Skin grafting is a vital surgical technique in reconstructive and plastic surgery used to replace damaged or missing skin by transplanting healthy skin from one part of the body (the donor site) to another (the recipient site). This procedure plays an essential role in treating severe burns, traumatic wounds, chronic ulcers, and surgical defects where the body’s ability to regenerate skin is limited or insufficient.
Skin grafts facilitate wound closure, protect underlying structures, prevent infection, reduce fluid loss, and help restore function and aesthetic appearance. The success of skin grafting depends on various factors including patient health, wound preparation, surgical technique, and postoperative care.
This comprehensive article explores the causes and risk factors necessitating skin grafts, clinical presentation, diagnostic steps, types and techniques of skin grafting, prevention and management strategies, possible complications, and living with and caring for grafts postoperatively.
Causes Requiring Skin Grafting
-
Thermal Burns: Deep partial-thickness and full-thickness burns destroying epidermis and dermis.
-
Traumatic Injuries: Including degloving injuries, large abrasions, avulsions, and crush wounds.
-
Surgical Resections: Post tumor excision, removal of necrotic or infected tissue.
-
Chronic Wounds and Ulcers: Pressure ulcers, diabetic foot ulcers, venous stasis ulcers resistant to conservative treatment.
-
Infections: Necrotizing soft tissue infections necessitating aggressive debridement.
-
Congenital and Acquired Defects: Such as large congenital nevi or scars requiring resurfacing.
Risk Factors Affecting Outcomes
-
Patient-Related: Diabetes mellitus, peripheral vascular disease, malnutrition, immunosuppression, smoking.
-
Wound-Related: Infection, poor vascular supply, excessive exudate, and inadequate debridement.
-
Graft-Related: Thickness of graft, size, and donor site morbidity.
-
Persistent Open Wounds: Failure to heal spontaneously over weeks to months.
-
Extensive Tissue Loss: Areas of skin loss exposing underlying muscle, fat, or bone.
-
Pain and Sensitivity: Due to exposed nerve endings in the wound bed.
-
Infection or Necrosis: Wound with purulent discharge, foul odor, or black necrotic tissue.
-
Functional Impairment: Limited joint mobility or risk of contracture.
-
Visible Disfigurement: Large scars or defects affecting appearance and quality of life.
Clinical Assessment
-
Detailed wound history, including etiology, duration, prior treatments.
-
Thorough examination assessing size, depth, vascularity, infection status, and surrounding skin.
-
Evaluation of patient’s overall health, nutritional status, and comorbidities.
Diagnostic Tools
-
Wound Cultures: To identify infection-causing organisms.
-
Doppler Ultrasonography: Evaluates blood flow in the recipient site.
-
Imaging: MRI or CT scan may be used for complex wounds to assess involvement of deeper tissues.
-
Laboratory Tests: Blood glucose, nutritional markers, and infection parameters.
Types of Skin Grafts
-
Split-Thickness Skin Graft (STSG): Harvests epidermis and a portion of dermis. Suitable for large wounds; donor site heals quickly but graft is thinner and more fragile.
-
Full-Thickness Skin Graft (FTSG): Includes epidermis and entire dermis, used for smaller, cosmetically sensitive areas; provides superior durability and texture but donor site requires primary closure.
-
Composite Grafts: Include skin and underlying structures like cartilage; used for complex reconstructions.
Harvesting Techniques
-
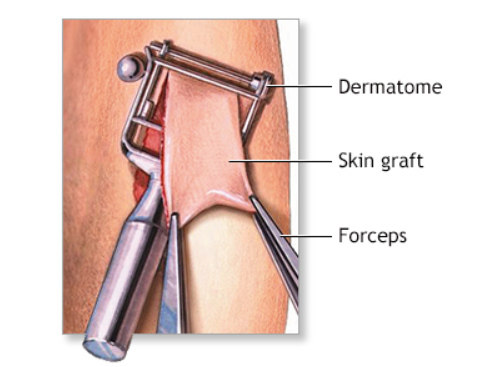
Dermatome: Instrument used to obtain thin, uniform grafts.
-
Free-Hand Technique: Manual excision with scalpel for small grafts.
Graft Preparation and Application
-
Meticulous preparation of recipient site with debridement of necrotic tissue.
-
Ensuring hemostasis to prevent hematoma formation beneath graft.
-
Securing graft using sutures, staples, or fibrin glue.
-
Application of appropriate dressings to maintain moisture and immobilization.
Adjunct Therapies
-
Negative Pressure Wound Therapy (NPWT): Enhances graft adherence by applying suction to remove exudate and promote blood flow.
-
Hyperbaric Oxygen Therapy: Used in selected cases to improve oxygen delivery and wound healing.
Preoperative Optimization
-
Control of diabetes, nutrition correction, cessation of smoking.
-
Treat underlying infections with antibiotics.
-
Patient education on procedure and postoperative care.
Intraoperative Strategies
-
Aseptic technique to minimize infection.
-
Adequate graft thickness and proper donor site selection.
-
Gentle handling of graft to preserve viability.
Postoperative Care
-
Immobilization of graft site to prevent shear forces.
-
Regular inspection and dressing changes under sterile conditions.
-
Pain management and prevention of infection.
-
Physiotherapy to prevent joint stiffness when applicable.
Early Complications
-
Graft Failure: Due to hematoma, infection, or insufficient vascularity.
-
Infection: Localized or spreading; requires prompt treatment.
-
Seroma or Hematoma: Fluid collections lifting graft from recipient bed.
-
Pain and Discomfort: At donor and recipient sites.
Late Complications
-
Scarring and Contractures: Affecting function and appearance.
-
Pigmentary Changes: Hypopigmentation or hyperpigmentation.
-
Donor Site Morbidity: Persistent pain, infection, or scarring.
-
Graft Breakdown: Due to trauma or poor integration.
Prevention of Complications
-
Experienced surgical technique.
-
Optimized patient health and wound bed preparation.
-
Strict postoperative protocols.
Healing and Recovery
-
Initial graft adherence visible within 5-7 days.
-
Complete epithelialization and maturation over weeks to months.
-
Donor site heals with minimal scarring when properly managed.
Functional and Aesthetic Outcomes
-
Improved protection of underlying tissues.
-
Restoration of skin continuity, reducing pain and infection risk.
-
Potential need for further procedures (scar revision, tissue expansion).
Long-Term Care and Monitoring
-
Protect grafted areas from trauma and excessive sun exposure.
-
Scar management using silicone gels, massage, or laser therapy.
-
Regular follow-ups to monitor skin integrity.
-
Psychological support when needed due to cosmetic or functional concerns.
1. What is a skin graft?
A skin graft is a surgical procedure where skin is removed from one area of the body (donor site) and transplanted to another area (recipient site) to repair damaged or missing skin.
2. Why are skin grafts needed?
Skin grafts are commonly used to treat severe burns, wounds, infections, surgical removal of skin cancers, or other injuries where the skin cannot heal naturally.
3. What types of skin grafts are there?
There are two main types: split-thickness grafts (which include the top layers of skin) and full-thickness grafts (which include the entire epidermis and dermis). The choice depends on the wound and location.
4. How is a skin graft procedure performed?
The surgeon removes healthy skin from the donor site, prepares the recipient site, and places the graft on the wound. The graft is then secured with stitches or staples and covered with dressings.
5. Is the skin graft procedure painful?
The procedure is performed under anesthesia, so pain during surgery is minimized. Post-operative pain is managed with medications, and the donor and graft sites may feel sore during healing.
6. How long does it take for a skin graft to heal?
Healing times vary but generally take 2 to 4 weeks for the graft to fully attach and for both donor and recipient sites to heal.
7. Are there risks or complications with skin grafts?
Risks include infection, graft failure, scarring, color mismatch, and poor healing. Proper care and monitoring are essential to minimize these risks.
8. Will the grafted skin look like the surrounding skin?
Initially, the graft may appear different in color and texture but often improves over time. However, some differences may persist permanently.
9. How do I care for the graft and donor sites after surgery?
Follow your surgeon’s instructions closely, keep the area clean and dry, avoid strenuous activity, and attend all follow-up appointments for wound care and monitoring.
10. Can skin grafts be used for cosmetic purposes?
While primarily for medical reasons, skin grafts can sometimes be used in reconstructive surgeries to improve appearance after trauma or cancer removal.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.

