Ossiculoplasty is a specialized surgical procedure designed to restore or repair the ossicular chain in the middle ear. The ossicular chain consists of three tiny bones—malleus (hammer), incus (anvil), and stapes (stirrup)—which transmit sound vibrations from the eardrum to the inner ear, where they are processed as auditory signals. When these ossicles are damaged due to infection, trauma, or congenital issues, hearing loss can result. Ossiculoplasty aims to reconstruct or repair the ossicular chain, thereby improving or restoring hearing function.
This procedure is performed when patients experience conductive hearing loss, a type of hearing loss that occurs due to mechanical problems in the middle ear. Ossiculoplasty can help treat conditions like chronic otitis media, cholesteatoma, and trauma to the ear, as well as congenital malformations.
In this article, we will explore the causes of ossicular damage, risk factors for undergoing ossiculoplasty, symptoms that indicate the need for surgery, diagnostic techniques, various treatment options, post-surgical management, and the potential complications and long-term recovery associated with this procedure.
Causes of Ossicular Chain Damage
Ossicular chain damage can be caused by various medical conditions, traumatic injuries, or congenital abnormalities. Below are the common causes leading to the need for ossiculoplasty:
-
Chronic Otitis Media (Chronic Ear Infections):
Chronic ear infections are one of the most common causes of ossicular damage. When the middle ear becomes infected repeatedly over a long period, the inflammation can erode or destroy the ossicles, leading to conductive hearing loss. This is particularly true when the infection spreads to the mastoid bone (mastoiditis), affecting the bones of the ear. -
Cholesteatoma:
A cholesteatoma is an abnormal skin growth that can develop in the middle ear. It often results from chronic infections and can cause progressive damage to the ossicular chain. If left untreated, cholesteatomas can erode the ossicles and the surrounding structures, making ossiculoplasty necessary. -
Trauma or Injury to the Ear:
Physical trauma to the ear, such as a blow to the head, skull fractures, or accidents involving the ear, can disrupt or fracture the ossicles. Severe ear trauma may require surgical reconstruction to restore hearing function. -
Congenital Abnormalities:
Some individuals are born with deformities or malformations in the ossicular chain, which can lead to conductive hearing loss. In such cases, ossiculoplasty may be needed to correct the structural defects and restore hearing. -
Barotrauma (Pressure Injury):
Sudden changes in atmospheric pressure, such as during flying, diving, or scuba diving, can cause barotrauma, which may damage the ossicles. This type of injury can result in hearing loss and may require surgical repair. -
Otosclerosis:
Otosclerosis is a condition characterized by abnormal bone growth around the stapes bone in the middle ear. The stapes can become immobilized, leading to conductive hearing loss. Surgery to replace the stapes with a prosthesis is often required.
Risk Factors
Several factors can increase the likelihood of ossicular damage, including:
-
Chronic Ear Infections:
Repeated ear infections or untreated otitis media can increase the risk of ossicular chain damage. -
Environmental Exposure:
Exposure to environmental toxins, loud noises, smoke, or allergens can contribute to inflammation in the middle ear and increase the risk of polyp or cholesteatoma formation. -
Age:
Age-related degenerative changes in the middle ear may lead to ossicular damage over time. This is particularly true for individuals who have a history of chronic ear conditions. -
Family History of Ear Problems:
A family history of otosclerosis, congenital malformations, or recurrent ear infections may predispose individuals to ossicular damage. -
Medical Conditions:
Conditions such as diabetes, immune system disorders, and certain genetic syndromes may increase the risk of developing conditions that affect the ossicular chain.
Ossicular chain dysfunction leads to conductive hearing loss, which is characterized by difficulty in transmitting sound from the outer ear to the inner ear. The severity of symptoms can range from mild hearing loss to complete deafness. Common symptoms that suggest the need for ossiculoplasty include:
-
Hearing Loss:
The primary symptom of ossicular damage is hearing loss, which may be gradual or sudden. Patients with ossicular damage may find it challenging to hear low sounds or struggle to understand speech, especially in noisy environments. -
Ear Fullness or Pressure:
A sensation of fullness or pressure in the ear, especially in cases of chronic ear infections, may indicate that the ossicular chain is damaged or not functioning properly. -
Chronic Otitis Media or Drainage:
Persistent ear infections or drainage from the ear are common symptoms that point to the presence of damaged ossicles, particularly in patients with chronic otitis media or cholesteatoma. -
Tinnitus (Ringing in the Ears):
Some patients with ossicular damage may experience tinnitus, a constant or intermittent ringing, buzzing, or humming sound in the ears. -
Dizziness or Balance Problems:
In rare cases, damage to the ossicles may also affect the vestibular system, leading to dizziness or balance problems. -
Visible Abnormalities or Trauma:
In cases of trauma, patients may notice visible changes in the ear or external injury to the ear canal or eardrum.
The diagnosis of ossicular damage involves a combination of clinical examination, medical history review, hearing tests, and imaging studies. The goal is to identify the underlying cause of hearing loss and assess the extent of ossicular damage.
Clinical Evaluation
-
Patient History:
The doctor will inquire about the patient's symptoms, ear infections, previous trauma, and family history of hearing loss or ear problems. -
Physical Examination:
A thorough examination of the ear canal and eardrum will be performed. The doctor will check for any signs of infection, perforation, or structural abnormalities.
Hearing Tests
-
Audiometry:
A hearing test (audiogram) is used to assess the degree of hearing loss. Conductive hearing loss, which is typically caused by problems in the middle ear, will be observed in patients with ossicular damage. -
Tympanometry:
Tympanometry tests the movement of the eardrum in response to changes in air pressure, which helps assess the function of the middle ear.
Imaging Studies
-
CT Scan:
A high-resolution CT scan of the temporal bone is often performed to evaluate the ossicular chain's condition and identify any abnormalities, fractures, or structural issues. -
MRI (Magnetic Resonance Imaging):
An MRI may be used in cases where soft tissue or cholesteatoma is suspected, providing a detailed image of the middle ear and surrounding structures.
Biopsy
-
Tissue Biopsy:
In rare cases, a biopsy may be performed to determine whether there is any cancerous or abnormal tissue present.
The treatment approach for ossicular damage depends on the severity of the damage, the underlying cause, and the patient's overall health. Treatment options include both surgical and non-surgical interventions.
Non-Surgical Treatments
-
Hearing Aids:
For patients with mild to moderate conductive hearing loss, hearing aids may be recommended. Hearing aids amplify sound, helping patients hear better and improving communication. -
Medications:
In cases of infection or inflammation, medications such as antibiotics, corticosteroids, or decongestants may be prescribed to reduce inflammation and prevent further damage to the ossicles.
Surgical Treatments
-
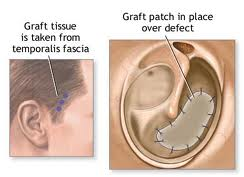
Ossiculoplasty (Ossicular Reconstruction):
The main surgical treatment for damaged ossicles is ossiculoplasty, which involves reconstructing or repairing the ossicular chain. This is done using prostheses, grafts, or by repositioning the existing ossicles. -
Stapedectomy (for Otosclerosis):
For patients with otosclerosis, a stapedectomy may be performed, where the stapes bone is replaced with a prosthetic to restore hearing. -
Myringoplasty and Tympanoplasty:
These procedures may be performed in conjunction with ossiculoplasty to repair a perforated eardrum, often in cases of chronic otitis media. -
Cholesteatoma Removal:
If a cholesteatoma is present, it must be removed during the surgery to prevent further damage to the ossicles and surrounding tissues.
Prevention Strategies
Although ossicular damage can be difficult to prevent, some steps can reduce the risk:
-
Manage Ear Infections:
Prompt treatment of ear infections, especially chronic otitis media, can help reduce the risk of ossicular damage. -
Avoid Trauma to the Ear:
Protecting the ear from injury, such as using ear protection during sports or avoiding exposure to loud noises, can help prevent trauma to the ossicles. -
Quit Smoking:
Smoking exacerbates ear infections and can contribute to the development of otitis media and other middle ear conditions. -
Manage Allergies and Asthma:
Effective control of allergies and asthma can help prevent inflammation in the middle ear and sinuses, reducing the risk of ossicular damage.
Postoperative Care
-
Follow-up Visits:
Regular follow-up visits with the ENT specialist are necessary to monitor healing and ensure the success of the surgery. -
Avoid Strenuous Activities:
Patients should avoid heavy lifting and activities that increase pressure in the ear during the recovery period. -
Speech and Hearing Rehabilitation:
In some cases, patients may benefit from speech therapy or auditory rehabilitation to optimize hearing post-surgery.
While ossiculoplasty is generally safe, there are potential complications:
-
Infection:
Infections are a rare but possible complication that may require antibiotics. -
Bleeding:
Minor bleeding is common, but major bleeding is unusual with skilled surgical techniques. -
Failure of the Prosthesis:
Sometimes, the prosthetic ossicles can fail or become displaced, requiring revision surgery. -
Hearing Loss Recurrence:
In some cases, the patient may experience a return of hearing loss, requiring additional interventions. -
Tinnitus (Ringing in the Ears):
Temporary or permanent ringing in the ear may occur after surgery.
After ossiculoplasty, most patients experience improved hearing and quality of life. However, there are several aspects of long-term care:
-
Hearing Improvement:
Most patients see a significant improvement in hearing after surgery. In some cases, hearing aids may still be necessary for optimal results. -
Lifestyle Adjustments:
Adopting a healthy lifestyle and avoiding smoking and ear infections can help maintain long-term success. -
Regular Checkups:
Ongoing follow-ups with an ENT specialist are essential to ensure continued healing and early detection of any issues.
1. What is ossiculoplasty?
Ossiculoplasty is a surgical procedure used to repair or reconstruct the ossicles, which are the three small bones (malleus, incus, and stapes) in the middle ear that transmit sound vibrations to the inner ear. The surgery is typically performed when these bones are damaged due to chronic ear infections, trauma, or congenital issues.
2. Why is ossiculoplasty performed?
Ossiculoplasty is primarily performed to improve hearing in patients with conductive hearing loss caused by damage to the ossicles. Conditions like chronic otitis media (middle ear infection), cholesteatoma, or trauma can result in the destruction of these bones, leading to hearing impairment.
3. How is ossiculoplasty performed?
The procedure involves accessing the middle ear through the ear canal or behind the ear. The damaged ossicles are either repaired or replaced with prosthetic implants made of materials like titanium, ceramic, or plastic. The surgery aims to restore the sound transmission pathway and improve hearing.
4. Is ossiculoplasty painful?
The surgery is performed under general anesthesia, so patients do not feel pain during the procedure. Post-surgery, some mild discomfort, pain, or pressure in the ear may occur, but this can usually be managed with medications.
5. How long does ossiculoplasty take?
The procedure generally takes 1 to 2 hours, depending on the complexity of the damage and whether additional procedures, such as tympanoplasty (eardrum repair), are required.
6. What is the recovery time after ossiculoplasty?
Recovery time varies depending on the individual and the extent of the surgery. Most patients can return to normal activities within 1 to 2 weeks. However, it may take a few months for the hearing improvement to stabilize. Follow-up visits are crucial for monitoring healing.
7. Are there risks or complications associated with ossiculoplasty?
As with any surgery, risks include infection, bleeding, hearing loss, dizziness, or damage to surrounding structures like the facial nerve. Prosthetic implants may also become displaced or fail to function as intended. These complications are rare, and the procedure is generally safe.
8. How should I prepare for ossiculoplasty?
Preparation includes a thorough medical evaluation, hearing tests, and imaging studies (such as a CT scan) to assess the condition of the ossicles and the middle ear. You may also need to stop taking certain medications, such as blood thinners, before surgery.
9. How successful is ossiculoplasty in improving hearing?
Ossiculoplasty is highly successful in improving hearing in many cases. Success rates can vary based on factors like the extent of ossicle damage, the type of prosthesis used, and the patient’s overall ear health. Most patients experience significant improvement in hearing after surgery.
10. How can I prevent the need for ossiculoplasty in the future?
To prevent ossicle damage, it is important to address ear infections promptly, maintain good ear hygiene, and protect the ears from trauma. Regular check-ups with an ENT specialist can help monitor ear health and prevent complications that may lead to hearing loss.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


