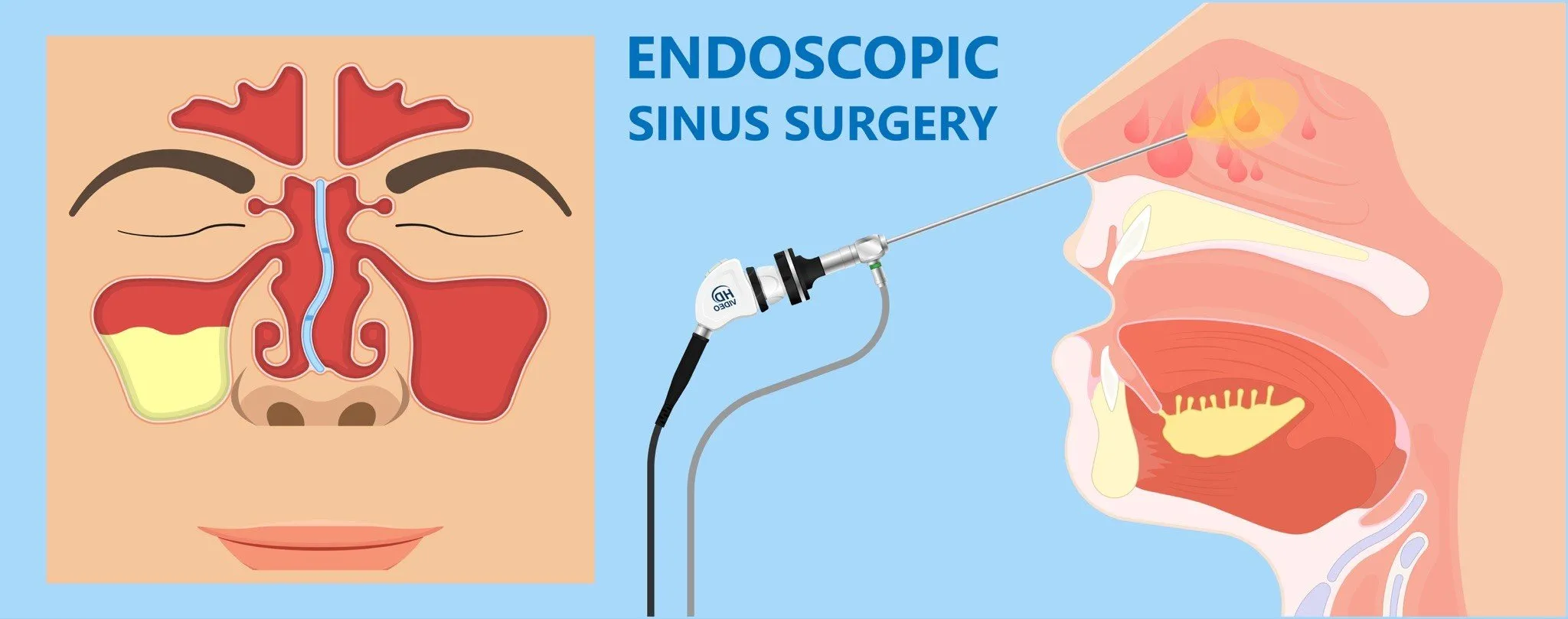
Functional Endoscopic Sinus Surgery (FESS) has become the gold standard surgical treatment for patients suffering from chronic and recurrent sinus diseases that do not respond adequately to medical management. It is a minimally invasive technique that uses an endoscope—a thin tube equipped with a camera and light—to access the sinuses via the nasal passages. This method avoids external incisions and allows the surgeon to visualize and operate on the sinuses with precision.
The primary goal of FESS is to restore normal sinus ventilation and drainage by removing obstructions such as inflamed mucosa, nasal polyps, or anatomical abnormalities, while preserving as much healthy tissue as possible. This surgery improves symptoms like nasal congestion, facial pain, headaches, and recurrent infections, thereby significantly enhancing the patient’s quality of life.
With advancements in technology and a deeper understanding of sinus physiology and anatomy, FESS has evolved into a highly effective and safe procedure with excellent outcomes. This guide will provide an extensive overview of FESS, including causes and risk factors, clinical presentation, diagnostic approaches, treatment methods, preventive strategies, potential complications, and post-surgical life considerations.
Underlying Causes Leading to FESS
-
Chronic Rhinosinusitis (CRS):
Characterized by inflammation of the nasal and paranasal sinus mucosa lasting more than 12 weeks. CRS often involves mucosal swelling, polyps, and persistent obstruction of sinus drainage pathways. -
Nasal Polyposis:
Growth of edematous mucosal tissue that blocks sinus ostia, commonly associated with allergic rhinitis, asthma, or aspirin sensitivity. -
Recurrent Acute Sinusitis:
Multiple episodes of acute sinus infection that do not resolve fully or recur frequently despite treatment. -
Anatomical Obstructions:
Deviated nasal septum, enlarged turbinates, concha bullosa (pneumatized middle turbinate), and narrow osteomeatal complexes that predispose to impaired sinus drainage. -
Fungal Sinusitis:
Both allergic fungal sinusitis and invasive fungal infections can cause chronic sinus disease. -
Mucoceles:
Mucus-filled cysts arising from obstructed sinuses that cause expansion and bone erosion. -
Sinonasal Tumors:
Benign or malignant lesions obstructing sinus drainage. -
Failure of Previous Medical or Surgical Treatments:
Persistent symptoms following conservative management or prior surgeries.
Risk Factors Enhancing Disease Development
-
Allergic rhinitis and other atopic conditions.
-
Cigarette smoking, which impairs mucociliary clearance.
-
Exposure to environmental pollutants and irritants.
-
Asthma, especially aspirin-exacerbated respiratory disease (AERD).
-
Immunosuppression or systemic inflammatory diseases.
-
Poor nasal hygiene and delayed treatment of infections.
Patients who may benefit from FESS often present with a constellation of symptoms reflecting impaired sinus drainage and chronic inflammation:
-
Nasal Obstruction or Congestion:
Persistent blockage that affects breathing through the nose. -
Facial Pressure or Pain:
Particularly over the forehead, cheeks, or between the eyes, often worsening with bending forward. -
Postnasal Drip:
Constant mucus drainage down the back of the throat causing cough or throat irritation. -
Chronic Nasal Discharge:
Thick, often colored secretions due to bacterial superinfection. -
Reduced or Loss of Smell (Hyposmia or Anosmia):
Frequently accompanies nasal polyps or mucosal swelling. -
Headaches:
Particularly frontal or retro-orbital, sometimes misdiagnosed as migraines. -
Fatigue and Malaise:
Due to chronic inflammation and disrupted sleep from nasal obstruction. -
Recurrent Sinus Infections:
Frequent bouts of acute sinusitis with incomplete resolution. -
Visual Symptoms:
Rare, but swelling near the eyes or orbital pain may indicate extensive disease. -
On nasal endoscopy: visible polyps, purulent discharge, mucosal edema, and anatomical variations blocking sinus openings.
Comprehensive Clinical Evaluation
-
A detailed medical history emphasizing duration, severity, and response to prior therapies.
-
Physical examination focusing on nasal cavity and sinuses using anterior rhinoscopy.
-
Nasal endoscopy performed by an ENT specialist to visualize nasal mucosa, polyps, and sinus ostia directly, evaluate mucopurulent secretions, and identify anatomic obstructions.
Imaging Studies
-
Computed Tomography (CT) Scan of the Paranasal Sinuses:
This remains the gold standard for surgical planning. It delineates sinus anatomy, extent of mucosal disease, anatomical variants, bony erosions, and helps identify contraindications such as skull base defects. -
Magnetic Resonance Imaging (MRI):
Used selectively to evaluate soft tissue involvement in suspected tumors or fungal disease.
Ancillary Investigations
-
Allergy testing to identify atopic triggers contributing to inflammation.
-
Microbiological cultures when infection is refractory to antibiotics.
-
Blood tests for systemic inflammatory markers or autoimmune causes.
-
Pulmonary function tests if coexistent asthma is suspected.
Medical Management as the First Step
-
Topical Nasal Steroids: To reduce mucosal inflammation and polyp size.
-
Saline Nasal Irrigation: Promotes mucociliary clearance and moisturizes mucosa.
-
Antibiotics: Used for bacterial exacerbations, guided by culture when possible.
-
Systemic Steroids: Short courses may provide relief in severe inflammation.
-
Antihistamines and Leukotriene Modifiers: For allergic inflammation control.
When to Consider FESS
-
Failure of optimal medical therapy after several weeks to months.
-
Persistent significant symptoms impacting quality of life.
-
Evidence of obstructed sinuses on imaging.
-
Presence of nasal polyps unresponsive to medical treatment.
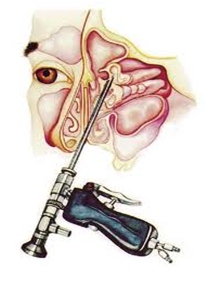
The Surgical Procedure
-
Performed under general anesthesia in a sterile operating room.
-
Surgeon uses an endoscope inserted through the nostrils to access the sinuses.
-
Removal of diseased ethmoid air cells, polypectomy, and widening of natural sinus openings.
-
Preservation of healthy mucosa and critical structures such as the skull base and orbit.
-
Concurrent correction of anatomic variations such as deviated septum if needed.
-
Surgery duration varies from 30 minutes to 2 hours depending on extent.
Postoperative Management
-
Regular nasal saline rinses to prevent crusting and promote healing.
-
Continued use of topical steroids to maintain mucosal health.
-
Follow-up endoscopic debridement sessions to remove crusts and debris.
-
Monitoring for symptom improvement and early detection of complications.
Preventive Strategies
-
Rigorous control of allergies through medications and avoidance.
-
Smoking cessation and reducing exposure to pollutants.
-
Prompt treatment of upper respiratory infections.
-
Maintaining nasal hygiene with daily saline irrigations.
Long-Term Management
-
Lifelong use of topical corticosteroids may be necessary.
-
Regular ENT follow-ups for early identification of disease recurrence.
-
Management of associated comorbidities such as asthma.
-
Patient education about recognizing early signs of sinus infection.
While FESS is generally safe and effective, potential complications include:
Common Minor Complications
-
Temporary nasal bleeding and crusting.
-
Nasal dryness or irritation.
-
Mild postoperative pain and congestion.
Rare but Serious Complications
-
Orbital Injury: Due to close proximity to the eyes, may cause hematoma, vision changes, or diplopia.
-
Cerebrospinal Fluid (CSF) Leak: From skull base breach; requires urgent management.
-
Infection: Postoperative sinus or intracranial infections.
-
Adhesion Formation: Scar tissue that can cause nasal blockage.
-
Persistent or Recurrent Disease: Sometimes necessitating revision surgery.
-
Anesthesia Risks: Including allergic reactions or cardiopulmonary complications.
Early recognition and appropriate management of complications are critical to prevent long-term sequelae.
Recovery Expectations
-
Nasal congestion and mild discomfort generally persist for 1-3 weeks.
-
Gradual improvement of sinus symptoms over 6-12 weeks.
-
Regular saline nasal irrigations and topical steroids essential during healing.
-
Return to normal activities usually within 1-2 weeks, avoiding strenuous exertion initially.
Long-Term Outlook
-
Majority of patients experience significant symptom relief and reduced frequency of sinus infections.
-
Some require maintenance therapy to prevent recurrence.
-
Close collaboration with ENT specialists for ongoing care.
Lifestyle and Quality of Life
-
Avoidance of smoking and nasal irritants.
-
Continued allergy management.
-
Use of humidifiers in dry environments.
-
Awareness and prompt treatment of sinus infections to prevent relapse.
-
Psychological support when chronic disease affects quality of life.
1. What is Functional Endoscopic Sinus Surgery (FESS)?
FESS is a minimally invasive surgical procedure used to restore normal drainage and function of the sinuses by removing blockages such as polyps, scar tissue, or inflamed mucosa through the use of an endoscope inserted via the nostrils.
2. Why is FESS performed?
It is performed to treat chronic sinusitis and other sinus conditions that do not respond to medical treatments such as antibiotics, nasal sprays, or steroids. FESS helps reduce sinus infections, improve breathing, and relieve symptoms like facial pain and congestion.
3. How is FESS performed?
The surgeon inserts a thin, flexible endoscope through the nostrils to view the sinus passages. Specialized instruments are then used to remove obstructions and open the sinus drainage pathways without external incisions.
4. Is FESS painful?
The surgery is done under general or local anesthesia, so patients do not feel pain during the procedure. Postoperative discomfort such as nasal congestion, mild pain, and swelling may occur but can be managed with medications.
5. What is the recovery time after FESS?
Recovery usually takes about 1 to 2 weeks. Patients may experience nasal congestion, drainage, and mild discomfort during this period and should follow postoperative care instructions closely.
6. Are there risks or complications associated with FESS?
While generally safe, risks include bleeding, infection, damage to nearby structures such as the eyes or brain, cerebrospinal fluid leak, and changes in smell. These complications are rare with experienced surgeons.
7. How should I prepare for FESS?
Preparation includes preoperative imaging (usually CT scans), medical evaluation, stopping blood thinners if advised, and following fasting instructions before surgery.
8. What should I expect after FESS?
After surgery, patients typically have nasal packing or splints, experience nasal congestion, mild pain, and drainage. Regular follow-up visits are important for nasal cleaning and monitoring healing.
9. Can FESS cure chronic sinusitis?
FESS significantly improves symptoms and sinus drainage, reducing the frequency and severity of infections. However, some patients may still require ongoing medical management.
10. How long do the benefits of FESS last?
Most patients experience long-term relief, but outcomes depend on the underlying condition and adherence to postoperative care and medical treatments.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.