Uvulopalate Pharyngoscopy (UPP) is a diagnostic procedure primarily used to examine the structures of the uvula, soft palate, and pharynx to assess any abnormalities that may contribute to airway obstruction, chronic snoring, obstructive sleep apnea (OSA), swallowing difficulties, and speech impairments. This minimally invasive procedure involves the use of a flexible endoscope or camera that is inserted through the nose or mouth to get a detailed view of the throat.
Uvulopalate Pharyngoscopy serves both diagnostic and therapeutic purposes. It is often performed when there is a concern that the uvula, soft palate, or other structures in the throat may be contributing to snoring or sleep apnea. By visualizing the soft tissues in the back of the throat, healthcare providers can identify the precise cause of the obstruction or dysfunction, enabling them to recommend effective treatments.
Though Uvulopalate Pharyngoscopy is often associated with evaluating sleep-disordered breathing, it is also used to assess other conditions such as chronic tonsillitis, pharyngeal obstruction, and even certain cancers of the throat. The procedure is valuable in sleep medicine and ENT (Ear, Nose, and Throat) specialties due to its ability to directly visualize anatomical and physiological issues in the upper airway.
Uvulopalate Pharyngoscopy is most commonly employed to evaluate conditions that cause airway obstruction, particularly those related to the uvula, soft palate, and pharyngeal tissues. Understanding the causes and risk factors that lead to the need for this procedure is crucial for both diagnosis and treatment. Let’s explore these causes in greater detail.
Common Causes of Airway Obstruction and Dysfunction:
-
Obstructive Sleep Apnea (OSA):
-
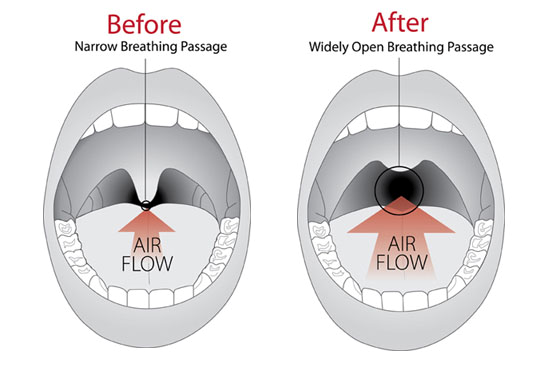
One of the primary reasons for performing Uvulopalate Pharyngoscopy is to assess Obstructive Sleep Apnea (OSA), a condition where there is intermittent blockage of the upper airway during sleep. This blockage often occurs when the soft tissues of the throat, including the uvula and soft palate, collapse and obstruct the airway, leading to difficulty breathing. This obstruction results in disrupted sleep, gasping, and choking episodes, along with excessive daytime sleepiness.
-
OSA is a severe condition associated with cardiovascular diseases, high blood pressure, stroke, and even diabetes. Identifying the exact anatomical cause of OSA via Uvulopalate Pharyngoscopy helps in developing targeted treatments like surgery, CPAP therapy, or oral appliances.
-
-
Chronic Snoring:
-
Chronic snoring, while often dismissed as a nuisance, is frequently linked to partial obstruction of the airway during sleep. This obstruction occurs when the uvula or soft palate vibrates excessively due to airflow resistance. Snoring is not only disruptive but can also be a sign of an underlying condition like sleep apnea.
-
Uvulopalate Pharyngoscopy is instrumental in determining the specific tissues (e.g., the uvula, soft palate, or pharynx) that are vibrating or obstructing airflow, which allows for the development of an effective treatment plan to reduce or eliminate snoring.
-
-
Enlarged Tonsils and Adenoids:
-
Enlarged tonsils and adenoids are common contributors to airway obstruction, particularly in children. These tissues, when inflamed or enlarged, can obstruct the upper airway, leading to mouth breathing, snoring, sleep apnea, and difficulty swallowing. The tonsils and adenoids are located in the pharynx, making them critical areas of concern when assessing airway obstructions.
-
Uvulopalate Pharyngoscopy can help visualize the size and positioning of the tonsils and adenoids, helping doctors determine whether they need to be removed surgically to alleviate symptoms.
-
-
Uvular Prolapse and Elongation:
-
Uvular prolapse (where the uvula becomes elongated or swollen) or uvular elongation can contribute to obstructive sleep apnea and snoring. An elongated or enlarged uvula can obstruct airflow during sleep and increase tissue vibration, leading to snoring. It may also irritate the throat and contribute to sleep disruption.
-
Uvulopalate Pharyngoscopy provides clear visualization of the uvula, helping to determine if it is elongated or prolapsed, which may require surgical intervention to restore normal airway function.
-
-
Pharyngeal Obstruction (Tumors, Cysts, and Abnormal Growths):
-
Abnormal growths or tumors in the pharynx can obstruct the airway, leading to symptoms such as snoring, difficulty swallowing, or changes in speech. These growths can be benign (non-cancerous) or malignant (cancerous).
-
Uvulopalate Pharyngoscopy can be used to assess the size, location, and nature of any abnormal masses in the throat. If necessary, the procedure can assist in guiding biopsy or removal of these growths.
-
-
Chronic Infections and Inflammation (Tonsillitis, Pharyngitis):
-
Chronic tonsillitis (inflammation of the tonsils) and pharyngitis (inflammation of the pharynx) can lead to swollen tissues that obstruct the airway and contribute to symptoms like sore throat, swallowing difficulties, and breathing issues.
-
Recurrent or chronic infections may require surgical intervention (such as tonsillectomy or adenoidectomy) if conservative treatments (e.g., antibiotics) do not alleviate the problem. Uvulopalate Pharyngoscopy can help assess the extent of infection and whether surgical removal is necessary.
-
Risk Factors for Airway Obstruction:
-
Obesity and Overweight:
-
Excess weight, particularly around the neck and throat, can contribute to airway collapse during sleep. Obesity is a significant risk factor for sleep apnea and snoring as excess tissue around the neck can press on the airway and cause obstruction. Reducing weight through lifestyle changes can improve these conditions and minimize the need for more invasive treatments.
-
-
Age and Gender:
-
As people age, the muscles and tissues in the throat weaken, increasing the likelihood of airway obstruction during sleep. Sleep apnea and snoring are more common in older adults due to these changes. Men are more likely to suffer from sleep apnea, though post-menopausal women are also at increased risk.
-
-
Genetic Factors:
-
Some individuals may be genetically predisposed to airway obstruction due to anatomical features such as a small jaw, enlarged tonsils, or a narrow airway. These structural traits can increase the risk of snoring, OSA, and difficulty swallowing.
-
-
Smoking and Alcohol Use:
-
Smoking causes inflammation in the upper respiratory tract, which can narrow the airway and increase the risk of snoring and sleep apnea. Additionally, alcohol relaxes the muscles in the throat, exacerbating airway obstruction during sleep.
-
-
Chronic Allergies and Nasal Congestion:
-
Individuals with chronic nasal congestion due to allergies, sinusitis, or a deviated septum are more likely to breathe through their mouths during sleep. Mouth breathing can exacerbate airway obstruction and increase the risk of snoring or sleep apnea.
-
The symptoms of airway obstruction and related conditions often prompt individuals to seek evaluation through Uvulopalate Pharyngoscopy. Understanding these symptoms is essential in identifying when this procedure may be needed.
Key Symptoms Indicating the Need for Uvulopalate Pharyngoscopy:
-
Loud and Chronic Snoring:
-
Persistent and loud snoring is often a sign that the airway is partially obstructed. The uvula and soft palate are common culprits of airway obstruction. When snoring is accompanied by other symptoms like choking or gasping, it may indicate sleep apnea.
-
-
Daytime Sleepiness and Fatigue:
-
Individuals with untreated sleep apnea often experience excessive daytime sleepiness, irritability, and poor concentration. This is due to fragmented sleep caused by repeated pauses in breathing throughout the night.
-
-
Breathing Pauses During Sleep:
-
One of the hallmarks of obstructive sleep apnea is frequent breathing pauses during sleep. This occurs when the airway is temporarily blocked, causing individuals to wake up abruptly, gasping for air. This can significantly disrupt sleep and result in a lack of restful sleep.
-
-
Choking or Gasping for Air During Sleep:
-
People with severe sleep apnea may wake up multiple times during the night due to choking or gasping for air. This is a direct result of the airway obstruction caused by the uvula, soft palate, or other structures in the throat.
-
-
Difficulty Swallowing (Dysphagia):
-
Difficulty swallowing food, liquids, or even saliva can be a symptom of a structural issue in the throat, such as enlarged tonsils, a prolapsed uvula, or a narrowed pharynx. Uvulopalate Pharyngoscopy can help identify the cause of dysphagia.
-
-
Dry Mouth and Throat Clearing:
-
Chronic mouth breathing during sleep often leads to dry mouth and throat irritation, which can also be a sign of obstructed airflow. This can contribute to discomfort upon waking, as well as frequent throat clearing.
-
-
Speech Problems:
-
Uvular and palatal abnormalities can affect speech patterns. Individuals may experience nasal voice or other speech impairments, particularly if there is a blockage or abnormality affecting the palate or uvula.
-
-
Chronic Sore Throat or Throat Irritation:
-
People with chronic airway obstruction may suffer from a persistent sore throat, especially upon waking. This is often caused by mouth breathing and the irritation of tissues in the throat.
-
The diagnosis of airway obstruction and other related conditions typically involves a combination of a medical history review, physical examination, and diagnostic procedures such as Uvulopalate Pharyngoscopy.
Steps in Diagnosing the Condition:
-
Medical History and Symptom Review:
-
The doctor will start by reviewing the patient’s medical history, including symptoms such as snoring, daytime fatigue, gasping for breath during sleep, difficulty swallowing, or frequent throat clearing.
-
-
Physical Examination:
-
A thorough examination of the throat, mouth, and neck is conducted. The doctor will assess the size and positioning of the tonsils, uvula, and soft palate. They may also examine the nose and sinuses to check for any additional causes of airway obstruction.
-
-
Polysomnography (Sleep Study):
-
Polysomnography is a diagnostic test used to evaluate sleep-related breathing disorders. During this study, a patient’s sleep patterns, brain activity, heart rate, breathing patterns, and oxygen levels are monitored. It helps confirm the diagnosis of sleep apnea and assess its severity.
-
-
Flexible Endoscopy and Laryngoscopy:
-
Flexible endoscopy or laryngoscopy is used to examine the upper airway. A flexible tube with a camera and light is inserted through the nose or mouth, providing a real-time view of the uvula, soft palate, and pharyngeal structures. This allows for the detection of abnormalities, inflammation, or blockages that may be contributing to symptoms.
-
-
Imaging Studies:
-
In some cases, CT scans or MRI scans may be used to further evaluate the airway structures, particularly when tumors, cysts, or other growths are suspected.
-
After diagnosing the cause of airway obstruction or other related conditions through Uvulopalate Pharyngoscopy, the appropriate treatment plan is developed. Treatment options vary depending on the severity and cause of the obstruction.
Non-Surgical Treatment Options:
-
Continuous Positive Airway Pressure (CPAP):
-
CPAP therapy is the gold standard treatment for Obstructive Sleep Apnea (OSA). The CPAP machine delivers a constant flow of air through a mask to keep the airway open while the patient sleeps.
-
-
Lifestyle Modifications:
-
Weight loss: Reducing excess weight can alleviate symptoms of sleep apnea and snoring caused by fat deposits around the neck.
-
Sleep position changes: Sleeping on the side instead of the back may help prevent airway collapse.
-
Avoiding alcohol and sedatives: These substances relax the throat muscles and can exacerbate sleep apnea.
-
-
Oral Appliances:
-
Dental mandibular advancement devices are used to reposition the lower jaw and tongue, which helps keep the airway open during sleep. These devices are commonly used for mild to moderate sleep apnea.
-
-
Medications:
-
Steroids, antihistamines, or decongestants may be prescribed to reduce inflammation and swelling in the throat, particularly if the obstruction is caused by chronic infection or allergies.
-
Surgical Treatment Options:
-
Uvulopalatopharyngoplasty (UPPP):
-
This surgical procedure removes excess tissue from the uvula, soft palate, and sometimes the pharynx to widen the airway and improve airflow during sleep.
-
-
Tonsillectomy and Adenoidectomy:
-
Removal of the tonsils or adenoids is often necessary for individuals with enlarged tonsils or adenoids that obstruct the airway. This procedure is particularly effective in children with sleep apnea or chronic infections.
-
-
Genioglossus Advancement (GA):
-
This surgery repositions the tongue muscle to prevent airway collapse during sleep, often in combination with UPPP for more effective results.
-
-
Radiofrequency Ablation:
-
This procedure uses controlled heat to shrink excess tissue in the uvula, soft palate, and other parts of the throat to reduce obstruction.
-
While not all causes of airway obstruction can be prevented, several strategies can help reduce the risk of developing sleep apnea, snoring, and other related conditions:
Preventive Strategies:
-
Maintain a Healthy Weight:
-
Losing weight can significantly reduce the likelihood of airway obstruction caused by excess tissue around the neck.
-
-
Avoid Smoking and Excessive Alcohol Use:
-
Smoking and alcohol use both relax the muscles in the throat, making airway collapse more likely.
-
-
Practice Good Sleep Hygiene:
-
Establishing a regular sleep schedule, avoiding late-night meals, and sleeping on your side can help prevent or reduce snoring and sleep apnea.
-
-
Regular Medical Check-ups:
-
For individuals with a history of snoring, sleep apnea, or airway issues, regular follow-up visits with a healthcare provider are essential to manage symptoms and prevent complications.
-
Though Uvulopalate Pharyngoscopy is generally a safe procedure, there are risks and potential complications associated with both the diagnostic process and any subsequent treatments:
-
Infection:
-
Infections can occur following any surgical or diagnostic procedure involving the throat.
-
-
Bleeding:
-
Bleeding may occur, particularly when tissue samples are taken or if surgery is performed to remove enlarged tissues.
-
-
Swelling and Pain:
-
Some swelling and discomfort in the throat are common after the procedure, especially if surgical interventions were performed.
-
-
Voice Changes:
-
Some patients may experience temporary voice changes following surgery, particularly if the soft palate or uvula is altered.
-
Post-treatment care and ongoing management are key to ensuring successful recovery and symptom relief. Here’s how to live with and manage conditions assessed by Uvulopalate Pharyngoscopy:
Post-Treatment Care:
-
Follow-up Appointments:
-
Regular visits with an ENT specialist are important to monitor progress and check for complications, especially if surgical intervention was performed.
-
-
Lifestyle Adjustments:
-
Committing to healthy habits such as weight loss, avoiding alcohol, and adhering to CPAP therapy (if prescribed) can drastically improve the quality of life for those with sleep apnea or snoring issues.
-
-
Speech and Swallowing Therapy:
-
In some cases, individuals may benefit from speech or swallowing therapy to address any lingering issues with articulation, swallowing, or voice quality after surgery or treatment.
-
-
Ongoing Monitoring:
-
For individuals with chronic conditions like sleep apnea, ongoing monitoring through home sleep studies or follow-up polysomnography may be necessary to ensure that the condition remains managed.
-
1. What is uvulopalate pharyngoscopy?
Uvulopalate pharyngoscopy is a diagnostic procedure used to examine the throat, soft palate, and uvula (the small hanging structure at the back of the throat). It is often performed to evaluate issues such as snoring, sleep apnea, and problems with swallowing or voice production.
2. Why is uvulopalate pharyngoscopy performed?
This procedure is performed to assess the function and structure of the uvula, soft palate, and pharynx. It is commonly used to diagnose conditions like obstructive sleep apnea, chronic snoring, or issues related to voice production and swallowing difficulties.
3. How is uvulopalate pharyngoscopy performed?
The procedure involves the insertion of a flexible endoscope (a small camera) through the nose or mouth to visualize the uvula, soft palate, and surrounding structures. It allows the doctor to observe airway obstructions or abnormalities in the throat. It is usually done in an office setting and does not require general anesthesia.
4. Is uvulopalate pharyngoscopy painful?
The procedure is generally well-tolerated. Local anesthesia or a numbing spray may be applied to the throat or nasal passages to minimize discomfort. Some patients may feel mild irritation or a sensation of gagging during the procedure, but it is typically not painful.
5. How long does the uvulopalate pharyngoscopy procedure take?
The procedure typically takes about 15 to 30 minutes, depending on the complexity of the examination and the findings.
6. Are there any risks or complications associated with uvulopalate pharyngoscopy?
The procedure is generally safe with minimal risks. Potential complications include mild throat irritation, gagging, or slight discomfort. Rarely, there could be injury to the mucosal lining or discomfort during the procedure. These risks are generally minimized with experienced practitioners.
7. How should I prepare for uvulopalate pharyngoscopy?
Preparation usually involves fasting for several hours before the procedure, especially if sedation is used. It’s important to inform your doctor about any medical conditions, allergies, or medications you’re taking, as these may affect the procedure or results.
8. What can uvulopalate pharyngoscopy diagnose?
This procedure can help diagnose conditions such as:
-
Obstructive sleep apnea (OSA)
-
Chronic snoring
-
Tonsillar or adenoidal enlargement
-
Problems with the soft palate or uvula that may be affecting speech or swallowing
-
Laryngeal abnormalities
9. What should I expect after the procedure?
After the procedure, you may experience mild throat irritation or discomfort, which typically resolves within a few hours. You may be advised to avoid consuming hot or spicy foods and to rest your voice for a short period of time. There are usually no restrictions on activities unless other treatments are needed.
10. Can uvulopalate pharyngoscopy be used for treatment purposes?
While uvulopalate pharyngoscopy is primarily a diagnostic procedure, it may also guide treatment decisions, such as surgical options for snoring or sleep apnea, including uvulopalatopharyngoplasty (UPPP) or other corrective surgeries. In some cases, therapeutic interventions may be planned based on the findings from the pharyngoscopy.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


