Hearing loss can significantly impact communication, social interaction, education, and overall quality of life. For individuals with severe to profound sensorineural hearing loss who derive limited benefit from traditional hearing aids, cochlear implants provide a revolutionary treatment option. Unlike hearing aids that amplify sounds, cochlear implants bypass damaged hair cells in the cochlea and directly stimulate the auditory nerve, enabling the brain to perceive sound.
Since their introduction in the late 20th century, cochlear implants have evolved with remarkable advancements in technology and surgical techniques, resulting in improved hearing outcomes and quality of life for both children and adults. This device has opened doors to spoken language development in congenitally deaf children and restored sound perception in adults who lost hearing.
This comprehensive guide explores the causes and risk factors associated with cochlear implant candidacy, symptoms prompting evaluation, diagnostic processes, treatment modalities, prevention and ongoing management, potential complications, and the realities of living with a cochlear implant.
Underlying Causes of Hearing Loss Addressed by Cochlear Implants
-
Congenital Hearing Loss:
Many infants are born with sensorineural hearing loss due to genetic mutations (e.g., connexin 26), prenatal infections (e.g., CMV), or developmental anomalies of the inner ear. -
Acquired Hearing Loss:
-
Ototoxicity: Caused by certain antibiotics (aminoglycosides), chemotherapy agents, or high-dose aspirin.
-
Noise-Induced Hearing Loss: Chronic exposure to loud noise damaging hair cells irreversibly.
-
Infections: Meningitis and chronic otitis media can cause cochlear damage.
-
Presbycusis: Age-related degeneration affecting hair cells and nerve fibers.
-
Trauma: Head injury causing cochlear nerve damage.
-
-
Auditory Neuropathy Spectrum Disorder (ANSD):
Disorder of neural transmission where cochlear implants may be beneficial despite preserved outer hair cell function. -
Sudden Sensorineural Hearing Loss:
If irreversible and severe, cochlear implantation can be considered.
Risk Factors Increasing Likelihood of Hearing Loss and Implantation
-
Family history of deafness or hearing disorders.
-
Prematurity or neonatal intensive care unit (NICU) admission.
-
Maternal infections during pregnancy.
-
Exposure to environmental toxins or loud noises.
-
Ototoxic drug use.
-
Recurrent or chronic ear infections.
-
In Infants and Children:
-
Failure to respond to sounds or voices.
-
Delayed speech and language development compared to milestones.
-
Lack of startle response to loud noises.
-
-
In Adults:
-
Severe difficulty understanding speech, even with hearing aids.
-
Social withdrawal due to communication barriers.
-
Progressive hearing loss despite amplification.
-
-
Additional Signs:
-
Difficulty hearing in noisy environments.
-
Tinnitus or ringing sensations.
-
Balance problems or dizziness may accompany hearing loss.
-
Early identification of these symptoms is critical, particularly in children, to enable timely intervention and avoid lifelong communication delays.
Audiological Evaluation
-
Pure Tone Audiometry:
To quantify hearing loss severity. -
Speech Recognition Tests:
Assess understanding of speech, crucial for candidacy. -
Hearing Aid Trial:
To evaluate benefit and confirm implant necessity.
Imaging Studies
-
CT Scan of Temporal Bone:
To examine cochlear anatomy, ossification, and auditory nerve presence. -
MRI:
Provides detail of the cochlear nerve and brainstem structures.
Additional Assessments
-
Auditory Brainstem Response (ABR) Testing:
Objective hearing assessment, especially in infants or non-responsive patients. -
Multidisciplinary Evaluation:
Involving ENT surgeons, audiologists, speech-language pathologists, and psychologists to ensure candidacy suitability. -
Medical Clearance:
Assessing overall health for anesthesia and surgery.
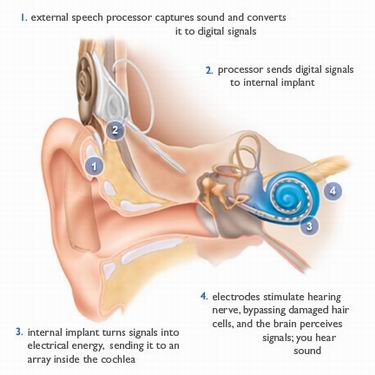
Device Components
-
External: Microphone, speech processor, transmitter coil worn behind the ear.
-
Internal: Receiver-stimulator implanted under the skin and electrode array inserted into the cochlea.
Surgical Procedure
-
Typically performed under general anesthesia.
-
Approximately 2-3 hours surgery with a small incision behind the ear.
-
Electrode insertion is performed with precision to preserve residual hearing where possible.
-
Hospital stay usually brief, outpatient or 1-2 days inpatient.
Postoperative Activation and Rehabilitation
-
Implant activation occurs 2-4 weeks after surgery.
-
Initial mapping to program the device according to patient’s auditory thresholds.
-
Ongoing auditory-verbal therapy to develop listening and speech skills.
-
Frequent follow-up appointments for re-mapping and progress evaluation.
Preventive Measures
-
Newborn Hearing Screening Programs: Critical for early detection.
-
Avoidance of Risk Factors: Protect against noise exposure and ototoxic medications.
-
Prompt Treatment of Ear Infections: To reduce cochlear damage.
Post-implantation Management
-
Commitment to rehabilitation programs for optimal speech and hearing outcomes.
-
Routine device maintenance and troubleshooting.
-
Protection of implant area from trauma and water exposure.
-
Psychological support to aid adjustment and social integration.
Surgical Complications
-
Infection at the implant site.
-
Facial nerve injury (rare).
-
Device failure or electrode misplacement.
-
Taste disturbances due to chorda tympani nerve involvement.
Long-Term Complications
-
Skin irritation or breakdown over implant.
-
Device malfunction requiring revision surgery.
-
Loss of residual natural hearing.
-
Vestibular symptoms like dizziness.
Managing Complications
-
Early recognition and treatment.
-
Device reprogramming or replacement.
-
Multidisciplinary approach for vestibular or psychological symptoms.
Hearing Outcomes
-
Most recipients achieve significant improvements in sound detection and speech understanding.
-
Early implantation, especially in children, correlates with better language acquisition.
-
Outcomes depend on age at implantation, duration of deafness, and rehabilitation.
Lifestyle Adjustments
-
MRI compatibility: modern implants allow safe scanning with precautions.
-
Avoidance of activities risking implant damage; use protective gear when needed.
-
Awareness of electromagnetic interference (e.g., security systems).
Social and Psychological Impact
-
Improved communication fosters social integration and educational success.
-
Support groups and counseling enhance coping and motivation.
-
Continuous engagement in auditory training maximizes benefits.
1. What is a cochlear implant?
A cochlear implant is a medical device designed to provide a sense of sound to individuals with severe to profound hearing loss by bypassing damaged parts of the ear and directly stimulating the auditory nerve.
2. Who is a candidate for a cochlear implant?
Candidates include adults and children with severe to profound sensorineural hearing loss who receive limited or no benefit from conventional hearing aids.
3. How does a cochlear implant work?
The implant consists of an external microphone and processor that capture sound and convert it into electrical signals, which are transmitted to the internal implant. The implant stimulates the auditory nerve, allowing the brain to interpret these signals as sound.
4. What is the cochlear implant surgery like?
The surgery is typically performed under general anesthesia and takes about 2 to 4 hours. It involves placing the internal device under the skin behind the ear and threading an electrode array into the cochlea.
5. Is cochlear implant surgery painful?
Patients are under anesthesia during the procedure and usually experience mild discomfort afterward, which can be managed with pain medication.
6. How long is the recovery period after surgery?
Most patients recover within a few weeks. The external processor is typically activated a few weeks after surgery once healing is complete.
7. What is the success rate of cochlear implants?
Cochlear implants have a high success rate, with many recipients experiencing significant improvement in hearing and speech understanding.
8. Are there any risks or complications associated with cochlear implants?
Risks include infection, device malfunction, facial nerve injury, and dizziness. However, serious complications are rare.
9. How do I prepare for cochlear implant surgery?
Preparation includes a comprehensive hearing evaluation, imaging studies, medical clearance, and counseling about expectations and postoperative rehabilitation.
10. What kind of rehabilitation is required after implantation?
Postoperative rehabilitation involves auditory training and speech therapy to help the brain adapt to new hearing signals and improve communication skills.
The other ENT Procedures are:
Few Popular Hospitals for Cochlear Implant are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Choclear Implant | Doctors For Choclear Implant | Cost For Choclear Implant | Treatment For Choclear Implant | Destinations For Choclear Implant | Risks Choclear Implant | Choclear Implant In India | Choclear Implant Recovery | Choclear Implant Information | Choclear Implant Thailand | Choclear Implant In Malaysia | Choclear Implant Abroad | Choclear Implant Overseas | Choclear Implant Low Cost | Choclear Implant In Singapore | Choclear Implant In Argentina | Surgery Choclear Implant | Choclear Implant In Singapore General Hospital | Choclear Implant In Apollo Hospitals | Bionic Ear | Speech Processing Equipment | Auditory Nerve | Cochlea | Side Effects Of Choclear Implant
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



