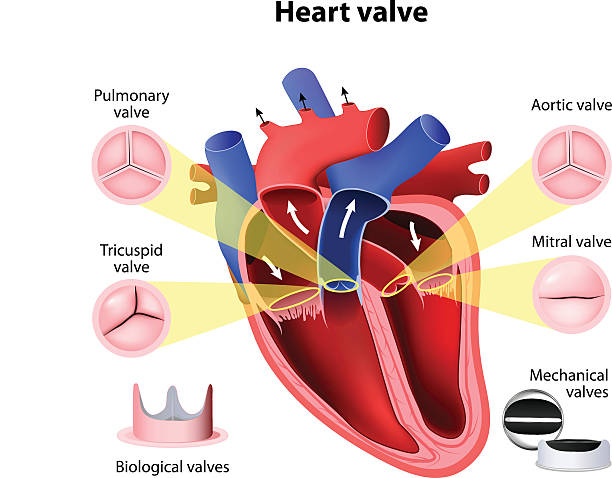
Heart valve replacement is a surgical procedure that replaces a damaged heart valve with a new one. The heart contains four valves – the aortic valve, mitral valve, pulmonary valve, and tricuspid valve – which ensure that blood flows in the correct direction through the heart and to the rest of the body. When one or more of these valves become damaged, they may no longer function properly, causing blood to flow backward, restrict normal blood flow, or lead to other complications.
The most common reasons for valve dysfunction are valvular heart disease (VHD), calcification, congenital valve defects, and conditions like endocarditis or rheumatic fever. If these conditions are severe, heart valve replacement may be necessary to prevent complications such as heart failure, stroke, or other severe symptoms.
Laparoscopic heart valve replacement is a minimally invasive technique that allows surgeons to replace damaged valves using small incisions, guided by a camera. This technique has revolutionized the way valve replacement surgery is performed, reducing recovery time, scarring, and complications, and offering an option for high-risk patients.
This procedure can replace damaged valves with either mechanical valves (made of durable materials) or biological valves (made from animal or human tissue). The decision to replace a valve with a mechanical or biological one depends on factors such as age, medical history, and lifestyle.
Heart valve disease occurs when one or more of the valves in the heart are no longer able to function properly. The reasons behind this valve dysfunction can vary widely, from degeneration over time to congenital defects.
Causes of Heart Valve Disease
-
Aortic Stenosis:
-
Aortic stenosis is the narrowing of the aortic valve, often caused by calcification (calcium buildup) over time. This causes the valve to become stiff, which limits its ability to open properly, restricting blood flow from the heart to the rest of the body.
-
-
Mitral Regurgitation:
-
Mitral regurgitation occurs when the mitral valve does not close properly, allowing blood to leak backward into the left atrium. This can lead to heart failure and is often caused by mitral valve prolapse, where the valve bulges into the left atrium during contraction.
-
-
Congenital Valve Defects:
-
Some individuals are born with heart valve abnormalities, such as a bicuspid aortic valve (a valve with only two leaflets instead of three), which can lead to stenosis or regurgitation over time.
-
-
Rheumatic Fever:
-
Rheumatic fever, a complication of strep throat infection, can lead to inflammation and scarring of the heart valves, causing valve disease, especially in the mitral valve.
-
-
Endocarditis:
-
Endocarditis, an infection of the inner lining of the heart, can damage or infect heart valves, leading to valve disease.
-
-
Aging:
-
As individuals age, the heart valves may become thicker, stiffer, or develop calcium deposits. These degenerative changes can lead to valve dysfunction, particularly in the aortic and mitral valves.
-
Risk Factors for Heart Valve Disease
-
Age:
-
The risk of heart valve disease increases with age, particularly for conditions like aortic stenosis or calcific valve disease.
-
-
Family History:
-
A family history of heart valve disease or certain heart conditions can increase an individual's risk of developing heart valve problems.
-
-
High Blood Pressure (Hypertension):
-
Hypertension can contribute to the deterioration of the heart valves, particularly the mitral and aortic valves, over time.
-
-
Coronary Artery Disease:
-
Coronary artery disease can affect the function of the heart valves, particularly the aortic valve.
-
-
Cholesterol:
-
High cholesterol levels can contribute to the development of atherosclerosis, which may affect the heart valves and lead to calcification, particularly in the aortic valve.
-
-
Congenital Defects:
-
Some people are born with heart valve abnormalities, such as bicuspid aortic valves, which increases their risk of needing valve replacement surgery as they age.
-
The symptoms of heart valve disease vary depending on the specific valve affected and the severity of the condition. In many cases, people with mild valve problems may not experience symptoms, while others may have significant health challenges that require heart valve replacement.
Common Symptoms of Heart Valve Disease
-
Shortness of Breath:
-
Difficulty breathing, particularly during physical activity or while lying flat, is a common symptom of heart valve disease. This occurs because the heart is unable to pump blood efficiently, leading to fluid buildup in the lungs.
-
-
Fatigue and Weakness:
-
Feeling unusually tired or weak, especially after minimal exertion, is a common symptom of valve problems due to the heart’s inability to supply enough oxygenated blood to the body.
-
-
Chest Pain:
-
Some individuals with heart valve disease experience chest pain or discomfort. This can occur when the heart is not getting enough oxygen or due to aortic stenosis causing restricted blood flow.
-
-
Swelling in the Legs, Abdomen, or Feet:
-
Swelling (edema) can occur when the heart is unable to pump blood effectively, causing fluid retention in the legs, feet, or abdomen.
-
-
Dizziness or Fainting:
-
Dizziness or fainting spells, especially during physical exertion, can occur when the heart is not able to supply adequate blood flow to the brain.
-
-
Heart Palpitations:
-
Irregular heartbeats or the sensation of a racing heart can be a sign of heart valve disease, especially in cases of mitral regurgitation or aortic stenosis.
-
-
Coughing:
-
Persistent coughing or wheezing, especially at night, can be a sign of fluid buildup in the lungs due to poor heart function.
-
Accurately diagnosing heart valve disease is essential to determine the most appropriate treatment, including the need for heart valve replacement. The diagnosis typically involves a combination of medical history, physical examination, and advanced diagnostic tests.
Diagnostic Methods
-
Physical Examination:
-
The doctor may detect signs of heart valve disease during a routine physical exam, including abnormal heart sounds (murmurs) or irregular heart rhythms, which can indicate valve dysfunction.
-
-
Echocardiogram:
-
An echocardiogram is a key diagnostic tool that uses sound waves to create detailed images of the heart’s structure and function. This test allows doctors to evaluate the condition of the heart valves, measure the degree of regurgitation or stenosis, and assess overall heart function.
-
-
Electrocardiogram (ECG/EKG):
-
An ECG records the electrical activity of the heart and can identify arrhythmias or other abnormalities caused by heart valve problems.
-
-
Chest X-Ray:
-
A chest X-ray can show the size and shape of the heart and detect fluid buildup in the lungs due to poor heart function.
-
-
Cardiac Catheterization (Angiography):
-
This procedure involves threading a catheter through the arteries to the heart and injecting a contrast dye to check for blockages or narrowing of the heart valves. It’s sometimes used when more information is needed before surgery.
-
-
MRI or CT Scan:
-
MRI or CT scans may be used to provide additional images of the heart and blood vessels, helping to evaluate the condition of the heart valves and plan for surgery.
-
The treatment for heart valve disease depends on the severity of the valve dysfunction and whether the patient has symptoms or other underlying conditions. When non-surgical treatments are insufficient, heart valve replacement is necessary.
Non-Surgical Treatment Options
-
Medications:
-
Diuretics may be prescribed to reduce fluid buildup in the body.
-
Beta-blockers and ACE inhibitors are used to control high blood pressure and reduce the strain on the heart.
-
Blood thinners (anticoagulants) may be prescribed for patients with certain types of valve disease to prevent blood clots.
-
-
Monitoring:
-
In some cases, especially when the valve dysfunction is mild, doctors may recommend regular monitoring with echocardiograms and other tests to track the disease progression.
-
Surgical Treatment: Heart Valve Replacement Surgery
Heart valve replacement surgery is necessary when the valve damage is severe and symptomatic. The two main types of valves used in replacement surgery are:
-
Mechanical Valves:
-
Mechanical heart valves are made from materials such as carbon and metal. These valves are durable and typically last a lifetime, but they require patients to take blood thinners to prevent clot formation.
-
-
Biological (Tissue) Valves:
-
Biological valves are made from animal tissues (usually pig or cow) or donated human tissue. While they may need to be replaced after 10-15 years, they do not require long-term blood thinner use.
-
Minimally Invasive Surgery:
-
In some cases, minimally invasive valve replacement techniques, including robotic surgery or transcatheter aortic valve replacement (TAVR), can be used. These methods involve smaller incisions and shorter recovery times compared to traditional open-heart surgery.
Preventing heart valve disease involves addressing risk factors and maintaining a healthy lifestyle.
Preventive Measures
-
Healthy Diet:
-
Eating a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats helps maintain healthy blood vessels and heart valves.
-
-
Regular Exercise:
-
Engaging in regular physical activity improves heart function, reduces cholesterol, and controls blood pressure.
-
-
Quit Smoking:
-
Smoking is a major risk factor for heart disease. Quitting smoking can significantly reduce the risk of developing heart valve disease and other cardiovascular conditions.
-
-
Manage Blood Pressure and Cholesterol:
-
Regular monitoring and management of blood pressure and cholesterol levels help prevent damage to the heart valves and arteries.
-
-
Early Detection:
-
Regular check-ups, particularly for individuals with a family history of heart disease, can help detect heart valve disease early, allowing for prompt intervention.
-
While heart valve replacement surgery is generally safe and effective, there are potential complications that patients should be aware of.
Potential Complications
-
Infection:
-
Infection can occur at the incision site or in the heart, though this is rare. Proper wound care and antibiotics are used to prevent infections.
-
-
Blood Clots:
-
After surgery, patients may be at risk for blood clots, particularly if mechanical valves are used. Blood thinners are typically prescribed to reduce this risk.
-
-
Bleeding:
-
As with any surgery, there is a risk of bleeding, particularly if the patient is on blood thinners or has other underlying health conditions.
-
-
Valve Dysfunction:
-
In rare cases, the new heart valve may not function properly, or it may wear out over time, necessitating additional surgery or valve replacement.
-
-
Stroke:
-
There is a small risk of stroke during or after surgery due to blood clots or complications in the blood flow.
-
After heart valve replacement, many patients can lead a normal, healthy life, but ongoing management and lifestyle changes are essential.
Post-Surgery Recovery
-
Hospital Stay:
-
Patients usually stay in the hospital for about 5 to 7 days after heart valve replacement surgery. During this time, doctors will monitor recovery and manage pain.
-
-
Physical Rehabilitation:
-
Cardiac rehabilitation programs help patients recover from surgery by improving cardiovascular fitness, strength, and endurance.
-
-
Regular Check-ups:
-
Regular follow-up visits with the healthcare provider are crucial to ensure the new valve is functioning correctly and to monitor heart health.
-
-
Dietary Adjustments:
-
After surgery, it is important to eat a heart-healthy diet to reduce the risk of further heart complications. A diet low in salt, saturated fat, and cholesterol is recommended.
-
1. What is heart valve replacement surgery?
Heart valve replacement surgery is a procedure used to replace a damaged or diseased heart valve. This surgery helps improve blood flow by correcting a faulty valve that may be causing problems like heart failure, chest pain, or shortness of breath. The two primary types of replacement valves are mechanical valves and biological valves (tissue valves).
2. Why do I need heart valve replacement surgery?
You may need heart valve replacement surgery if your heart valve is damaged, either due to wear and tear, an infection, or congenital heart defects. Symptoms of a malfunctioning valve can include fatigue, chest pain, dizziness, shortness of breath, and swollen ankles. If your heart valve cannot be repaired, surgery is often the best option to restore proper heart function.
3. What are the different types of heart valves used in the surgery?
The two main types of heart valves used in replacement surgery are:
-
Mechanical valves: Made from durable materials like titanium, carbon, or ceramics. These valves are long-lasting, but they require lifelong blood-thinning medications.
-
Biological valves: Made from animal tissue (such as pig or cow valves) or human donor tissue. They do not require blood thinners, but they may wear out over time, especially in younger patients.
4. What are the risks associated with heart valve replacement surgery?
While heart valve replacement surgery is generally safe, it carries risks such as infection, bleeding, stroke, blood clots, and damage to other heart structures. The risks depend on various factors, including the patient’s age, overall health, and the complexity of the surgery.
5. How is heart valve replacement surgery performed?
Heart valve replacement is performed under general anesthesia. The surgeon may use open-heart surgery, where a large incision is made in the chest, or minimally invasive surgery with smaller incisions. The damaged valve is removed and replaced with an artificial valve. In most cases, the patient is on a heart-lung machine to ensure blood circulation during the procedure.
6. What is the recovery time after heart valve replacement surgery?
Recovery time varies depending on the individual and the type of surgery performed. Generally, patients stay in the hospital for 5-7 days. Full recovery may take several weeks, with most people returning to normal activities within 3 to 6 months. It is important to follow all postoperative instructions, including lifestyle changes and rehabilitation, for the best recovery outcome.
7. What should I expect during the recovery process?
After surgery, patients are usually monitored in the hospital for several days. During recovery, you may experience some discomfort or fatigue, but this should improve over time. Your doctor may recommend physical therapy to help regain strength and mobility. Follow-up appointments are crucial to monitor the function of the new valve and ensure proper healing.
8. How long will a heart valve replacement last?
The lifespan of a heart valve replacement depends on the type of valve used. Mechanical valves can last 20-30 years or more, while biological valves typically last 10-20 years. Your doctor will monitor the valve over time, and if the valve wears out or becomes damaged, you may need a second replacement.
9. What lifestyle changes should I make after heart valve replacement surgery?
After surgery, you may need to make certain lifestyle changes to support your heart health. These can include maintaining a healthy diet, quitting smoking, exercising regularly (as advised by your doctor), and taking medications as prescribed. If you have a mechanical valve, you may need to take blood thinners for life to prevent blood clots.
10. Can heart valve replacement surgery be performed on elderly patients?
Yes, heart valve replacement surgery can be performed on elderly patients, although the risk of complications may be higher. In older adults, surgery may be performed with special considerations, and the decision is often based on the patient's overall health and other medical conditions. Many elderly patients benefit greatly from heart valve replacement surgery, improving their quality of life.


