Belt Buckling Vitrectomy Endolaser is a specialized, combination procedure in ocular surgery that is often used to treat certain retinal disorders, particularly those caused by retinal detachment or vitreoretinal diseases. It is a hybrid technique that combines vitrectomy, retinal laser therapy, and scleral buckling to reattach the retina, treat vitreous problems, and stabilize the eye.
A vitrectomy involves the removal of the vitreous gel, a clear substance that fills the inside of the eye, to allow the surgeon better access to the retina. Endolaser photocoagulation is then used to apply a laser directly to the retina, promoting the formation of scars around the areas of retinal damage. Meanwhile, scleral buckling is the process of attaching a silicone band or other material around the eye to help the retina reattach by physically pushing the retina back toward the eye wall.
This combined technique is often utilized for conditions that affect the posterior segment of the eye, such as retinal detachments, macular holes, and certain types of diabetic retinopathy. The goal of Belt Buckling Vitrectomy Endolaser is to prevent further damage, improve visual outcomes, and stabilize the eye’s structure after damage to the retina or vitreous body.
While the procedure can be highly effective in treating retinal problems, it requires precision and expertise, as improper treatment could lead to complications, including vision loss or recurrence of the detachment.
Belt Buckling Vitrectomy Endolaser is typically used for patients with certain conditions that affect the retina or vitreous body of the eye. These conditions may be caused by a variety of factors, some of which are preventable, while others are not. The primary causes and risk factors for requiring this procedure include:
1. Retinal Detachment
Retinal detachment is the most common reason for performing this procedure. It occurs when the retina becomes separated from its underlying tissue. Trauma, eye injury, or increased pressure within the eye can lead to retinal tears or holes, causing fluid to leak beneath the retina and detaching it from the back of the eye.
2. Vitreous Detachment and Changes
The vitreous gel in the eye changes with age. As we age, the vitreous may shrink or liquefy, pulling away from the retina. In some cases, this can cause tears or holes in the retina, leading to a retinal detachment. Conditions like diabetic retinopathy or retinal vein occlusion can also lead to such changes.
3. Diabetic Retinopathy
Diabetic retinopathy is one of the leading causes of vision problems and blindness in people with diabetes. The high blood sugar levels can damage blood vessels in the retina, causing them to leak or become blocked. This damage can lead to retinal detachment, making the patient a candidate for procedures like vitrectomy and endolaser treatment.
4. Age-Related Macular Degeneration (AMD)
Although macular degeneration primarily affects the macula (the central part of the retina), advanced forms of AMD can cause complications that lead to retinal detachment. As the retinal tissue degenerates, it may increase the risk of developing holes or tears that could require a vitrectomy with laser treatment.
5. Trauma or Injury
Eye injuries, including blunt trauma or penetrating injuries, can cause tears in the retina, leading to retinal detachment. In such cases, vitrectomy with scleral buckling and endolaser photocoagulation may be used to treat and prevent further retinal damage.
6. Hereditary Conditions
Some genetic conditions, such as retinitis pigmentosa, Stickler syndrome, or Marfan syndrome, can increase the risk of retinal detachment due to weaknesses in the connective tissues or the vitreous gel of the eye.
7. Pre-existing Eye Conditions
Individuals with certain eye conditions, like high myopia (nearsightedness), may have a higher risk of retinal detachment. These patients tend to have thinner retinae, which can be more susceptible to tears or detachment under certain conditions.
Patients requiring Belt Buckling Vitrectomy Endolaser are often experiencing symptoms related to retinal detachment, vitreous abnormalities, or other related eye conditions. The most common symptoms associated with these conditions include:
1. Sudden Vision Loss
The most dramatic symptom of retinal detachment is a sudden loss of vision, often in one eye. This may be partial (loss of central or peripheral vision) or complete blindness in severe cases.
2. Floaters
Many people with retinal tears or detachments report seeing floaters—small, shadowy spots or strings in the vision. These are often the result of the vitreous gel pulling away from the retina or floating debris within the vitreous body.
3. Flashes of Light
Flashes of light in the vision (known as photopsia) can occur when the vitreous pulls on the retina, irritating the retina’s photoreceptor cells. This is commonly seen in patients with vitreous detachment or retinal tears.
4. Blurred Vision or Blind Spots
A blurred area or blind spot in the central or peripheral vision may appear. This can occur if the retina is partially detached or if there is swelling or fluid beneath the retina.
5. Dark Shadows or Curtains
A feeling of a dark curtain or shadow moving across the field of vision is another indication of retinal detachment. This phenomenon occurs when the retina begins to detach, obstructing light from reaching the photoreceptor cells.
6. Pain or Pressure
Although retinal detachment itself is often painless, the associated conditions or injuries leading to detachment may cause pain, pressure, or discomfort around the eyes or within the orbital cavity.
Early diagnosis of retinal detachment or other conditions requiring Belt Buckling Vitrectomy Endolaser is crucial for the success of the procedure and the preservation of vision. The diagnostic process involves a combination of physical exams, imaging tests, and sometimes special diagnostic tools.
1. Comprehensive Eye Exam
The first step in diagnosing conditions that require this procedure is a comprehensive eye exam. The ophthalmologist will assess visual acuity, examine the retina for tears or holes, and check for signs of detachment. This may involve dilating the pupils to examine the back of the eye.
2. Ultrasound
An ocular ultrasound can be used to assess the retina’s condition, especially when the retina is not visible due to hemorrhage or other eye conditions. This imaging tool helps the surgeon evaluate the extent of retinal detachment and decide on the appropriate course of action.
3. Optical Coherence Tomography (OCT)
OCT provides high-resolution images of the retina, allowing doctors to assess the thickness of the retina and any abnormal fluid accumulation or tears. This helps in determining whether a vitrectomy is necessary.
4. Fluorescein Angiography
This procedure involves injecting a fluorescent dye into the bloodstream and taking images of the retina as the dye travels through the blood vessels. It helps identify areas of damage or leakage within the retina, particularly in diabetic retinopathy.
5. Fundus Photography
Fundus photography allows for detailed images of the retina and optic disc to be captured, helping to monitor any retinal changes over time.
The treatment for conditions requiring Belt Buckling Vitrectomy Endolaser typically involves a combination of surgery and laser therapy to stabilize the retina and prevent further damage.
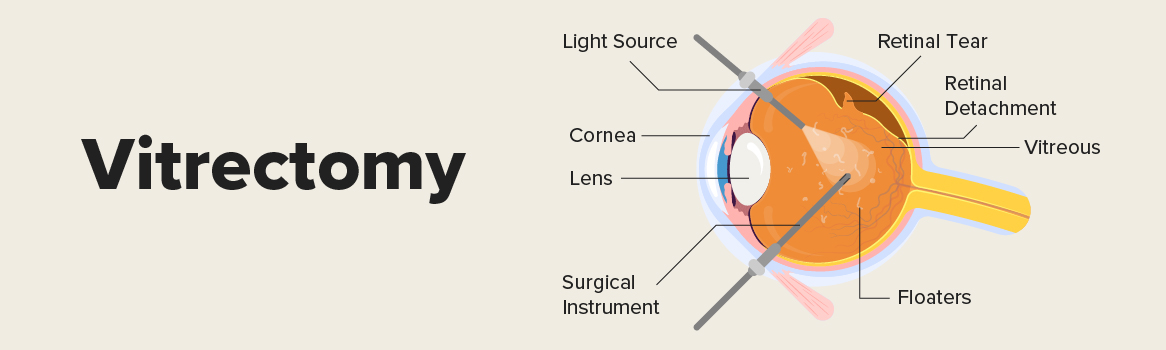
1. Vitrectomy
Vitrectomy is the main component of the procedure. It involves the removal of the vitreous gel from the eye to allow better access to the retina. This is necessary when the vitreous gel is causing traction or when blood or fluid has accumulated in the vitreous cavity.
2. Scleral Buckling
Scleral buckling is the process of placing a silicone band or another material around the eye to gently push the retina back into position. This helps relieve the traction and prevents further detachment. The band is typically left in place permanently.
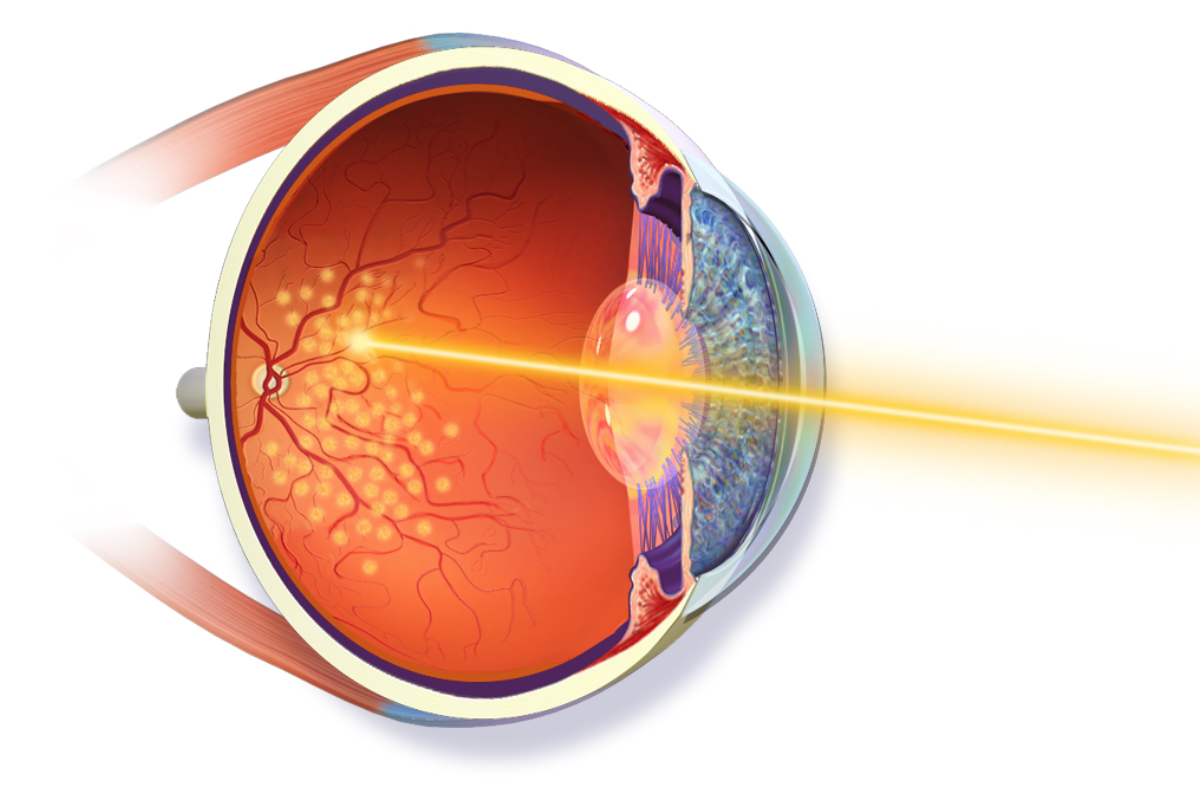
3. Endolaser Photocoagulation
After vitrectomy and scleral buckling, endolaser photocoagulation is applied to the retina. This laser treatment helps create scars around the tear or detachment site, effectively "welding" the retina back to the underlying tissue and preventing further separation. The laser can be applied directly to the retina during surgery.
4. Pneumatic Retinopexy
In some cases, a gas bubble may be injected into the eye to help push the retina back into place. This is often used in combination with laser therapy or scleral buckling.
5. Post-Surgical Care
After the procedure, patients typically need to remain in a specific head position for a period to allow the retina to settle in its proper position. Eye drops and medications to reduce inflammation and prevent infection are commonly prescribed.
While some conditions leading to Belt Buckling Vitrectomy Endolaser cannot be prevented, early detection and treatment of retinal problems can reduce the risk of requiring surgery. Regular eye exams, especially for individuals with high-risk factors like diabetes or a history of eye trauma, can help detect problems early.
1. Regular Eye Exams
Regular eye exams are crucial for individuals at risk of retinal diseases. Early detection of retinal tears, diabetic retinopathy, or macular degeneration can prevent further complications.
2. Managing Risk Factors
Proper management of underlying conditions such as diabetic retinopathy and hypertension can reduce the risk of retinal detachment. Control of blood sugar levels and blood pressure through lifestyle changes and medication is key.
3. Post-Surgical Care and Lifestyle Modifications
Following surgery, it’s important to follow the doctor’s instructions to ensure proper healing. This may include:
-
Restricting physical activity.
-
Avoiding sudden head movements.
-
Adhering to prescribed eye drops and medications.
Although Belt Buckling Vitrectomy Endolaser is generally effective, it carries some risks and potential complications, including:
1. Recurrence of Retinal Detachment
In some cases, retinal detachment can recur, requiring additional treatment or surgery.
2. Cataract Formation
One of the most common complications after vitrectomy is the development of a cataract, as the procedure can disrupt the natural lens of the eye.
3. Infection
As with any surgery, there is a risk of infection, which can lead to further complications such as loss of vision.
4. Increased Intraocular Pressure
After surgery, some patients may develop elevated intraocular pressure, which can lead to glaucoma if not properly managed.
5. Vision Impairment
Though rare, there can be a temporary or permanent decrease in vision due to complications during or after surgery, including the development of scar tissue or macular edema.
Living with the condition that necessitates Belt Buckling Vitrectomy Endolaser requires ongoing care and lifestyle adjustments. After surgery, patients need to make modifications in their daily activities and stay in touch with their eye care team for follow-up visits.
1. Emotional and Psychological Support
The emotional impact of losing vision or undergoing complex eye surgery can be significant. Support groups, therapy, and counseling can help patients manage stress, anxiety, and depression related to their visual impairment.
2. Rehabilitation
Vision rehabilitation may be needed after surgery to help the patient adjust to changes in their vision and maintain independence. This can include learning new techniques to compensate for vision loss and using assistive devices.
3. Lifestyle Adjustments
Patients should avoid activities that could strain the eye, such as lifting heavy objects or engaging in strenuous physical activities for several weeks after surgery. Wearing sunglasses and protective eyewear can also prevent further damage.
1. What is Belt Buckling Vitrectomy Endolaser?
Belt Buckling Vitrectomy Endolaser is a combination of three advanced eye surgery techniques used to treat various retinal conditions, particularly those caused by retinal detachment. This procedure involves:
-
Belt Buckling: A technique where a silicone band is placed around the eye to help reattach the retina to its proper position.
-
Vitrectomy: Removal of the vitreous gel in the eye to allow better access to the retina and to remove any scar tissue.
-
Endolaser: A laser is used inside the eye to seal retinal tears or holes and create scar tissue to help the retina reattach securely.
This procedure is often used in cases of retinal detachment, diabetic retinopathy, or other conditions that affect the retina.
2. What conditions are treated with Belt Buckling Vitrectomy Endolaser?
Belt Buckling Vitrectomy Endolaser is typically used to treat:
-
Retinal Detachment: When the retina separates from the back of the eye, causing vision loss.
-
Retinal Tears or Holes: When the retina is torn, leading to potential detachment.
-
Proliferative Diabetic Retinopathy: A condition caused by abnormal blood vessel growth in the retina, leading to potential retinal detachment.
-
Tractional Retinal Detachment: Often caused by scar tissue pulling on the retina.
This surgery helps in stabilizing the retina and preventing further damage, improving vision in many cases.
3. What are the benefits of Belt Buckling Vitrectomy Endolaser?
The benefits of this combined procedure include:
-
Effective reattachment of the retina: Helps to stabilize the retina and restore its normal position.
-
Improved vision: Many patients experience improved or restored vision following successful treatment.
-
Minimally invasive: The procedure uses small incisions, reducing recovery time compared to traditional surgery.
-
Prevents further complications: The procedure helps to prevent further retinal damage or vision loss in cases of retinal tears or detachment.
4. How is Belt Buckling Vitrectomy Endolaser performed?
The procedure is performed under local or general anesthesia, depending on the patient’s needs. The surgeon makes small incisions in the eye to access the vitreous and retina. The steps typically include:
-
Belt Buckling: A silicone band is placed around the eye to provide external support and help reposition the retina.
-
Vitrectomy: The vitreous gel is removed to provide better access to the retina and to clear any abnormal growths or scar tissue.
-
Endolaser: A laser is used to treat retinal tears, holes, or other issues within the retina to help reattach it and prevent further detachment.
The surgery typically takes one to two hours, depending on the complexity of the case.
5. What are the risks and complications of this surgery?
While the procedure is generally safe, some risks and complications may include:
-
Infection: As with any surgery, there is a risk of infection.
-
Glaucoma: Increased eye pressure could occur after surgery.
-
Cataracts: In some cases, cataracts may develop after vitrectomy.
-
Retinal Re-detachment: There is a possibility that the retina may detach again, requiring further surgery.
-
Vision problems: Some patients may experience blurry vision or reduced visual acuity after surgery, although this often improves over time.
It's essential to follow post-surgery care instructions to minimize these risks.
6. What is the recovery time for Belt Buckling Vitrectomy Endolaser?
Recovery time varies from patient to patient, but most individuals experience:
-
Initial recovery: You may need to rest for the first few days, avoiding strenuous activities.
-
Follow-up visits: Regular follow-up appointments are necessary to monitor healing and retinal reattachment.
-
Vision recovery: Vision improvement can take weeks to months, depending on the extent of the retinal damage before surgery.
-
Activity restrictions: Patients are usually advised to avoid activities that put pressure on the eye, such as heavy lifting or vigorous exercise, for at least a few weeks.
7. Are there any alternatives to Belt Buckling Vitrectomy Endolaser?
Yes, there are other treatments for retinal detachment or retinal tears, including:
-
Pneumatic Retinopexy: A procedure where a gas bubble is injected into the eye to help reattach the retina.
-
Scleral Buckling: A procedure similar to belt buckling, where a silicone band is placed around the eye but without the vitrectomy or endolaser.
-
Laser Photocoagulation: A laser used to treat retinal tears without the need for vitrectomy.
Each treatment option depends on the severity and location of the retinal issue, and a surgeon will determine the best course of action.
8. Can Belt Buckling Vitrectomy Endolaser help restore lost vision?
In many cases, Belt Buckling Vitrectomy Endolaser can help restore or stabilize vision, especially if the retina has been successfully reattached. However, if the retina has been damaged for a long time or if there is extensive scar tissue, full vision recovery may not be possible. The goal of the surgery is to prevent further vision loss, alleviate symptoms, and improve visual function.
9. How long will the results last after surgery?
The results of Belt Buckling Vitrectomy Endolaser are typically long-lasting, especially if the retinal detachment or tear is successfully treated. However, some patients may require additional surgery in the future if complications arise, such as re-detachment or cataracts. It’s important to have regular eye checkups to monitor the health of the retina and vision.
10. Who is a good candidate for Belt Buckling Vitrectomy Endolaser?
Candidates for Belt Buckling Vitrectomy Endolaser typically have retinal conditions such as retinal detachment, retinal tears, or proliferative diabetic retinopathy. A good candidate generally:
-
Has a retinal tear or detachment that cannot be managed with less invasive procedures.
-
Is in generally good health and able to undergo surgery.
-
Has not experienced irreversible vision loss due to the retinal condition.
A retinal specialist will assess the patient’s specific situation and determine if this combined surgical approach is the most appropriate treatment option.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.