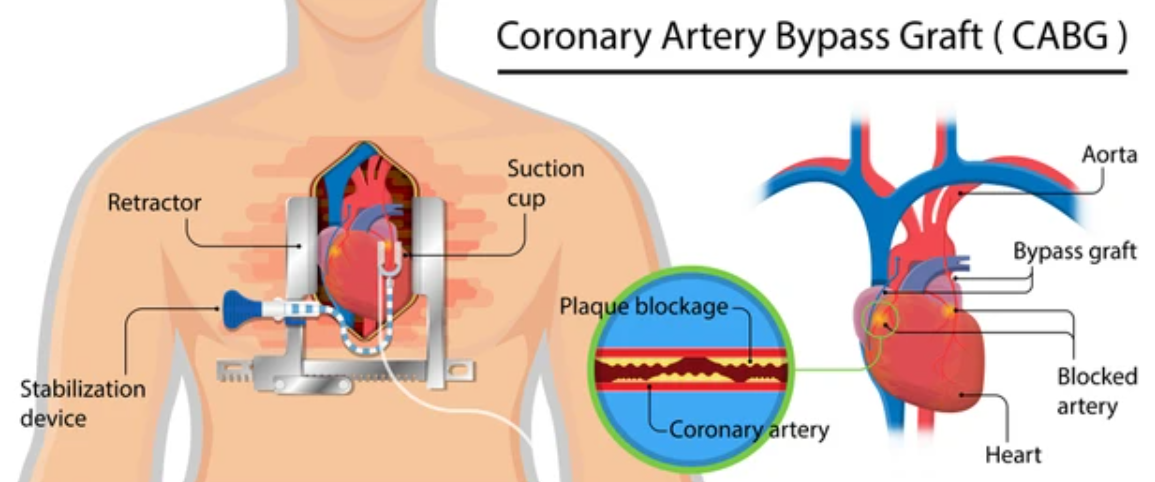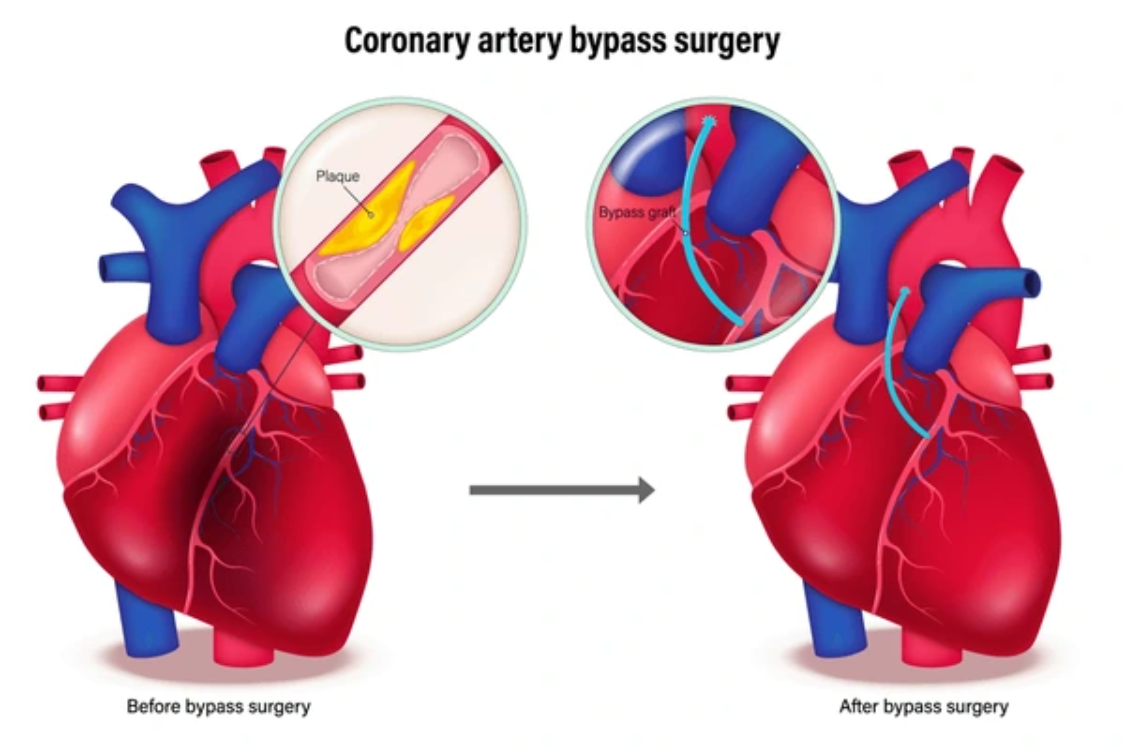
Coronary Artery Bypass Graft (CABG) is a surgical procedure aimed at improving blood flow to the heart in individuals with coronary artery disease (CAD). CAD occurs when the coronary arteries, which supply oxygen-rich blood to the heart, become narrowed or blocked due to atherosclerosis (buildup of plaque and fatty deposits).
During CABG surgery, the surgeon creates new routes, called bypasses, around the blocked or narrowed arteries using healthy blood vessels from other parts of the body, such as the saphenous vein in the leg, the internal mammary artery, or the radial artery in the arm. These new blood vessels allow blood to flow freely to the heart muscle, reducing symptoms like chest pain and improving heart function.
Why is CABG Surgery Necessary?
CABG surgery is typically recommended when:
-
Angina (chest pain) becomes severe and uncontrollable.
-
The heart's ability to pump blood is compromised due to blocked arteries.
-
Non-surgical treatments, like medication and angioplasty, have been ineffective or unsuitable.
CABG surgery can significantly improve quality of life, prevent heart attacks, and prolong survival in patients with severe coronary artery disease.
Understanding the underlying causes and risk factors of coronary artery disease (CAD) is essential for preventing the need for CABG surgery. The primary cause of CAD is the buildup of plaque inside the arteries, which narrows the blood vessels and restricts blood flow to the heart.
Causes of Coronary Artery Disease (CAD)
-
Atherosclerosis:
-
Atherosclerosis is the main cause of CAD. It occurs when plaque—composed of fat, cholesterol, calcium, and other substances—builds up in the coronary arteries. Over time, this plaque hardens and narrows the arteries, leading to decreased blood flow to the heart muscle. This process is often referred to as arterial plaque buildup or clogging.
-
-
Blood Clots:
-
A rupture in an existing plaque in the arteries can lead to the formation of blood clots, which can block the flow of blood to the heart, potentially leading to a heart attack.
-
-
Spasm of the Coronary Arteries:
-
Coronary artery spasm occurs when the coronary arteries temporarily constrict or tighten, reducing blood flow. This can happen due to factors like drug use (e.g., cocaine) or stress, and can lead to severe chest pain or heart attacks.
-
Risk Factors for Coronary Artery Disease (CAD)
Several factors increase the risk of developing CAD, leading to the need for CABG surgery:
-
Age:
-
The risk of coronary artery disease increases with age, especially after the age of 45 for men and 55 for women.
-
-
Family History:
-
A family history of heart disease significantly increases the risk of CAD. If a close family member had a heart attack or heart disease at a young age, the likelihood of developing CAD is higher.
-
-
Smoking:
-
Smoking contributes to arterial plaque buildup and can cause the narrowing of arteries, raising the risk of CAD and subsequent heart attacks.
-
-
High Blood Pressure:
-
Hypertension or high blood pressure puts added stress on the heart and arteries, contributing to plaque buildup and increasing the risk of heart disease.
-
-
High Cholesterol:
-
Elevated levels of LDL cholesterol ("bad" cholesterol) and low levels of HDL cholesterol ("good" cholesterol) contribute to the development of atherosclerosis, raising the risk of coronary artery disease.
-
-
Diabetes:
-
People with diabetes or insulin resistance have a higher risk of developing coronary artery disease due to the effects of high blood sugar on the arteries and blood vessels.
-
-
Obesity:
-
Being overweight or obese increases the risk of developing CAD through its association with high blood pressure, high cholesterol, and diabetes.
-
-
Physical Inactivity:
-
Lack of regular physical activity is a significant risk factor for the development of CAD. Exercise helps control weight, lower blood pressure, and improve cholesterol levels.
-
-
Stress:
-
Chronic stress, particularly when combined with unhealthy lifestyle choices, can contribute to heart disease by increasing blood pressure, promoting inflammation, and accelerating plaque buildup.
-
-
Unhealthy Diet:
-
A diet high in saturated fats, trans fats, sodium, and refined sugars contributes to the development of plaque buildup in the arteries.
-
The symptoms of coronary artery disease can vary from person to person, and in some cases, there may be no symptoms until the condition becomes severe. The presence of symptoms often signals that there is a significant narrowing or blockage of the coronary arteries.
Common Symptoms of Coronary Artery Disease
-
Angina (Chest Pain):
-
Angina is the most common symptom of CAD and occurs when the heart muscle does not get enough oxygenated blood. This results in chest pain or discomfort that may feel like pressure, tightness, squeezing, or heaviness in the chest. The pain may radiate to the left arm, neck, jaw, or back.
-
-
Shortness of Breath:
-
Shortness of breath is common, especially during physical activity, as the heart struggles to pump enough oxygen-rich blood to the body. It can be a sign that the heart is not getting enough blood flow due to narrowed arteries.
-
-
Fatigue:
-
Fatigue and a general feeling of weakness can be an early symptom of CAD, especially if the heart is unable to pump blood effectively due to clogged arteries.
-
-
Heart Palpitations:
-
Irregular heartbeats or heart palpitations can occur due to the decreased blood flow to the heart, which may be an early sign of CAD.
-
-
Dizziness or Lightheadedness:
-
Decreased blood flow to the heart can result in dizziness, fainting, or lightheadedness, particularly during physical activity or stress.
-
-
Sweating:
-
Unexplained excessive sweating, particularly during physical exertion or even at rest, may be a sign of CAD or an impending heart attack.
-
A thorough diagnosis of coronary artery disease (CAD) is necessary to determine if CABG surgery is required. Several tests are used to assess the extent of blockages in the coronary arteries and the heart’s overall function.
Diagnostic Steps for CAD
-
Physical Examination:
-
The doctor will perform a physical exam, checking for signs of heart disease such as high blood pressure, abnormal heart sounds, or signs of heart failure.
-
-
Electrocardiogram (ECG/EKG):
-
An ECG measures the electrical activity of the heart and can identify abnormalities in heart rhythm or evidence of previous heart attacks.
-
-
Stress Testing:
-
A stress test involves exercising on a treadmill while being monitored for changes in heart function. This test assesses how well the heart performs under physical stress and helps detect blockages in the coronary arteries.
-
-
Echocardiogram:
-
An echocardiogram uses sound waves to create images of the heart’s chambers and valves. This test can help evaluate heart function and blood flow.
-
-
Coronary Angiography:
-
Coronary angiography is the gold standard for diagnosing CAD. A catheter is inserted into the coronary arteries, and dye is injected to visualize any blockages or narrowing of the arteries on an X-ray screen.
-
-
CT Angiography:
-
CT angiography is a non-invasive test that uses CT scans to create detailed images of the coronary arteries. It is particularly helpful in detecting coronary artery blockages.
-
-
Blood Tests:
-
Blood tests may be done to check for risk factors such as high cholesterol, high blood sugar, and kidney function, which contribute to the development of CAD.
-
The treatment for coronary artery disease depends on the severity of the condition, the extent of the blockages, and the individual patient’s health. Non-surgical options are often tried first, but CABG surgery is recommended when the blockages are severe or the patient has not responded to other treatments.
Non-Surgical Treatment Options
-
Medications:
-
Aspirin or antiplatelet drugs are prescribed to reduce the risk of blood clots.
-
Statins help lower cholesterol levels, reducing plaque buildup.
-
Beta-blockers and ACE inhibitors help lower blood pressure and reduce the heart’s workload.
-
-
Angioplasty and Stenting:
-
Angioplasty involves using a balloon to open narrowed or blocked arteries. A stent (a small mesh tube) may be placed to keep the artery open.
-
-
Lifestyle Modifications:
-
A heart-healthy diet, regular exercise, weight management, and quitting smoking are essential components of managing CAD.
-
Surgical Treatment: CABG Surgery
CABG surgery is performed when other treatments are ineffective or the blockages are too severe. The surgeon will take a healthy blood vessel from another part of the body (often the leg, chest, or arm) and attach it to the coronary artery, bypassing the blockage and improving blood flow to the heart.
Preventing coronary artery disease (and the need for CABG surgery) involves making significant lifestyle changes and managing risk factors effectively.
Preventive Measures for CAD
-
Heart-Healthy Diet:
-
Consume a balanced diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats. Limit saturated fats, trans fats, and sodium.
-
-
Regular Exercise:
-
Engage in moderate to vigorous exercise for at least 150 minutes per week to improve heart health and reduce cholesterol levels.
-
-
Control Blood Pressure:
-
Maintain healthy blood pressure through lifestyle changes and medications, if necessary.
-
-
Manage Cholesterol:
-
Keep cholesterol levels in check by eating heart-healthy foods, exercising, and taking medications if prescribed.
-
-
Quit Smoking:
-
Smoking accelerates the development of coronary artery disease and increases the risk of heart attacks. Quitting smoking significantly lowers these risks.
-
-
Diabetes Management:
-
If you have diabetes, managing blood sugar levels is crucial to preventing complications like CAD.
-
While CABG surgery is highly effective, there are potential complications that may arise, both during and after the procedure.
Possible Complications of CABG Surgery
-
Infection:
-
As with any surgery, there is a risk of infection at the incision sites or in the heart after surgery.
-
-
Bleeding:
-
Patients undergoing CABG surgery may experience bleeding, particularly during or after the surgery, which may require additional interventions.
-
-
Heart Attack:
-
In rare cases, a heart attack may occur during the surgery due to complications with the heart’s blood flow.
-
-
Stroke:
-
There is a small risk of a stroke during CABG surgery due to blood clots traveling to the brain.
-
-
Arrhythmias:
-
After surgery, patients may develop irregular heart rhythms (arrhythmias), which may require further treatment.
-
-
Memory and Cognitive Issues:
-
Some patients may experience memory problems or cognitive decline after surgery, though this tends to improve over time.
-
After undergoing CABG surgery, it’s important to follow a recovery plan to ensure proper healing and prevent further complications.
Post-Surgery Recovery
-
Hospital Stay:
-
After the surgery, patients typically stay in the hospital for 5-7 days to recover. During this time, the healthcare team will monitor for any complications and help manage pain.
-
-
Cardiac Rehabilitation:
-
Cardiac rehabilitation is a structured program designed to help patients recover and regain strength. It includes supervised exercise, dietary advice, and counseling.
-
-
Gradual Return to Normal Activities:
-
Most patients can return to work within 4-6 weeks, though heavy physical activities should be avoided for 2-3 months to allow full recovery.
-
-
Lifestyle Adjustments:
-
Long-term success after CABG surgery depends on adopting heart-healthy habits, including maintaining a healthy diet, exercising regularly, controlling blood pressure and cholesterol, and avoiding smoking.
-
1. What is Coronary Artery Bypass Graft (CABG) Surgery?
Coronary Artery Bypass Graft (CABG) surgery is a procedure performed to treat coronary artery disease (CAD), a condition in which the arteries supplying blood to the heart become narrowed or blocked. During CABG, a healthy blood vessel is taken from another part of the body (such as the leg, chest, or arm) and used to bypass the blocked or narrowed sections of the coronary arteries, improving blood flow to the heart.
2. Why is CABG surgery needed?
CABG surgery is recommended when the coronary arteries are severely blocked, causing:
-
Chest pain (angina) or shortness of breath, which are symptoms of reduced blood flow to the heart.
-
Heart attacks caused by the blockage of coronary arteries.
-
Failure of other treatments, such as lifestyle changes, medication, or angioplasty (ballooning the artery) or stenting.
3. How is CABG surgery performed?
During CABG surgery, the surgeon will:
-
Make a small incision in the chest to access the heart.
-
Take a healthy blood vessel (usually the saphenous vein from the leg, or the internal mammary artery from the chest) and attach one end to the aorta and the other end to the coronary artery beyond the blocked area.
-
This bypass graft restores proper blood flow to the heart.
-
In some cases, multiple bypasses may be performed if there are multiple blocked arteries.
CABG can be performed as open-heart surgery or with a minimally invasive technique, where smaller incisions are made.
4. Is CABG surgery painful?
CABG surgery is performed under general
anesthesia, so there is no pain during the procedure. After the surgery, patients may
experience discomfort, especially in the chest
area where the incision was made. Some patients also report soreness in the legs if the saphenous vein was used. Pain management
strategies, including medication, are provided to keep discomfort under control. Most pain subsides
after a few weeks.
5. How long does CABG surgery take?
The duration of CABG surgery can vary depending on the number of bypasses required, but it typically takes 3 to 6 hours. If multiple bypasses are needed, the surgery may take longer.
6. What is the recovery time after CABG surgery?
Recovery after CABG surgery generally follows this timeline:
-
Hospital stay: Typically 5 to 7 days for monitoring and recovery.
-
Initial recovery: Patients may feel fatigued or weak for 6 to 8 weeks.
-
Full recovery: It may take 3 to 6 months for the body to heal completely. During this period, patients are encouraged to gradually resume physical activities and follow a cardiac rehabilitation program to restore heart function.
It is important to avoid strenuous activities for at least 6 weeks after surgery to allow the chest to heal.
7. Are there any risks or complications with CABG surgery?
As with any major surgery, CABG carries some risks, including:
-
Infection at the incision sites.
-
Bleeding or blood clots.
-
Stroke or heart attack during or after surgery.
-
Arrhythmias (irregular heart rhythms), which are common but usually temporary.
-
Kidney problems due to decreased blood flow during surgery.
-
Graft failure, where the bypass vessel becomes blocked or narrowed over time.
However, the overall risk of complications is generally low with modern surgical techniques and a skilled surgical team.
8. How should I prepare for CABG surgery?
Preparation for CABG surgery typically involves:
-
Preoperative tests: These may include blood tests, imaging (e.g., angiography), and an electrocardiogram (ECG) to assess heart health.
-
Fasting: You’ll be instructed to fast for 6 to 8 hours before the surgery to prevent complications with anesthesia.
-
Medications: Your doctor may adjust or stop certain medications, especially blood thinners.
-
Arrangements for recovery: You should arrange for someone to help at home during the initial recovery period.
9. Can CABG surgery cure coronary artery disease?
While CABG surgery can significantly improve symptoms and blood flow, it does not cure coronary artery disease. The underlying disease process, such as atherosclerosis (hardening of the arteries), may still progress. However, CABG improves heart function and reduces the risk of heart attacks. Lifestyle changes, including a healthy diet, regular exercise, and medication, are essential to manage the condition and prevent future blockages.
10. Is CABG surgery covered by insurance?
Yes, CABG surgery is typically covered by most health insurance plans when it is deemed medically necessary, such as for patients with severe coronary artery disease or recurrent heart attacks. It’s important to confirm coverage details with your insurance provider before surgery, including hospital stays, follow-up care, and rehabilitation services.