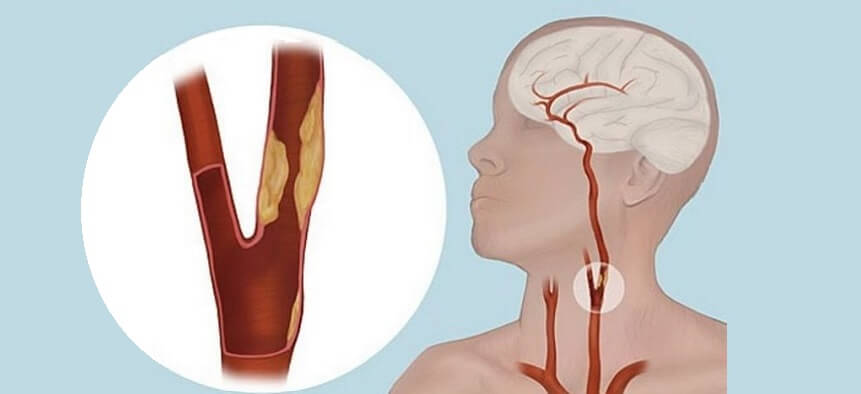
Carotid endarterectomy (CEA) is a surgical procedure aimed at treating carotid artery disease, a condition in which the carotid arteries, the main blood vessels supplying oxygenated blood to the brain, become narrowed or blocked. The narrowing is usually caused by the build-up of fatty deposits, cholesterol, and other substances, which forms a plaque in the arteries—a process known as atherosclerosis.
The purpose of a carotid endarterectomy is to remove the plaque from the affected carotid artery to restore normal blood flow to the brain. By doing so, the procedure reduces the risk of a stroke, which can occur when the blood supply to the brain is compromised.
Carotid endarterectomy is typically performed in patients who have a high-grade stenosis (severe narrowing) of the carotid artery, especially those who have experienced a transient ischemic attack (TIA) or a stroke. The procedure can prevent further neurological damage by restoring blood flow to the brain.
As a commonly performed neurosurgical procedure, carotid endarterectomy has been proven effective in reducing the incidence of stroke in patients with significant carotid artery disease. However, it requires careful evaluation of the patient's overall health, degree of arterial narrowing, and associated risks.
Carotid artery disease and the need for carotid endarterectomy are usually caused by atherosclerosis or the build-up of plaque in the arteries. There are several causes and risk factors associated with carotid artery disease, leading to the necessity for carotid endarterectomy.
1. Atherosclerosis:
-
The main cause of carotid artery disease is atherosclerosis, which is the gradual accumulation of plaque (fatty deposits, cholesterol, and other substances) inside the arteries. As the plaque builds up, it narrows the arteries, restricting blood flow to the brain. This restriction can lead to stroke or transient ischemic attacks (TIAs). If a stenosis (narrowing) exceeds 60-70%, carotid endarterectomy may be recommended to reduce the risk of stroke.
2. High Blood Pressure (Hypertension):
-
High blood pressure is a significant risk factor for the development of atherosclerosis. It accelerates the process of plaque formation by damaging the blood vessel walls. Over time, high blood pressure increases the risk of stroke, particularly when associated with other risk factors such as high cholesterol or smoking.
3. High Cholesterol:
-
High cholesterol, especially low-density lipoprotein (LDL) or “bad cholesterol,” contributes significantly to the formation of plaque in the carotid arteries. Elevated cholesterol levels can lead to plaque buildup, narrowing the arteries and impeding blood flow.
4. Smoking:
-
Smoking is a major risk factor for atherosclerosis and carotid artery disease. It damages the lining of blood vessels, increases the formation of plaque, and raises blood pressure. Smokers are at a much higher risk of stroke and need to quit smoking to reduce the risks associated with carotid artery disease.
5. Diabetes:
-
Diabetes increases the likelihood of developing atherosclerosis by contributing to high blood sugar levels, which damage blood vessels and encourage plaque formation. Individuals with diabetes are at greater risk for carotid artery disease and its associated complications.
6. Age and Gender:
-
Age is a significant risk factor for carotid artery disease, with older individuals being at greater risk. The risk of developing atherosclerosis and narrowing of the carotid arteries increases with age. Men are generally more likely to develop carotid artery disease at a younger age than women, but the risk increases in women after menopause.
7. Family History:
-
A family history of cardiovascular disease, stroke, or carotid artery disease increases the likelihood of developing these conditions. Genetic factors can predispose individuals to high cholesterol, hypertension, or atherosclerosis, making them more susceptible to carotid artery disease.
8. Lack of Physical Activity and Poor Diet:
-
A sedentary lifestyle combined with an unhealthy diet high in saturated fats, trans fats, and processed foods contributes to the development of atherosclerosis. Lack of physical activity and poor diet can result in obesity, high cholesterol, and high blood pressure, which further increases the risk of carotid artery disease.
The symptoms that lead to a recommendation for carotid endarterectomy typically arise when there is significant narrowing or blockage in the carotid artery, which impairs blood flow to the brain. Some signs and symptoms include:
1. Stroke or Transient Ischemic Attack (TIA):
-
The most common and severe consequence of carotid artery disease is stroke. A TIA, also known as a mini-stroke, is a temporary blockage of blood flow to the brain and can serve as an early warning of a potential full stroke. Symptoms of stroke or TIA include:
-
Sudden weakness or numbness on one side of the body (face, arm, or leg).
-
Sudden difficulty speaking or understanding speech.
-
Sudden loss of vision in one or both eyes or double vision.
-
Dizziness, loss of coordination, or trouble walking.
-
2. Carotid Bruit:
-
A carotid bruit is an abnormal sound heard through a stethoscope when blood flow through the carotid artery is turbulent due to plaque buildup. A carotid bruit often indicates the presence of significant narrowing or blockage in the carotid artery.
3. Decreased Memory or Cognitive Function:
-
When blood flow to the brain is compromised, it can result in memory problems, confusion, or difficulty concentrating. Cognitive decline can be a sign of carotid artery disease affecting the brain’s ability to function normally.
4. Dizziness or Lightheadedness:
-
Reduced blood flow to the brain can cause dizziness, lightheadedness, or fainting, particularly when standing up quickly. These symptoms may indicate a blockage in the carotid artery and require evaluation.
5. Weakness or Numbness in the Limbs:
-
Weakness or numbness, particularly on one side of the body, is a common symptom of reduced blood flow caused by carotid artery disease. Patients may have trouble using their arms or legs effectively.
The diagnosis of carotid artery disease involves a combination of physical examinations, imaging tests, and diagnostic procedures to assess the severity of arterial narrowing and determine if surgery is necessary.
1. Physical Examination:
-
A healthcare provider will perform a neurological exam to assess signs of stroke or neurological deficits such as weakness, numbness, or changes in speech. Auscultation of the carotid artery with a stethoscope may reveal a carotid bruit if blood flow is turbulent due to plaque buildup.
2. Carotid Ultrasound:
-
Carotid ultrasound, or Doppler ultrasound, is a non-invasive imaging technique that uses sound waves to create an image of the carotid arteries and measure blood flow. It is the primary diagnostic tool for detecting carotid stenosis (narrowing) and assessing the degree of blockage.
3. CT Angiography (CTA) and MRI Angiography (MRA):
-
CT angiography (CTA) and MRI angiography (MRA) are advanced imaging techniques that provide detailed images of the carotid arteries, allowing doctors to assess the extent of the blockage or narrowing and plan for surgery if necessary.
4. Cerebral Angiography:
-
Cerebral angiography is a more invasive test that involves injecting a contrast dye into the carotid arteries and taking X-ray images to visualize the blood vessels. This test provides detailed information about the location and severity of blockages and is often used to guide treatment decisions.
Carotid endarterectomy is the primary surgical option for treating severe carotid artery disease that is at risk of causing stroke. However, other treatments may be considered based on the severity of the disease and the patient’s health.
1. Carotid Endarterectomy (CEA):
-
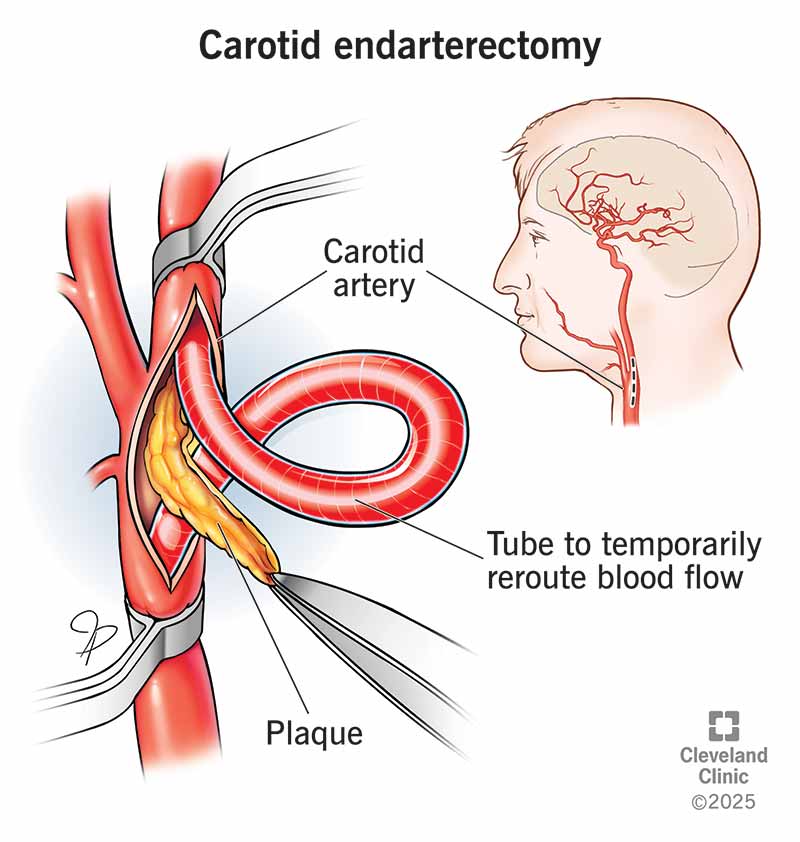
Carotid endarterectomy is the most common treatment for severe carotid artery stenosis. During the procedure, the surgeon makes an incision in the neck, exposes the carotid artery, and removes the plaque blocking the artery. The artery is then stitched back together to restore normal blood flow. This surgery is highly effective in preventing stroke in patients with 60-99% stenosis.
2. Carotid Artery Stenting (CAS):
-
Carotid artery stenting (CAS) is a less invasive procedure used to treat carotid artery disease. A catheter with a balloon is inserted through the groin to the affected carotid artery, and a stent is placed to open the narrowed artery. This procedure is often considered for patients who are not candidates for endarterectomy due to other health concerns.
3. Medications:
-
For less severe cases of carotid artery disease, medications such as statins (to lower cholesterol), antihypertensive drugs (to manage high blood pressure), and antiplatelet drugs (to prevent blood clots) may be prescribed. These medications help manage the condition and prevent further plaque buildup.
Preventing the need for carotid endarterectomy involves managing risk factors and adopting a heart-healthy lifestyle.
1. Healthy Lifestyle:
-
Diet: A healthy diet, low in saturated fats and high in fruits, vegetables, and whole grains, can help manage cholesterol and prevent plaque buildup in the arteries.
-
Exercise: Regular physical activity improves cardiovascular health and helps manage blood pressure, cholesterol, and weight.
2. Medication Adherence:
-
Taking prescribed medications such as statins, blood pressure medications, and antiplatelet agents can reduce the risk of further narrowing of the carotid arteries and prevent strokes.
3. Smoking Cessation:
-
Quitting smoking is crucial to reducing the risk of carotid artery disease and improving overall heart health.
4. Regular Monitoring:
-
Regular check-ups with your doctor, including routine ultrasound exams of the carotid arteries, can help monitor the progression of the disease and identify when surgery may be needed.
While carotid endarterectomy is generally a safe and effective procedure, there are risks associated with the surgery:
1. Stroke:
-
The risk of stroke during or immediately after surgery is present, though it is generally low. Stroke can occur due to the release of plaque debris during the surgery or from blood clots forming after the procedure.
2. Infection:
-
Infection at the incision site or in the blood vessels is a potential complication, though it is uncommon with proper surgical care.
3. Nerve Damage:
-
The vagus nerve, which controls swallowing and speech, and the facial nerve can be affected during the procedure, potentially causing temporary or permanent nerve damage.
4. Hematoma:
-
Hematoma (accumulation of blood) may form at the surgery site, requiring further treatment to drain the blood.
Living with the Condition of Carotid Endarterectomy
After undergoing carotid endarterectomy, patients will need to make lifestyle changes and engage in post-operative care to ensure optimal recovery and prevent the recurrence of carotid artery disease.
1. Post-Surgical Recovery:
-
Patients may experience mild discomfort or swelling at the incision site. Pain medications are typically prescribed, and the recovery period may take several weeks.
2. Rehabilitation:
-
Physical therapy may be recommended for patients who experience any weakness or limited mobility after surgery. Follow-up visits are necessary to monitor the patient’s recovery and manage any potential complications.
3. Ongoing Lifestyle Modifications:
-
Continuing a healthy diet, regular exercise, and taking medications as prescribed are crucial to prevent the progression of atherosclerosis and reduce the risk of further blockages.
1. What is Carotid Endarterectomy?
Carotid endarterectomy is a surgical procedure used to remove plaque (fatty deposits) from the carotid arteries, which supply blood to the brain. The procedure aims to reduce the risk of stroke by restoring normal blood flow to the brain. The plaque buildup can cause narrowing or blockage in the arteries, which increases the risk of stroke.
2. Why is Carotid Endarterectomy needed?
Carotid endarterectomy is typically recommended for individuals who have significant narrowing (stenosis) of the carotid arteries, which can lead to:
-
Stroke or transient ischemic attacks (TIAs), also known as mini-strokes.
-
Reduced blood flow to the brain, increasing the risk of cognitive decline or neurological problems.
-
Severe carotid artery disease, which may not be manageable with medication alone.
The surgery is especially beneficial for those with greater than 70% stenosis of the carotid artery.
3. How is Carotid Endarterectomy performed?
The surgery is performed under local or general anesthesia, depending on the patient’s preference and health condition. The steps typically involve:
-
An incision is made in the neck to expose the carotid artery.
-
The artery is carefully opened, and the plaque is removed.
-
After the plaque is cleared, the artery is sewn back together, and the incision is closed.
-
Sometimes, a patch graft may be used to widen the artery if it is too narrow after plaque removal.
4. What are the risks of Carotid Endarterectomy?
While Carotid Endarterectomy is generally safe, like any surgery, it carries some risks:
-
Stroke: There is a risk of stroke during or after the surgery, although it is low when performed by experienced surgeons.
-
Heart attack: Stress on the heart during surgery can lead to a heart attack, especially in those with existing heart disease.
-
Nerve damage: Injury to nearby nerves, causing issues like hoarseness or difficulty swallowing.
-
Infection: As with any surgery, there is a risk of infection at the incision site.
-
Bleeding: There could be bleeding at the surgery site, which may require further intervention.
5. How long does the surgery take?
Carotid endarterectomy typically takes 1 to 2 hours to complete, depending on the complexity of the case and the patient's specific condition. It is considered a relatively quick procedure compared to other types of surgeries.
6. What is the recovery process after Carotid Endarterectomy?
The recovery process varies but typically includes:
-
Hospital stay: Most patients spend 1-2 days in the hospital after surgery for monitoring and pain management.
-
Resuming normal activities: Patients can usually return to normal activities within 2-4 weeks. However, more strenuous physical activity may need to be avoided for 4-6 weeks.
-
Follow-up care: After surgery, follow-up appointments are necessary to monitor the healing process and ensure the artery remains clear.
7. What is the success rate of Carotid Endarterectomy?
Carotid endarterectomy has a high success rate. Studies show the procedure reduces the risk of stroke by as much as 70-80% in patients with significant carotid artery stenosis. The success of the surgery depends on factors like the severity of the blockage, the patient’s age, and any pre-existing health conditions.
8. How do I know if I need Carotid Endarterectomy?
If you have been diagnosed with carotid artery disease or have risk factors such as a history of strokes or transient ischemic attacks (TIAs), your doctor may recommend Carotid Endarterectomy. It is particularly considered if you have more than 70% narrowing of the carotid artery or if you’ve had a recent stroke or TIA. Your doctor will assess your overall health, including any heart or vascular conditions, to determine if surgery is appropriate.
9. What happens if Carotid Endarterectomy is unsuccessful?
While rare, if Carotid Endarterectomy is unsuccessful, there may be the possibility of:
-
Recurrent blockage: If the artery narrows again, additional procedures may be needed.
-
Stroke or neurological problems: In some cases, a stroke or neurological issue may occur despite the surgery.
If the surgery does not fully restore blood flow or if complications arise, your doctor may consider alternative treatments such as carotid artery stenting or further surgery.
10. Are there alternatives to Carotid Endarterectomy?
Yes, there are alternatives to Carotid Endarterectomy, such as:
-
Carotid artery stenting (CAS): A less invasive procedure where a stent (a small mesh tube) is placed in the artery to keep it open. This may be an option for patients who are not candidates for surgery or those with high surgical risk.
-
Medications: If the narrowing is not severe, medications like statins and blood thinners may be used to manage the condition and prevent complications.
-
Lifestyle changes: Diet, exercise, and managing blood pressure and cholesterol levels can also help reduce the risk of stroke and slow down the progression of carotid artery disease.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.