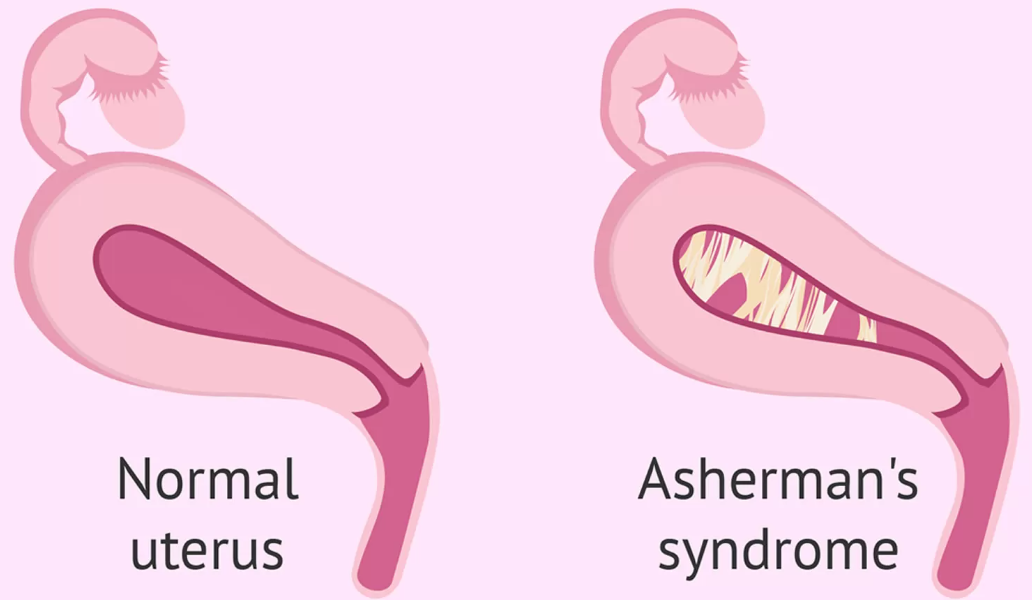
Asherman’s Syndrome, also referred to as intrauterine adhesions or synechiae, is a condition that occurs when scar tissue or adhesions form inside the uterus, leading to partial or complete closure of the uterine cavity. The adhesions develop in the endometrium (the inner lining of the uterus) and can cause a variety of complications, including infertility, miscarriage, and menstrual irregularities. In severe cases, Asherman’s Syndrome can lead to a complete inability to conceive or carry a pregnancy to term.
The condition was first described in 1948 by Dr. Joseph Asherman, a gynecologist who observed the association between uterine surgeries, especially dilation and curettage (D&C), and the formation of these intrauterine adhesions. While the condition is relatively rare, it is important for women to be aware of its potential risks, particularly after any uterine surgery or trauma.
Asherman’s Syndrome is a treatable condition, and with early diagnosis and appropriate intervention, most women can successfully recover and restore normal uterine function. However, timely medical intervention is critical, as untreated adhesions can have long-lasting impacts on a woman’s reproductive health.
Asherman’s Syndrome is most commonly caused by trauma to the uterus, often due to surgical procedures, infections, or other factors that damage the uterine lining. The severity of the condition depends on the location, extent, and depth of the adhesions. The primary causes of Asherman’s Syndrome are outlined below:
Primary Causes of Asherman’s Syndrome:
-
Dilation and Curettage (D&C):
-
The most common cause of Asherman’s Syndrome is a D&C procedure, which involves the dilation of the cervix and the scraping or suctioning of the uterine lining. This procedure is often performed after a miscarriage or for diagnostic purposes (such as abnormal uterine bleeding). However, the mechanical process of scraping the uterine wall can damage the endometrium, leading to the formation of scar tissue and adhesions.
-
-
Uterine Surgery:
-
Other types of uterine surgery, such as myomectomy (removal of uterine fibroids) or hysteroscopy, can also result in adhesions. Multiple surgeries increase the risk, particularly if they involve the inner lining of the uterus.
-
-
Infections:
-
Pelvic infections, particularly endometritis (infection of the uterine lining), can lead to scarring. Infections may occur after childbirth, miscarriage, or surgery. Chronic pelvic inflammatory disease (PID) or untreated sexually transmitted infections (STIs) can also damage the uterine lining and increase the likelihood of Asherman’s Syndrome.
-
-
Postpartum Complications:
-
Postpartum hemorrhage (excessive bleeding after childbirth) requiring surgical intervention such as D&C can increase the risk of uterine trauma and scarring, leading to Asherman’s Syndrome.
-
-
Abortion or Miscarriage Management:
-
After a miscarriage, a D&C may be performed to clear the uterine lining. In cases of multiple miscarriages or complications during miscarriage management, the risk of developing adhesions increases.
-
-
Trauma or Injury:
-
Any form of trauma to the uterus, such as accidental injury during miscarriage or surgery, can result in the development of scar tissue inside the uterine cavity.
-
Risk Factors for Asherman’s Syndrome:
-
Multiple Surgical Procedures:
-
Women who undergo multiple uterine surgeries, especially D&C, are at a higher risk of developing Asherman’s Syndrome. Each subsequent surgery increases the likelihood of uterine damage and scarring.
-
-
History of Infections:
-
Women with a history of chronic pelvic infections or STIs, especially gonorrhea or chlamydia, are at greater risk of developing adhesions after surgery or miscarriage.
-
-
Postpartum Complications:
-
Women who experience significant postpartum bleeding or require invasive procedures after childbirth (such as uterine evacuation or D&C) are more susceptible to Asherman’s Syndrome.
-
-
Prior Miscarriages:
-
Multiple miscarriages or complicated miscarriage management, particularly involving surgical intervention, increases the risk of uterine adhesions and Asherman’s Syndrome.
-
-
Cesarean Section:
-
Although rare, cesarean sections can sometimes contribute to adhesions, especially if there are complications during surgery, such as infection or injury to the uterine lining.
-
The symptoms of Asherman’s Syndrome vary widely based on the severity of the condition, the extent of the adhesions, and the presence of other underlying reproductive health issues. In some cases, women with Asherman’s Syndrome may not experience any symptoms, while in others, the condition may cause significant menstrual, fertility, and pregnancy-related issues.
Common Symptoms of Asherman’s Syndrome:
-
Amenorrhea (Absence of Menstrual Periods):
-
One of the most common signs of Asherman’s Syndrome is the absence of menstruation (amenorrhea). The adhesions in the uterus can block or restrict the shedding of the uterine lining, preventing the menstrual cycle from occurring.
-
-
Hypomenorrhea (Scanty Periods):
-
Women with Asherman’s Syndrome may experience very light or scanty periods (hypomenorrhea) due to the partial blockage of the uterine cavity. The adhesions reduce the surface area available for the endometrial lining to grow and shed.
-
-
Infertility:
-
Infertility is a common symptom, particularly in women with moderate to severe cases of Asherman’s Syndrome. Adhesions in the uterus can prevent the embryo from implanting properly or disrupt normal uterine function, making it difficult to achieve or maintain a pregnancy.
-
-
Recurrent Miscarriage:
-
Women with Asherman’s Syndrome are at increased risk of miscarriage, especially if the adhesions affect the lower part of the uterus or the cervix. The presence of scar tissue can interfere with implantation or the growth of the pregnancy.
-
-
Pelvic Pain or Discomfort:
-
Some women with Asherman’s Syndrome experience pelvic pain or discomfort, particularly during menstruation. The adhesions can restrict the movement of the uterine walls, leading to cramps or a feeling of fullness in the pelvis.
-
-
Dysmenorrhea (Painful Periods):
-
Women may experience painful menstruation (dysmenorrhea) due to adhesions obstructing normal menstrual flow. The buildup of blood in the uterus can lead to cramping or pain.
-
-
Difficulty During Labor:
-
In severe cases, Asherman’s Syndrome can cause difficulty during labor due to the reduced flexibility of the uterine walls caused by adhesions. This may result in complications, such as preterm labor or difficulty in delivery.
-
Diagnosing Asherman’s Syndrome requires a combination of clinical evaluation, imaging, and diagnostic tests. It’s important to accurately assess the extent and location of the adhesions to guide treatment decisions effectively.
Diagnostic Methods:
-
Hysterosalpingography (HSG):
-
Hysterosalpingography is a diagnostic X-ray procedure that is used to visualize the uterus and fallopian tubes. A contrast dye is injected into the uterus, and X-ray images are taken. In cases of Asherman’s Syndrome, the dye may be unable to pass through the uterus due to adhesions.
-
-
Hysteroscopy:
-
Hysteroscopy is the gold standard for diagnosing Asherman’s Syndrome. A small camera (hysteroscope) is inserted into the uterus through the cervix to directly visualize the uterine cavity. This allows the doctor to assess the extent and severity of adhesions and to potentially treat the condition during the procedure.
-
-
Ultrasound:
-
A transvaginal ultrasound can be used to assess the size and shape of the uterus and identify any abnormalities. In some cases, a saline infusion sonogram (SIS) may be performed, in which saline is introduced into the uterine cavity to create a clearer image of the inside of the uterus.
-
-
Magnetic Resonance Imaging (MRI):
-
MRI may be used for further detailed imaging of the uterus. While not typically used as the first line of diagnosis, it can be useful in complicated cases or to evaluate the surrounding tissues for additional abnormalities.
-
The treatment of Asherman’s Syndrome is focused on removing the adhesions and restoring normal uterine function. In most cases, surgical intervention is required, but other treatment options may be considered depending on the severity of the condition.
Surgical Treatments:
-
Hysteroscopic Adhesiolysis:
-
Hysteroscopic adhesiolysis is the most common treatment for Asherman’s Syndrome. During this procedure, a hysteroscope is inserted into the uterus to visualize the adhesions. Small instruments are used to cut or remove the adhesions, and the uterine cavity is restored to its normal state. This is usually done under general anesthesia.
-
-
Dilation and Curettage (D&C):
-
In some cases, a D&C may be performed after adhesiolysis to further remove any remaining tissue and to ensure that the uterine lining is completely cleared. However, the use of D&C should be minimized, as it can contribute to further scarring if done improperly.
-
-
Intrauterine Devices (IUDs):
-
After surgery, a hormonal intrauterine device (IUD) may be placed in the uterus to help prevent the formation of new adhesions. The IUD also helps keep the uterine cavity open and reduces the risk of further scarring.
-
Non-Surgical Treatments:
-
Hormonal Therapy:
-
Following surgery, hormonal therapy (such as estrogen) may be prescribed to promote the growth of the endometrial lining. Estrogen helps stimulate the growth of the uterine lining, which is necessary for proper menstrual function and fertility.
-
-
Fertility Treatments:
-
Women with Asherman’s Syndrome who wish to conceive may require fertility treatments such as in vitro fertilization (IVF). IVF can bypass some of the issues caused by adhesions and help facilitate conception.
-
While it’s not always possible to prevent Asherman’s Syndrome, certain strategies can reduce the risk and improve management after treatment.
Prevention:
-
Minimize Uterine Surgery:
-
Reducing the number of uterine surgeries (especially D&C) can decrease the risk of adhesions. If possible, alternative, non-invasive treatments should be considered.
-
-
Proper Infection Management:
-
Prompt and effective treatment of infections, particularly pelvic infections, can help prevent the formation of scar tissue in the uterus.
-
-
Careful Postpartum Management:
-
Proper management of postpartum bleeding or any complications during labor can help reduce the risk of uterine trauma and Asherman’s Syndrome.
-
Management:
-
Regular Monitoring:
-
After treatment, regular follow-up appointments are essential to monitor the condition of the uterus and to check for the recurrence of adhesions. Imaging tests and hysteroscopies may be used to track progress.
-
-
Fertility Support:
-
For women with infertility due to Asherman’s Syndrome, fertility treatments and assisted reproductive technologies (ART) like IVF may be recommended to help achieve pregnancy.
-
If left untreated, Asherman’s Syndrome can lead to a variety of complications, affecting a woman’s fertility, menstrual cycles, and overall reproductive health. Some potential complications include:
-
Infertility:
-
Asherman’s Syndrome is a significant cause of infertility, as adhesions block the normal implantation of embryos or disrupt uterine function.
-
-
Recurrent Miscarriage:
-
Women with Asherman’s Syndrome are at higher risk of recurrent miscarriages due to the inability of the uterus to properly support a pregnancy.
-
-
Pregnancy Complications:
-
Asherman’s Syndrome can lead to complications during pregnancy, such as preterm labor, placental abnormalities, or intrauterine growth restriction (IUGR).
-
Living with Asherman’s Syndrome involves careful management and ongoing medical support. Women with this condition can still lead healthy and fulfilling lives, but it may require adjustments, especially if fertility is impacted.
Key Considerations for Living with Asherman’s Syndrome:
-
Mental Health Support:
-
Dealing with infertility or recurrent miscarriage due to Asherman’s Syndrome can be emotionally challenging. Psychological counseling or support groups for women facing fertility challenges can be helpful.
-
-
Post-Treatment Care:
-
After treatment, regular follow-up care is important to ensure the adhesions do not recur and that fertility is restored. Monitoring and maintaining overall uterine health are crucial for long-term success.
-
-
Supportive Care:
-
Women with Asherman’s Syndrome may need additional support, such as fertility treatments, counseling, and lifestyle changes, to manage the emotional and physical aspects of the condition.
-
1. What is Asherman’s Syndrome?
Asherman’s Syndrome is a rare condition that involves the formation of scar tissue (adhesions) inside the uterus, which can lead to infertility, recurrent miscarriages, or menstrual abnormalities. The scar tissue typically forms after a trauma to the uterus, such as a surgical procedure, infection, or a difficult childbirth.
2. What causes Asherman’s Syndrome?
The most common cause of Asherman’s Syndrome is a surgical procedure involving the uterus, such as a dilation and curettage (D&C), which is often performed after a miscarriage or childbirth. Other causes include infections that affect the uterus (like pelvic inflammatory disease), or any procedure that causes trauma to the uterine lining. The damage results in scar tissue formation, which can block the normal function of the uterus.
3. What are the symptoms of Asherman’s Syndrome?
The symptoms of Asherman’s Syndrome can vary depending on the severity of the adhesions and how much of the uterine lining is affected. Common symptoms include:
-
Absent or reduced menstrual flow (amenorrhea or hypomenorrhea)
-
Recurrent miscarriages
-
Infertility or difficulty getting pregnant
-
Pelvic pain or discomfort
-
Abnormal bleeding patterns
4. How is Asherman’s Syndrome diagnosed?
Asherman’s Syndrome is diagnosed through a combination of medical history, physical examination, and imaging tests. Common diagnostic procedures include:
-
Hysterosalpingography (HSG): An X-ray test that uses contrast dye to evaluate the inside of the uterus and fallopian tubes.
-
Hysteroscopy: A minimally invasive procedure in which a camera is inserted into the uterus to directly visualize any scar tissue or adhesions.
-
Ultrasound: A pelvic ultrasound may be used to assess the condition of the uterus and detect any abnormalities.
5. How is Asherman’s Syndrome treated?
Treatment for Asherman’s Syndrome typically involves surgical removal of the adhesions inside the uterus. This is done through a procedure called hysteroscopic adhesiolysis, in which a thin camera (hysteroscope) is used to cut and remove the scar tissue. In some cases, hormonal therapy (such as estrogen) may be used after surgery to encourage the regrowth of the uterine lining and prevent the adhesions from reforming.
6. What are the chances of pregnancy after treatment for Asherman’s Syndrome?
The chances of pregnancy after treatment depend on the severity of the adhesions and how much damage was done to the uterus. Many women can achieve pregnancy after treatment, particularly if the adhesions were mild and the uterine lining was restored. However, if the adhesions were extensive or affected the cervix or fallopian tubes, pregnancy may be more difficult. In some cases, assisted reproductive technologies (such as in vitro fertilization or IVF) may be recommended.
7. What are the risks of not treating Asherman’s Syndrome?
If left untreated, Asherman’s Syndrome can lead to severe complications, including:
-
Infertility or difficulty becoming pregnant
-
Recurrent miscarriages
-
Chronic pelvic pain
-
Permanent damage to the uterine lining, which could make it more difficult to carry a pregnancy to term
-
Increased risk of complications during pregnancy, such as placental issues or preterm labor
8. Can Asherman’s Syndrome recur after treatment?
Yes, it is possible for Asherman’s Syndrome to recur after treatment, especially if the underlying causes, such as infections or repeated uterine procedures, are not addressed. To reduce the risk of recurrence, doctors may recommend hormone therapy (estrogen) after surgery to promote proper healing of the uterine lining and prevent the formation of new adhesions. Close follow-up with a doctor is essential to monitor for any signs of recurrence.
9. Can Asherman’s Syndrome be prevented?
While it is not always possible to prevent Asherman’s Syndrome, there are steps that can reduce the risk:
-
Avoid unnecessary uterine procedures: Minimizing the number of D&Cs or other surgeries that involve the uterus can help prevent injury and scarring.
-
Prompt treatment of uterine infections: Treating any infections that affect the uterus promptly can reduce the risk of adhesions forming.
-
Careful surgical techniques: When surgical procedures are necessary, using the least invasive methods possible can reduce the risk of uterine damage.
10. What is the outlook for women with Asherman’s Syndrome?
The outlook for women with Asherman’s Syndrome depends on the severity of the adhesions, the extent of uterine damage, and how early treatment is initiated. Many women who receive treatment for Asherman’s Syndrome can recover normal uterine function and achieve pregnancy. However, the chances of success can vary, and in some cases, assisted reproductive techniques may be necessary. Regular follow-up care is essential to ensure that any complications are detected early and treated appropriately.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


