Testicular Sperm Aspiration (TESA) is a medical procedure used to retrieve sperm directly from the testicles in cases where sperm is not present in the ejaculate. This technique is typically used for men with azoospermia (a condition where no sperm is present in the semen) due to obstructive or non-obstructive causes. TESA is a critical part of assisted reproductive technology (ART) and is frequently used in combination with in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI).
In TESA, sperm is extracted from the testicles through a needle aspiration technique. The procedure is minimally invasive and is performed under local anesthesia or mild sedation. It offers an option for men who are either unable to ejaculate sperm or whose sperm production is limited to the testicles due to a blockage or other factors affecting the reproductive system.
TESA can be the first step for men with azoospermia who wish to become fathers, providing them with the opportunity to use their sperm in IVF or ICSI cycles. This procedure has made it possible for many men with previously unmanageable infertility issues to successfully father biological children.
TESA is used primarily for men with azoospermia. The causes of azoospermia can be broadly classified into two categories: obstructive azoospermia and non-obstructive azoospermia. The underlying causes of these conditions determine whether TESA will be an effective sperm retrieval method.
1. Obstructive Azoospermia:
-
Vasectomy: One of the most common causes of obstructive azoospermia is a vasectomy, a surgical procedure in which the vas deferens (the tube that carries sperm from the testicles to the urethra) is cut or blocked. While this prevents sperm from being present in the ejaculate, sperm may still be found in the testicles, making TESA a viable solution for sperm retrieval.
-
Congenital Absence of Vas Deferens (CAVD): Some men are born with a congenital absence of the vas deferens, leading to azoospermia. In these cases, sperm can often be retrieved from the testicles using TESA.
-
Infections and Blockages: Infections, such as epididymitis or orchitis, or physical trauma to the reproductive system may cause blockages in the epididymis or vas deferens, preventing sperm from reaching the ejaculate.
-
Surgical Blockages: Blockages caused by previous surgeries or other medical conditions affecting the reproductive tract may require TESA for sperm retrieval.
2. Non-Obstructive Azoospermia:
-
Testicular Failure: Non-obstructive azoospermia occurs when the testicles are unable to produce sperm, often due to genetic factors, hormonal imbalances, or testicular damage. This can occur in conditions like Klinefelter syndrome, Y chromosome microdeletions, or chemotherapy treatments for cancer. Although sperm production may be impaired, TESA can sometimes retrieve viable sperm directly from the testicles, depending on the extent of damage to the reproductive cells.
-
Genetic Disorders: Men with genetic conditions affecting sperm production, such as Y-chromosome microdeletions, may still have some sperm present in the testicles, making TESA a suitable option.
-
Hormonal Imbalances: Low levels of testosterone or other hormonal imbalances can impair sperm production. TESA may be used to extract sperm if production is still occurring at a low level within the testicles.
3. Other Risk Factors:
-
Age: While age is typically a more significant factor for women in fertility, male fertility also tends to decline with age. This is especially true for men over 40, who may experience decreased sperm quality or production, which may require TESA.
-
Exposure to Toxins: Environmental factors, such as prolonged exposure to chemicals, radiation, or heavy metals, can impair sperm production. These factors can also cause testicular damage, making TESA necessary for sperm retrieval.
-
Previous Injury: Physical trauma to the testicles, such as injury from accidents or surgery, can lead to scarring or blockage, which may require TESA for sperm retrieval.
TESA is a procedure performed to address male infertility issues, so the symptoms associated with the procedure usually stem from the underlying condition causing azoospermia. Infertility, particularly the inability to conceive despite prolonged efforts, is the primary symptom prompting TESA.
1. Symptoms Indicating the Need for TESA:
-
Inability to Conceive: The most common symptom prompting TESA is infertility, specifically azoospermia, where no sperm is present in the ejaculate. A semen analysis showing no sperm is the main indication that sperm retrieval is needed.
-
Absence of Sperm in Semen: The absence of sperm in the ejaculate during a semen analysis can signal a blockage or dysfunction in the male reproductive system, prompting further evaluation and potential sperm retrieval via TESA.
-
Previous Vasectomy: Men who have had a vasectomy and later wish to have children may find that sperm retrieval through TESA is the most viable option for conception.
2. Post-Procedure Symptoms:
-
Mild Pain or Discomfort: Following TESA, some men may experience mild discomfort or tenderness in the scrotal area. This is typically short-lived and can be managed with over-the-counter pain medications.
-
Swelling or Bruising: Minor swelling or bruising around the needle insertion site is common but resolves in a few days.
-
Infection Risk: Although rare, there is a slight risk of infection after the procedure, which may present as redness, warmth, or fever. This can be managed with antibiotics if necessary.
The diagnosis for the need for TESA begins with a comprehensive fertility evaluation to assess the cause of azoospermia and determine whether TESA is the appropriate sperm retrieval method.
1. Semen Analysis:
-
The first step in diagnosing azoospermia is a semen analysis. If sperm is absent in the ejaculate, further diagnostic tests are conducted to determine whether the cause is obstructive (blockage) or non-obstructive (failure of sperm production).
2. Hormonal Testing:
-
Blood tests to measure testosterone, FSH (Follicle Stimulating Hormone), and LH (Luteinizing Hormone) levels help assess sperm production and hormonal imbalances. These results can provide important information about whether sperm production is occurring in the testicles and if TESA is appropriate.
3. Genetic Testing:
-
Genetic tests may be performed to identify Y chromosome microdeletions or other genetic factors that could contribute to azoospermia and inform whether TESA is a viable option.
4. Ultrasound Imaging:
-
A scrotal ultrasound helps to assess the testicles and epididymis for any blockages, cysts, or abnormalities that could affect sperm production or transport. In some cases, a testicular biopsy may be performed if sperm cannot be identified in the semen.
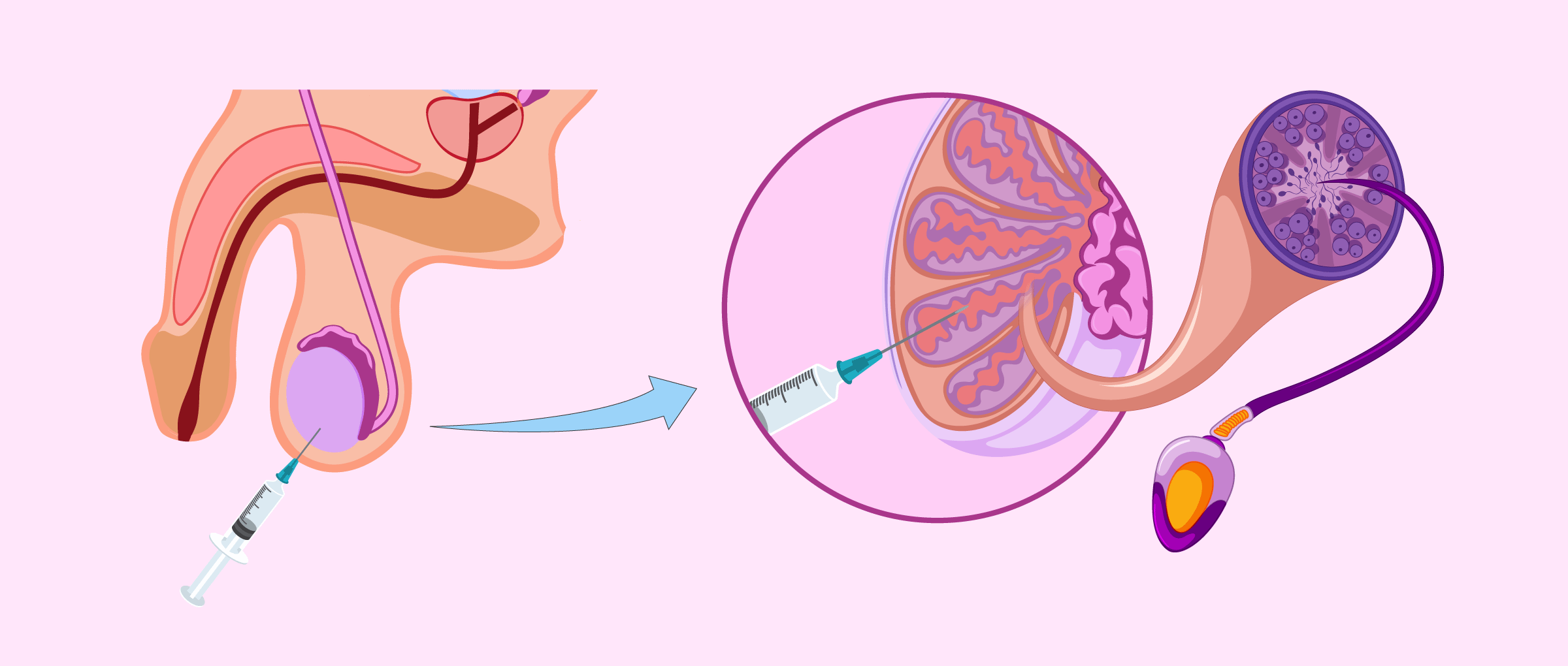
The TESA procedure is performed to extract sperm directly from the testicles. The following are the key steps involved in TESA:
1. Procedure Steps:
-
Local Anesthesia or Sedation: TESA is typically performed under local anesthesia to numb the area and minimize discomfort. In some cases, mild sedation may be used.
-
Needle Aspiration: A fine needle is used to aspirate sperm from the testicles. The procedure is minimally invasive and can be completed within a short time frame, typically under 30 minutes.
-
Microscopic Examination: The sperm retrieved via TESA is examined under a microscope to assess quality and viability before being used for IVF or ICSI (intracytoplasmic sperm injection).
2. IVF or ICSI:
-
The sperm retrieved through TESA is then used for IVF or ICSI. In ICSI, a single sperm is injected directly into an egg to facilitate fertilization. The resulting embryos are then cultured and transferred into the woman’s uterus.
3. Sperm Cryopreservation:
-
If sperm is successfully retrieved, it may be frozen and stored for future use, allowing the couple to undergo IVF or ICSI treatments at a later time.
While TESA itself cannot prevent infertility, there are several strategies to manage male reproductive health and improve the chances of success:
1. Healthy Lifestyle:
-
Diet and Exercise: A balanced diet rich in antioxidants, vitamins, and minerals can improve sperm quality. Regular exercise helps maintain a healthy weight and supports overall reproductive health.
-
Avoiding Toxins: Smoking, excessive alcohol consumption, and drug use can negatively affect sperm quality. Limiting exposure to environmental toxins and heat (such as from laptops, hot tubs, or tight clothing) can improve fertility.
2. Medical Treatment of Underlying Conditions:
-
If the cause of azoospermia is related to blockages, infections, or varicocele, surgical or medical treatments may be available to correct the issue before sperm retrieval.
3. Genetic Counseling:
-
Men with genetic infertility issues should seek genetic counseling to understand the implications for future children and explore potential options for genetic testing and assisted reproduction.
While TESA is generally safe, there are some risks and potential complications associated with the procedure:
1. Infection:
-
As with any surgical procedure, there is a risk of infection at the needle insertion site. This is usually preventable with proper sterilization techniques and post-procedure care.
2. Bleeding or Hematoma:
-
Minor bleeding or the formation of a hematoma (a collection of blood) at the puncture site is common but typically resolves within a few days.
3. Testicular Injury:
-
Although rare, there is a small risk of testicular injury during the procedure, which may affect future fertility.
4. Low Sperm Retrieval Rates:
-
In some cases, sperm retrieval may fail if the testicles are not producing sperm or if sperm is not found in the sample.
Living with the decision to undergo TESA involves both emotional and practical considerations. The following aspects are important for individuals and couples undergoing TESA:
1. Emotional Support:
-
Infertility treatments, including TESA, can be emotionally taxing. It is important to seek psychological support or fertility counseling to cope with the emotional impact of the procedure.
2. Financial Considerations:
-
TESA and subsequent ART treatments can be costly. Couples should discuss the financial aspects of the procedure and explore insurance coverage options, if applicable.
3. Family Planning and Follow-Up:
-
After sperm retrieval, couples should discuss future family planning and IVF/ICSI treatments with their fertility specialist. Regular follow-up visits are important to monitor progress and address any concerns.
1. What is Testicular Sperm Aspiration (TESA)?
Testicular Sperm Aspiration (TESA) is a medical procedure used to retrieve sperm directly from the testicle in men who have difficulty producing sperm through ejaculation. It is typically used in cases of non-obstructive azoospermia, where there is a lack of sperm in the ejaculate due to sperm production issues, or in cases where less invasive methods of sperm retrieval have been unsuccessful.
2. Why is TESA needed?
TESA is recommended in cases where men have:
-
Non-obstructive azoospermia: This occurs when sperm is not produced in sufficient quantities or at all in the testicles.
-
Previous vasectomy: When sperm is no longer present in the ejaculate after a vasectomy, but sperm may still be present in the testicles.
-
Failed sperm retrieval attempts using less invasive techniques like PESA (Percutaneous Epididymal Sperm Aspiration).
-
Genetic or medical conditions affecting sperm production, such as Klinefelter syndrome or chemotherapy-induced infertility.
3. How is TESA performed?
TESA is a minimally invasive procedure performed under local anesthesia. A needle is inserted into the testicle, and a small sample of testicular tissue is aspirated (suctioned). The sample is then examined in the laboratory to check for viable sperm. If sperm are found, they can be used for in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
4. Is the TESA procedure painful?
TESA is generally well-tolerated because it is performed under local anesthesia, which numbs the area. Most men experience mild discomfort or soreness in the testicular area after the procedure, but the pain is usually minimal and can be managed with over-the-counter pain relievers. Sedation or general anesthesia may be used if the patient prefers or if the procedure is more complex.
5. How long does TESA take?
The TESA procedure typically takes about 15 to 30 minutes. The procedure itself is relatively quick, though it may take longer depending on the complexity of the case. After the procedure, the patient is usually monitored for a short time before being allowed to go home.
6. What are the success rates of TESA?
The success rates of TESA depend on the underlying cause of infertility and the quality of sperm retrieved. In cases of non-obstructive azoospermia, TESA can be successful in retrieving viable sperm in approximately 40-60% of cases. The retrieved sperm can then be used for IVF or ICSI. The overall success of achieving a pregnancy also depends on the woman’s fertility, the quality of the sperm, and the success of the IVF/ICSI procedure.
7. What are the risks and complications of TESA?
TESA is a relatively safe procedure, but like any surgery, it carries some risks:
-
Infection: There is a risk of infection at the needle insertion site, though this is rare.
-
Bleeding: Some bleeding or bruising may occur at the procedure site.
-
Damage to surrounding tissues: Although uncommon, there is a small risk of damaging the testicle or other nearby structures.
-
Pain: Mild to moderate pain or discomfort may occur after the procedure, but this can usually be managed with medication.
8. How long does it take to recover from TESA?
The recovery time for TESA is typically short. Most men can resume normal activities within 1 to 2 days. However, it’s advisable to avoid strenuous activities or heavy lifting for about a week. Soreness or bruising in the testicular area may last for a few days but usually resolves on its own. It’s important to follow the aftercare instructions provided by the fertility clinic to minimize the risk of complications.
9. Can sperm from TESA be used for IVF or ICSI?
Yes, sperm retrieved through TESA can be used for assisted reproductive techniques such as IVF (in vitro fertilization) or ICSI (intracytoplasmic sperm injection). ICSI is particularly useful when sperm quality is poor or when only a small number of sperm are retrieved. In ICSI, a single sperm is injected directly into an egg to facilitate fertilization.
10. What happens if sperm cannot be retrieved with TESA?
If sperm cannot be retrieved with TESA, alternative methods may be considered, such as:
-
Testicular Sperm Extraction (TESE): A more invasive procedure where tissue is surgically removed from the testicle for sperm retrieval.
-
Donor sperm: If no viable sperm can be retrieved, the couple may consider using donor sperm for IVF or ICSI.
- In vitro fertilization (IVF)
- Percutaneous Epididymal Sperm Aspiration (PESA)
- Laser Assisted Hatching …etc
- Jinemed Hospital
- Women's Health & Fertility Centre Pte Ltd
- Jindal Heart Institute & Test Tube Baby Centre
- Apollo Fertility and IVF Center
- Bangkok IVF Center
- Lilavati Assisted Conception Unit
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.