Periodontics root planing is a fundamental and advanced dental procedure designed to treat periodontal disease by deeply cleaning the root surfaces of teeth to remove plaque, tartar (calculus), and bacterial toxins that cause gum inflammation and destruction of supporting tissues. As a cornerstone of periodontal therapy, root planing addresses infection below the gum line, promoting gum reattachment and preventing progression to severe periodontitis, which can result in tooth loss.
Periodontal disease is one of the most prevalent chronic inflammatory diseases worldwide, affecting millions of adults. Root planing, often combined with scaling, constitutes the non-surgical phase of periodontal treatment and aims to restore periodontal health by creating a clean environment that facilitates healing and reduces pocket depths.
This comprehensive guide covers the pathophysiology of periodontal disease, causes and risk factors necessitating root planing, clinical signs and symptoms, diagnostic methods, treatment techniques, preventive care, potential complications, and lifestyle considerations for patients undergoing root planing.
The Pathogenesis Behind Periodontal Disease
Periodontal disease is primarily caused by bacterial biofilms (plaque) accumulating on the teeth and below the gumline. These biofilms harbor pathogenic microorganisms that induce an inflammatory immune response, damaging the gingival tissues, periodontal ligament, and alveolar bone. If plaque is not disrupted, it calcifies into tartar, which acts as a reservoir for bacteria and cannot be removed by normal brushing.
Key Causes Necessitating Root Planing
-
Subgingival Plaque and Calculus Formation: The bacterial deposits beneath the gumline stimulate chronic inflammation and tissue destruction.
-
Poor Oral Hygiene: Ineffective plaque control facilitates bacterial colonization.
-
Smoking and Tobacco Use: Smoking impairs neutrophil function, decreases blood flow to gums, and exacerbates periodontal destruction.
-
Systemic Health Conditions: Diabetes mellitus, rheumatoid arthritis, and cardiovascular diseases are linked with increased susceptibility and severity of periodontal disease.
-
Genetic Predisposition: Family history can influence disease aggressiveness and response to therapy.
-
Hormonal Changes: Pregnancy, puberty, and menopause can heighten gingival sensitivity and inflammation.
-
Certain Medications: Drugs causing gingival enlargement complicate plaque removal.
-
Stress: Chronic stress can impair immune responses and wound healing.
-
Bleeding Gums: Spontaneous or provoked bleeding on brushing or flossing.
-
Gum Swelling and Redness: Inflammation causing tender, edematous gums.
-
Increased Pocket Depths: Formation of periodontal pockets exceeding 4mm detected clinically.
-
Gum Recession: Exposure of tooth roots causing sensitivity.
-
Halitosis: Persistent bad breath due to bacterial toxins.
-
Tooth Mobility or Migration: Resulting from loss of bone support.
-
Pus or Exudate: Infected pockets may discharge pus.
-
Pain or Discomfort: While early stages may be painless, advanced periodontitis can cause discomfort.
Clinical Periodontal Examination
-
Measurement of pocket depths with a calibrated periodontal probe at multiple sites per tooth.
-
Assessment of bleeding on probing as an indicator of inflammation.
-
Evaluation of clinical attachment loss and gingival recession.
-
Recording tooth mobility and furcation involvement.
Radiographic Assessment
-
Periapical and bitewing radiographs to evaluate alveolar bone levels and detect bone loss patterns.
-
Cone Beam Computed Tomography (CBCT) in complex cases for three-dimensional bone mapping.
Risk Assessment
-
Medical history to identify systemic conditions and lifestyle factors.
-
Microbial analysis or host-response testing in some advanced cases.
Scaling and Root Planing (SRP) Overview
-
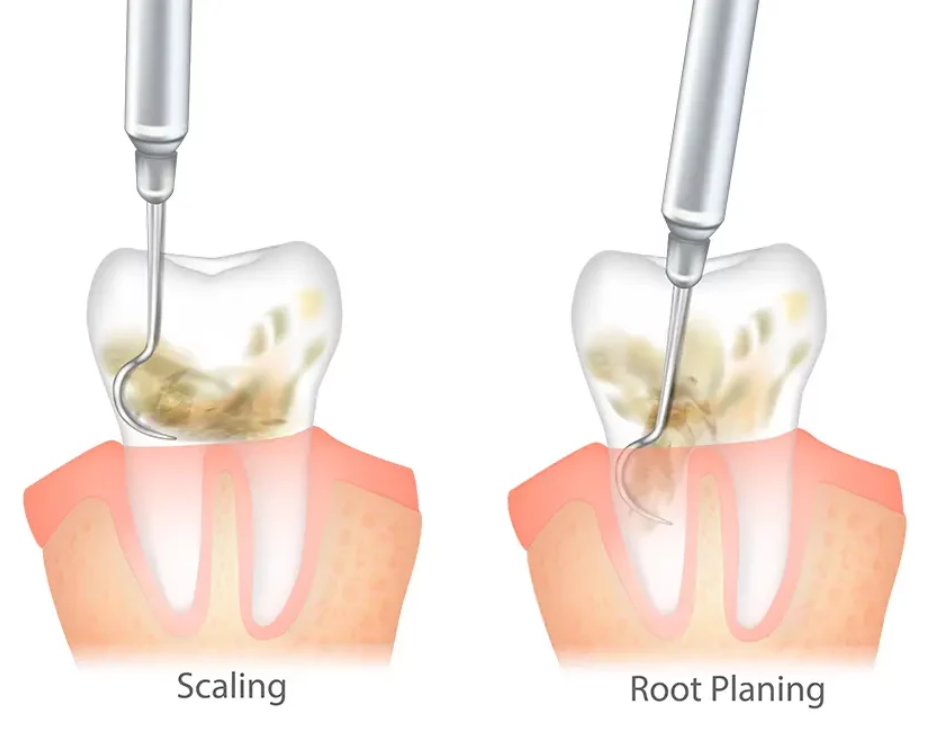
Scaling: Removal of supra- and subgingival plaque and calculus using manual scalers and ultrasonic devices.
-
Root Planing: Meticulous smoothing of root surfaces to eliminate bacterial endotoxins and create a biologically compatible surface conducive to tissue healing and reattachment.
-
Typically performed under local anesthesia to ensure patient comfort.
-
May require multiple sessions depending on disease severity and patient tolerance.
Adjunctive Treatments
-
Use of antimicrobial mouth rinses such as chlorhexidine gluconate to reduce bacterial load.
-
Systemic or localized antibiotic therapy in severe or refractory cases.
-
Emerging laser-assisted periodontal therapies providing enhanced bacterial reduction and improved healing.
Post-Procedure Follow-Up
-
Reevaluation 4-6 weeks post-treatment to assess healing and pocket depth reduction.
-
Consideration of surgical periodontal therapy if pockets remain deep.
Preventive Strategies
-
Rigorous oral hygiene regimen: twice-daily brushing with fluoridated toothpaste and daily interdental cleaning.
-
Regular professional dental cleanings every 3-6 months.
-
Smoking cessation counseling and support.
-
Nutritional optimization emphasizing antioxidants and vitamins for tissue repair.
-
Management of systemic diseases with healthcare provider collaboration.
Maintenance Phase
-
Supportive periodontal therapy involving ongoing monitoring and reinforcement of oral hygiene.
-
Patient education on recognizing early signs of disease recurrence.
Common Minor Complications
-
Temporary gum soreness and sensitivity to temperature or touch.
-
Mild bleeding or discomfort post-procedure.
-
Transient tooth sensitivity due to root exposure.
Less Common but Serious Complications
-
Inadequate removal of calculus leading to persistent infection.
-
Gingival recession resulting in aesthetic concerns and hypersensitivity.
-
Root surface damage if excessive instrumentation occurs.
-
Postoperative infection (rare with proper hygiene).
Adapting to Treatment
-
Patients may experience initial discomfort, which typically subsides within days.
-
Improvement in gum health and reduction in bleeding and inflammation often evident after a few weeks.
-
Commitment to meticulous oral hygiene is essential for sustained results.
Long-Term Outlook
-
Periodontal maintenance therapy critical for long-term tooth retention.
-
Early intervention prevents progression to tooth loss.
-
Positive impacts on systemic health, including potential benefits for cardiovascular disease management.
Psychological and Social Benefits
-
Enhanced self-confidence due to improved oral health and aesthetics.
-
Reduced anxiety related to dental health fears.
1. What is root planing in periodontics?
Root planing is a deep cleaning dental procedure aimed at removing plaque, tartar, and bacterial toxins from the root surfaces of teeth below the gumline. It smooths the roots to help gums reattach to the teeth and prevent further gum disease.
2. When is root planing recommended?
Root planing is recommended for patients diagnosed with periodontal (gum) disease, especially when pockets have formed between the teeth and gums due to infection or inflammation that cannot be treated with regular cleaning.
3. How is root planing different from scaling?
Scaling removes plaque and tartar from the tooth surfaces above and just below the gumline, while root planing focuses on cleaning and smoothing the root surfaces beneath the gums to promote healing.
4. Is root planing painful?
Root planing is usually performed under local anesthesia to minimize discomfort. Some patients may experience mild soreness or sensitivity after the procedure, which typically resolves within a few days.
5. How long does a root planing procedure take?
Treatment time varies depending on the extent of gum disease, but it usually requires one or more visits, each lasting 30 to 60 minutes, often divided by quadrants of the mouth.
6. What should I expect after root planing?
After treatment, gums may feel tender and slightly swollen. You might notice some bleeding or sensitivity, but these symptoms generally improve within a week. Maintaining good oral hygiene and following your dentist’s instructions is crucial for healing.
7. How effective is root planing in treating gum disease?
Root planing is highly effective in stopping the progression of periodontal disease when combined with good oral hygiene and regular dental visits. It helps reduce pocket depth and promotes gum reattachment.
8. Are there any risks or side effects of root planing?
Risks are minimal but can include temporary gum sensitivity, bleeding, or infection if aftercare is neglected. Proper technique and follow-up care help minimize these risks.
9. How do I care for my gums after root planing?
Follow your dentist’s recommendations for brushing gently with a soft toothbrush, using antimicrobial mouthwash if prescribed, avoiding smoking, and attending follow-up appointments for monitoring and additional cleanings.
10. Can root planing prevent tooth loss?
Yes, by removing bacteria and toxins that cause gum disease and bone loss, root planing helps preserve the supporting structures of teeth, significantly reducing the risk of tooth loss.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


