Alzheimer’s Disease is a progressive neurodegenerative disorder that causes the brain to shrink (atrophy) and brain cells to die. It is the most common cause of dementia, which is a general term for a decline in cognitive ability that interferes with daily life. The disease is named after Alois Alzheimer, a German psychiatrist who first identified the condition in 1906.
Alzheimer's disease primarily affects older adults, although it can occasionally occur in younger people, known as early-onset Alzheimer's. It typically starts with mild memory loss and confusion but gradually worsens over time, leading to severe memory loss, impaired thinking, disorientation, and changes in behavior. The disease often makes it difficult for individuals to perform everyday tasks, leading to a significant loss of independence.
There is no known cure for Alzheimer’s disease, and while treatments can help manage symptoms, they cannot stop or slow down the progression of the disease. Alzheimer's disease is a leading cause of death worldwide, with millions of people affected.
The exact cause of Alzheimer’s disease is still not fully understood, but research has identified several factors that increase the risk of developing the disease. These factors are usually a combination of genetic, environmental, and lifestyle-related elements.
Causes of Alzheimer’s Disease:
-
Genetic Factors:
-
Alzheimer’s disease has a genetic component, and people with a family history of Alzheimer’s are at an increased risk of developing the disease. Certain genes, such as the APOE ε4 allele, are associated with an increased risk of developing Alzheimer's, although not everyone with these genes will develop the disease.
-
Early-onset Alzheimer's (before age 65) is often caused by specific genetic mutations that can be inherited, but this form of the disease is rare.
-
-
Abnormal Protein Deposits:
-
Alzheimer's disease is characterized by the accumulation of two abnormal proteins in the brain:
-
Amyloid plaques: Clusters of protein fragments that build up between nerve cells, blocking communication.
-
Tau tangles: Twisted strands of tau proteins that accumulate inside brain cells, disrupting their function.
-
-
These protein deposits disrupt communication between brain cells and lead to cell death.
-
-
Brain Changes:
-
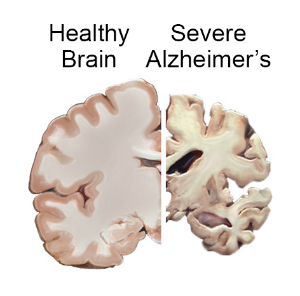
In Alzheimer’s disease, there is a significant loss of brain cells and connections between them. The brain regions responsible for memory, thinking, and behavior, such as the hippocampus and cortex, are most affected.
-
Risk Factors for Alzheimer’s Disease:
-
Age:
-
Age is the most significant risk factor for Alzheimer’s. The likelihood of developing the disease increases significantly after the age of 65, and the risk continues to rise with age.
-
-
Family History and Genetics:
-
Having a first-degree relative (such as a parent or sibling) with Alzheimer’s increases an individual’s risk, particularly if multiple family members are affected.
-
The presence of the APOE ε4 gene increases the likelihood of developing Alzheimer’s, though it does not guarantee that an individual will develop the disease.
-
-
Gender:
-
Women are at a higher risk than men, and they tend to develop Alzheimer’s at an older age. It is not entirely clear why women are more likely to develop the disease, but hormonal differences and longer life expectancy may play a role.
-
-
Down Syndrome:
-
People with Down syndrome are at a higher risk of developing Alzheimer’s disease due to having an extra copy of chromosome 21, which carries the gene responsible for producing amyloid plaques.
-
-
Head Trauma:
-
A history of severe or repeated head trauma may increase the risk of developing Alzheimer’s disease, especially if the injuries occur in middle age or earlier.
-
-
Lifestyle Factors:
-
Poor cardiovascular health, lack of physical activity, smoking, and a poor diet can all contribute to an increased risk of Alzheimer’s. These factors can affect blood flow to the brain and lead to brain cell damage.
-
Alzheimer’s disease progresses in stages, with symptoms becoming more severe over time. The symptoms often start subtly but progressively interfere with daily activities.
Early Symptoms (Mild Stage):
-
Memory Loss:
-
Forgetting recent conversations, appointments, and events, or misplacing items frequently.
-
-
Difficulty with Familiar Tasks:
-
Individuals may have trouble with tasks they’ve done for years, such as preparing meals, driving, or balancing a checkbook.
-
-
Disorientation:
-
Confusion about the time of day, places, or the identity of people.
-
-
Language Problems:
-
Difficulty finding the right words or following conversations.
-
-
Misplacing Objects:
-
Individuals may put things in unusual places and have difficulty retracing their steps to find them.
-
Moderate Symptoms (Moderate Stage):
-
Increased Memory Loss and Confusion:
-
Loss of short-term memory becomes more profound, and individuals may forget family members’ names or important personal details.
-
-
Difficulty Recognizing Family and Friends:
-
Alzheimer’s patients may lose recognition of close family members and friends.
-
-
Behavioral Changes:
-
Increased mood swings, depression, anxiety, agitation, and even paranoia may emerge.
-
-
Wandering and Getting Lost:
-
People with Alzheimer’s may wander off and get lost, even in familiar places, due to a lack of spatial awareness.
-
Severe Symptoms (Severe Stage):
-
Inability to Communicate:
-
Complete loss of verbal communication or ability to understand language.
-
-
Loss of Physical Abilities:
-
In the later stages, individuals may lose the ability to walk, feed themselves, or control bowel and bladder functions.
-
-
Severe Memory Loss:
-
Most memory functions are lost, and the individual may not recognize themselves or others.
-
Diagnosing Alzheimer’s disease involves ruling out other potential causes of symptoms and using various cognitive and imaging tests. Early diagnosis is crucial in planning treatment options and understanding the progression of the disease.
Diagnostic Steps:
-
Medical History:
-
The doctor will review the patient’s medical history, family history of Alzheimer’s, and any changes in memory or behavior.
-
-
Physical and Neurological Exam:
-
A physical exam, including checking for signs of other diseases, and a neurological exam to assess cognitive function and movement skills, is performed.
-
-
Cognitive and Memory Tests:
-
Mini-Mental State Examination (MMSE) and other cognitive tests help assess memory, problem-solving, and orientation.
-
-
Imaging Tests:
-
MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans are used to look for signs of brain shrinkage or other abnormalities.
-
PET scans can detect amyloid plaques in the brain, which are characteristic of Alzheimer’s.
-
-
Blood Tests:
-
Blood tests can help rule out other conditions that might cause similar symptoms, such as thyroid disorders or vitamin deficiencies.
-
-
Genetic Testing:
-
In some cases, genetic testing may be done, especially in individuals with a family history of early-onset Alzheimer’s.
-
Although there is no cure for Alzheimer’s, there are several treatments that can help manage symptoms, slow down progression, and improve quality of life.
Medications for Alzheimer’s Disease:
-
Cholinesterase Inhibitors:
-
Medications like Donepezil, Rivastigmine, and Galantamine are used to increase the level of acetylcholine in the brain, which helps with memory and cognition.
-
-
Glutamate Regulators:
-
Memantine is a drug that works by regulating the activity of glutamate, a neurotransmitter involved in learning and memory. It is often prescribed for moderate to severe Alzheimer’s.
-
-
Antidepressants, Anti-anxiety, and Antipsychotic Medications:
-
These medications can help manage mood swings, anxiety, depression, and agitation, which are common in Alzheimer’s patients.
-
Non-Pharmacological Therapies:
-
Cognitive Stimulation Therapy (CST):
-
Engaging in activities that challenge cognitive function, such as puzzles, memory exercises, and group activities, can help maintain mental function.
-
-
Behavioral Therapy:
-
Techniques to manage challenging behaviors, including wandering, agitation, and sleep disturbances, can improve the quality of life for both patients and caregivers.
-
-
Occupational Therapy:
-
Occupational therapists can help patients maintain their independence by suggesting strategies to perform daily tasks safely.
-
Although there is no known cure, certain lifestyle changes may help reduce the risk or delay the onset of Alzheimer’s disease.
Prevention Strategies:
-
Physical Activity:
-
Regular exercise improves brain health by boosting blood flow and reducing the risk of cognitive decline.
-
-
Healthy Diet:
-
A balanced diet rich in antioxidants, healthy fats (such as those found in the Mediterranean diet), and vitamins can help protect brain health.
-
-
Mental Stimulation:
-
Learning new skills, engaging in social activities, and keeping the mind active through reading, puzzles, and strategy games can help maintain cognitive function.
-
-
Adequate Sleep:
-
Sleep plays an essential role in brain health. Quality sleep helps clear toxins from the brain, including amyloid plaques associated with Alzheimer’s.
-
-
Chronic Disease Management:
-
Managing conditions like diabetes, high blood pressure, and high cholesterol can lower the risk of Alzheimer’s.
-
As Alzheimer's disease progresses, it leads to various complications that impact the health and well-being of the patient.
-
Physical Decline:
-
As the disease advances, mobility issues and the loss of motor skills make it difficult for patients to perform daily activities.
-
-
Infections:
-
Alzheimer’s patients are at higher risk of infections such as pneumonia, often due to swallowing difficulties or limited mobility.
-
-
Malnutrition and Dehydration:
-
As cognitive abilities decline, patients may forget to eat or drink, leading to malnutrition and dehydration.
-
-
Psychological Effects:
-
Alzheimer’s can lead to severe anxiety, depression, and mood swings, impacting both patients and their families.
-
Living with Alzheimer’s disease presents challenges for both the individual and their family. However, with proper care, the quality of life can be significantly improved.
For Patients:
-
Managing Daily Life:
-
Routine and structure are key. Patients can benefit from memory aids, calendars, and reminder systems to help them navigate their day.
-
-
Family and Caregiver Support:
-
Family members and caregivers play a critical role in providing care. It’s important for them to manage stress and seek respite care when needed.
-
For Caregivers:
-
Emotional Support:
-
Alzheimer’s caregiving can be emotionally draining. Caregivers should seek emotional support from support groups or professional counseling to prevent burnout.
-
-
Education and Resources:
-
Learning about the disease and available treatment options can help caregivers provide the best care for their loved one.
-
1. What is Alzheimer’s disease?
Alzheimer’s disease is a progressive neurodegenerative disorder that affects the brain, leading to memory loss, cognitive decline, and behavioral changes. It is the most common cause of dementia, a condition characterized by a decline in memory and thinking skills that interferes with daily life. Alzheimer’s typically affects older adults, but early-onset cases can also occur.
2. What are the early signs of Alzheimer’s disease?
Early signs of Alzheimer’s disease can include:
-
Memory loss that disrupts daily activities, such as forgetting recent conversations or appointments.
-
Difficulty completing familiar tasks at home or work.
-
Confusion with time or place, such as forgetting the date or getting lost in familiar locations.
-
Trouble with language, like difficulty finding the right words in conversation.
-
Poor judgment or decision-making.
-
Changes in mood and personality, including increased anxiety, depression, or irritability.
3. What causes Alzheimer’s disease?
The exact cause of Alzheimer’s disease is not fully understood, but it is believed to involve a combination of genetic, lifestyle, and environmental factors. The disease is characterized by the buildup of abnormal proteins, such as amyloid plaques and tau tangles, in the brain. These protein deposits damage and disrupt communication between brain cells, leading to their death. Age is the biggest risk factor, but genetics, family history, and certain health conditions like cardiovascular disease can also play a role.
4. Who is at risk for developing Alzheimer’s disease?
The primary risk factors for Alzheimer’s disease include:
-
Age: The risk increases with age, especially after 65.
-
Family history: Having a parent or sibling with Alzheimer’s increases the likelihood of developing the disease.
-
Genetics: Specific genes, such as the APOE ε4 allele, have been linked to an increased risk of Alzheimer’s.
-
Lifestyle factors: Poor cardiovascular health, lack of physical activity, smoking, and high cholesterol can increase risk.
-
Head injuries: People who have had significant head injuries may have a higher risk of developing Alzheimer’s later in life.
5. How is Alzheimer’s disease diagnosed?
Alzheimer’s disease is diagnosed based on a combination of medical history, physical exams, cognitive tests, and imaging studies. The diagnosis typically involves:
-
Cognitive and neuropsychological tests: To assess memory, problem-solving skills, and other cognitive functions.
-
Blood tests: To rule out other conditions that may mimic Alzheimer’s symptoms.
-
Brain imaging: MRI or CT scans to check for brain changes or damage, and PET scans to detect amyloid plaques.
-
Genetic testing: In some cases, genetic tests may be done to identify risk genes, though this is not always necessary.
6. What treatments are available for Alzheimer’s disease?
While there is no cure for Alzheimer’s disease, there are treatments available to help manage symptoms and improve quality of life:
-
Medications: Drugs like donepezil (Aricept), rivastigmine (Exelon), and galantamine (Razadyne) can help improve memory and cognition by increasing levels of acetylcholine, a neurotransmitter involved in memory. Memantine (Namenda) may also be prescribed to help with symptoms in the moderate to severe stages.
-
Lifestyle interventions: Cognitive therapies, exercise, a healthy diet, and social engagement can help slow progression and improve overall well-being.
-
Supportive care: Helping patients with daily tasks and providing a structured environment can help improve their quality of life.
7. Can Alzheimer’s disease be prevented?
While there is no guaranteed way to prevent Alzheimer’s disease, certain lifestyle changes can reduce the risk or delay the onset of symptoms:
-
Physical exercise: Regular physical activity is associated with better brain health.
-
Healthy diet: A diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids may support brain function.
-
Mental stimulation: Keeping the brain active through learning, puzzles, or social interaction may help improve cognitive function.
-
Good sleep habits: Ensuring adequate, quality sleep is crucial for brain health.
-
Heart health: Managing blood pressure, cholesterol, and blood sugar levels can reduce the risk.
8. What are the stages of Alzheimer’s disease?
Alzheimer’s disease progresses through several stages:
-
Early (Mild) Stage: Symptoms are subtle and may include memory loss, difficulty with familiar tasks, and changes in mood.
-
Middle (Moderate) Stage: Cognitive decline becomes more pronounced, with increased memory loss, confusion, and difficulty recognizing loved ones. Patients may also experience behavioral changes like agitation or anxiety.
-
Late (Severe) Stage: Individuals lose the ability to communicate and require full-time care. Physical abilities may be lost, and patients may no longer be able to walk or feed themselves.
9. What is the prognosis for someone with Alzheimer’s disease?
Alzheimer’s disease is progressive and currently irreversible. The course of the disease can vary widely from person to person, with some individuals living with mild symptoms for many years and others experiencing rapid cognitive decline. On average, people with Alzheimer’s live for 4 to 8 years after diagnosis, but some may live longer. Early diagnosis and intervention can improve the quality of life and extend the time a person remains independent.
10. How can caregivers support someone with Alzheimer’s disease?
Caregivers can play a crucial role in supporting individuals with Alzheimer’s by:
-
Providing emotional support: Offering reassurance, empathy, and understanding as the person copes with cognitive changes.
-
Creating a safe and structured environment: Minimizing confusion by establishing routines and ensuring the home is safe from hazards.
-
Encouraging engagement: Helping the person stay mentally and physically active by encouraging hobbies, exercise, and social interactions.
-
Seeking help and support: Caregivers should seek professional advice, join support groups, and take time for self-care to avoid caregiver burnout.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


