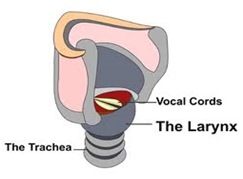
Thyroplasty is a type of voice surgery used to treat voice disorders caused by structural problems in the larynx (voice box). The procedure is commonly used to treat conditions such as vocal cord paralysis, vocal cord atrophy, and other disorders that affect the movement or function of the vocal cords. The goal of thyroplasty is to improve or restore the patient’s voice by improving vocal cord function or restoring vocal cord position.
In many cases, thyroplasty is recommended when non-surgical treatments (like speech therapy or voice rest) have not provided sufficient results. The surgery is designed to correct the position of the vocal cords and help optimize airflow, allowing patients to speak more clearly and naturally.
Thyroplasty is typically performed under local or general anesthesia, depending on the specific type of surgery and the patient's health. It can be a life-changing procedure for individuals who have suffered from voice disorders for an extended period.
Causes of Voice Disorders Leading to Thyroplasty
Thyroplasty is often required when a patient has a condition that directly affects the function or position of the vocal cords. These conditions include:
-
Vocal Cord Paralysis:
Vocal cord paralysis is one of the most common causes of voice disorders requiring thyroplasty. This condition occurs when one or both vocal cords fail to move properly, often due to nerve damage. Vocal cord paralysis can result from surgery (such as thyroid surgery), trauma, viral infections, or neurological disorders. -
Vocal Cord Atrophy:
Over time, the muscles of the vocal cords can weaken and shrink, particularly in older adults. This condition, known as vocal cord atrophy, can lead to a hoarse, weak voice. Thyroplasty can help restore vocal cord function in such cases. -
Neurological Disorders:
Certain neurological conditions, such as Parkinson’s disease or multiple sclerosis, can affect the movement and function of the vocal cords, leading to voice problems. -
Trauma or Injury:
Trauma to the larynx or neck, such as from an accident, fall, or surgery, can cause damage to the vocal cords or the nerves controlling them. This damage can lead to permanent voice changes, necessitating thyroplasty. -
Aging:
As people age, the structure of the vocal cords may change, and the muscle tone may decrease. This age-related change can contribute to hoarseness and weakened voice quality. -
Thyroid Surgery or Other Neck Surgery:
Surgeries performed in the neck area, such as thyroidectomy or parathyroid surgery, can inadvertently damage the recurrent laryngeal nerve (RLN), which controls the vocal cords. Damage to this nerve can cause vocal cord paralysis and may require thyroplasty to restore voice function.
Risk Factors for Needing Thyroplasty
While any individual can develop vocal cord dysfunction, several risk factors increase the likelihood of requiring thyroplasty:
-
Prior Neck or Thyroid Surgery:
People who have undergone thyroid or other neck surgeries are at higher risk of vocal cord damage due to the close proximity of the recurrent laryngeal nerve. -
Trauma or Injury:
Physical trauma, such as neck injuries or accidental choking, can lead to vocal cord paralysis or scarring, requiring surgical treatment. -
Voice Overuse or Misuse:
Excessive or improper use of the voice (like constant shouting, singing, or speaking for extended periods) can lead to vocal cord strain or injury, contributing to long-term voice problems. -
Medical Conditions:
Neurological conditions such as stroke, Bell’s palsy, or brain tumors can affect the nerves controlling the vocal cords, increasing the likelihood of requiring thyroplasty.
Common Symptoms Indicating the Need for Thyroplasty
Patients with vocal cord dysfunction may experience a variety of symptoms, which can range from mild hoarseness to complete loss of voice. Symptoms that may indicate the need for thyroplasty include:
-
Hoarseness or a Weak Voice:
Hoarseness, a breathy or raspy voice, or a weak voice that doesn't project well can be indicative of vocal cord problems. These issues may worsen over time or after prolonged speaking. -
Difficulty Speaking or Breathing:
If the vocal cords do not come together properly, it can affect both speech and breathing. Patients may experience difficulty speaking for extended periods or shortness of breath. -
Chronic Throat Clearing or Coughing:
A sensation of something being stuck in the throat, constant throat clearing, or frequent coughing can be signs of vocal cord paralysis or scarring, which may require surgical intervention. -
Voice Fatigue:
Voice fatigue, where the voice becomes tired or strained after speaking for a short period, can be a sign of vocal cord dysfunction. This condition may lead to the need for thyroplasty to restore normal voice function. -
Loss of High-Pitched Sounds:
Difficulty producing high-pitched sounds or a change in vocal pitch can indicate a problem with the vocal cords' ability to vibrate and create sound. This may be related to vocal cord atrophy or paralysis. -
Gasping for Air or Choking:
Difficulty breathing, gasping, or choking while speaking or eating can occur when the vocal cords are unable to function properly, resulting in airway obstruction.
To determine whether thyroplasty is necessary, a comprehensive diagnostic evaluation is performed by an ENT specialist (otolaryngologist). The diagnostic process typically includes:
Clinical Evaluation
-
Medical History and Symptom Review:
The doctor will ask about the patient’s symptoms, previous surgeries (especially in the neck or throat), any trauma to the vocal cords, and whether the symptoms have been persistent or progressive. -
Physical Examination:
A thorough physical examination of the throat, neck, and voice quality will be conducted to check for visible signs of vocal cord dysfunction, inflammation, or paralysis.
Diagnostic Tests
-
Laryngoscopy:
A laryngoscopy involves using a flexible scope with a camera to examine the larynx (voice box) and vocal cords. This test allows the doctor to assess the movement, structure, and function of the vocal cords and identify any abnormalities. -
Stroboscopy:
Stroboscopy is a specialized type of laryngoscopy that uses a strobe light to observe the vibrations of the vocal cords in slow motion. This provides a detailed view of vocal cord movement and helps diagnose conditions like vocal cord paralysis, lesions, or atrophy. -
Voice Assessment:
A speech-language pathologist may conduct a voice assessment to evaluate the patient's voice quality, pitch, and loudness, and determine how well the vocal cords are functioning. -
Electromyography (EMG):
An EMG test may be performed to assess the nerve function of the vocal cords. It helps determine whether nerve damage is the cause of vocal cord paralysis or dysfunction.
Surgical Treatment: Thyroplasty
The primary treatment for restoring vocal cord function in patients with vocal cord paralysis, atrophy, or other voice disorders is thyroplasty. There are several types of thyroplasty, depending on the cause of the problem:
-
Medialization Thyroplasty (Type I):
This procedure is performed to reposition the paralyzed vocal cord to the midline, where it can come into contact with the other vocal cord. A small implant is placed to push the vocal cord toward the center, improving voice production and airway protection. -
Arytenoid Adduction (Type II):
In some cases, the arytenoid cartilage (which controls vocal cord movement) is repositioned to improve the voice. This procedure is often done in conjunction with medialization thyroplasty for patients with more severe vocal cord dysfunction. -
Thyroid Cartilage Shifting (Type III):
This procedure involves repositioning the thyroid cartilage (the main cartilage of the larynx) to improve the tension of the vocal cords, typically used for cases of vocal cord atrophy. -
Injection Laryngoplasty:
This less invasive procedure involves injecting a filler material (such as collagen or hyaluronic acid) into the vocal cord to bulk it up and improve contact with the opposite vocal cord. It is often used in cases of vocal cord paralysis or weakness. -
Reconstruction or Repair of Vocal Cord Lesions:
If a vocal cord lesion, such as a polyp or cyst, is present, surgery may be needed to remove or repair the lesion and restore normal vocal cord function.
Non-Surgical Treatments
In some cases, surgery may not be necessary, and patients can benefit from other treatments, such as:
-
Speech Therapy:
Speech therapy can help patients with weak or impaired voices learn techniques to improve vocal cord function, strength, and endurance. This is particularly helpful in cases of mild vocal cord dysfunction or post-surgical recovery. -
Voice Rest and Hydration:
For patients with temporary vocal cord issues, voice rest (avoiding excessive speaking or shouting) and proper hydration may help restore function.
Preventing Voice Disorders
While some causes of vocal cord issues are genetic or unavoidable, several steps can be taken to reduce the risk of needing thyroplasty:
-
Avoid Excessive Straining or Misuse of the Voice:
Avoid shouting, speaking loudly for extended periods, or using poor voice technique that can strain the vocal cords. -
Stay Hydrated:
Keeping the vocal cords hydrated by drinking plenty of fluids helps prevent dryness, which can lead to irritation or injury. -
Quit Smoking:
Smoking is a major risk factor for vocal cord damage and other throat issues. Quitting smoking can improve vocal cord health and reduce the risk of related problems. -
Manage Underlying Health Conditions:
Conditions like GERD, allergies, and nasal congestion can irritate the vocal cords, so managing these conditions appropriately can prevent long-term damage.
Although thyroplasty is generally a safe procedure, there are some potential risks and complications:
-
Infection:
As with any surgery, infection is a potential complication. Antibiotics are often prescribed after surgery to reduce the risk. -
Bleeding:
Minor bleeding can occur, but excessive bleeding is rare. -
Vocal Cord Damage:
In rare cases, further damage to the vocal cords may occur during surgery, affecting voice quality. -
Change in Voice Quality:
While the goal of thyroplasty is to improve the voice, some patients
may experience temporary or permanent changes in voice pitch or quality.
-
Need for Revision Surgery:
Some patients may require additional surgery if the initial procedure does not provide the desired results or if the implants or adjustments move over time.
After undergoing thyroplasty, many patients experience significant improvement in their voice. However, there are several things to consider post-surgery:
Post-Surgery Care
-
Voice Rest:
Patients are typically advised to rest their voices for a few days to allow the vocal cords to heal. -
Follow-Up Appointments:
Regular follow-up visits with the ENT specialist are crucial to monitor healing and the effectiveness of the surgery. -
Speech Therapy:
Speech therapy may be recommended to optimize vocal cord function and improve overall voice quality after surgery. -
Healthy Habits:
Maintaining hydration, avoiding smoking, and practicing good vocal hygiene will help preserve the benefits of thyroplasty.
1. What is thyroplasty?
Thyroplasty is a surgical procedure used to treat voice and breathing disorders caused by dysfunction of the vocal cords. It involves modifying the thyroid cartilage, which surrounds the vocal cords, to improve voice quality, pitch, and breathing function.
2. Why is thyroplasty performed?
Thyroplasty is commonly performed to treat hoarseness, voice changes, or difficulty breathing caused by vocal cord paralysis, scarring, or other structural issues affecting the vocal cords. It can also be used to treat conditions like laryngeal cancer or vocal cord atrophy.
3. How is thyroplasty performed?
The procedure is typically done under general anesthesia. The surgeon makes a small incision in the neck to access the thyroid cartilage. Various types of implants or sutures are then used to reposition the vocal cords or strengthen the cartilage to improve vocal cord function.
4. Is thyroplasty painful?
The surgery is performed under anesthesia, so there is no pain during the procedure. Afterward, patients may experience mild discomfort, soreness in the neck, and difficulty swallowing for a few days to a week. Pain is generally manageable with medications.
5. How long does thyroplasty take?
Thyroplasty typically takes about 1 to 2 hours to complete, depending on the complexity of the case and the specific procedure being used. It is usually performed on an outpatient basis, meaning patients can go home the same day.
6. What is the recovery time after thyroplasty?
Recovery time varies, but most patients can return to normal activities within 1 to 2 weeks. Voice rest is recommended for the first few days following surgery, and patients may need to avoid strenuous activities or heavy lifting for several weeks.
7. Are there risks or complications associated with thyroplasty?
Risks include infection, bleeding, damage to surrounding structures (such as nerves), scarring, and changes in voice quality. In rare cases, the implant may need to be adjusted or replaced. These risks are minimized when the procedure is performed by an experienced surgeon.
8. How should I prepare for thyroplasty?
Preparation includes a thorough medical evaluation, including a laryngoscopy to examine the vocal cords, imaging tests to assess the airway, and an assessment of general health. You may need to stop taking certain medications, like blood thinners, prior to surgery. It is also important to arrange for someone to drive you home after surgery.
9. What are the expected results after thyroplasty?
Most patients experience significant improvement in voice quality, including reduced hoarseness and improved speech clarity. Breathing difficulties caused by vocal cord paralysis or dysfunction are often alleviated. Results are typically long-lasting, but follow-up visits are needed to monitor recovery and ensure the best outcome.
10. Can thyroplasty be repeated if necessary?
Yes, in cases where the initial procedure does not provide optimal results, or if complications occur, thyroplasty can be repeated. Some patients may require additional adjustments or enhancements to the implant over time.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


