal. Once the pouch is full, the band slowly allows this food to be passed on to the lower portion of the stomach. Eventually, the procedure enables the patient to feel hungry less often, feel full more quickly and helps the patient to eat smaller portions of meal.
Associated Risks
The most significant complication that can occur is alteration of the stomach pouch, due to slippage of the band or stretching of the wall of the pouch. In addition there is always the risk of erosion of the band in the stomach.
Other risks include:
- Band leakage
- Reflux or vomiting
- Erosion of band into stomach
- Difficulty swallowing
- Enlargement of stomach pouch or band slippage
- Dehydration
- No weight loss
- Blockage of stomach outlet
- Gas bloat
- Nausea
- Constipation
- Ulceration
- Weight regain
- Gastritis
One of the main advantages of a Gastric Lap Band Surgery is that it can be reversed if any of the above complications become serious.
Recovery
Usually patients are able to return home the same day. However, some patients may be required to stay overnight at the hospital, depending on how they recover after the procedure.
It takes about 6 weeks for complete recovery.
Bariatric Surgeons usually give a planned customized diet plan for every patient. The pattern is such that a gradual increase in the intake of food is made over a period of several weeks. This is done to help the body to get accustomed to the new size and shape of the stomach pouch. This needs to be followed strictly to reduce discomfort and avoid potential side-effects.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


