Cataract and glaucoma are two of the most prevalent eye conditions that can lead to significant vision impairment or blindness if left untreated. These two diseases are major causes of visual disability worldwide, affecting millions of people, especially as they age. While cataract and glaucoma are both eye conditions that can affect a person's vision, they are fundamentally different diseases in terms of their causes, progression, and treatment options.
Cataract:
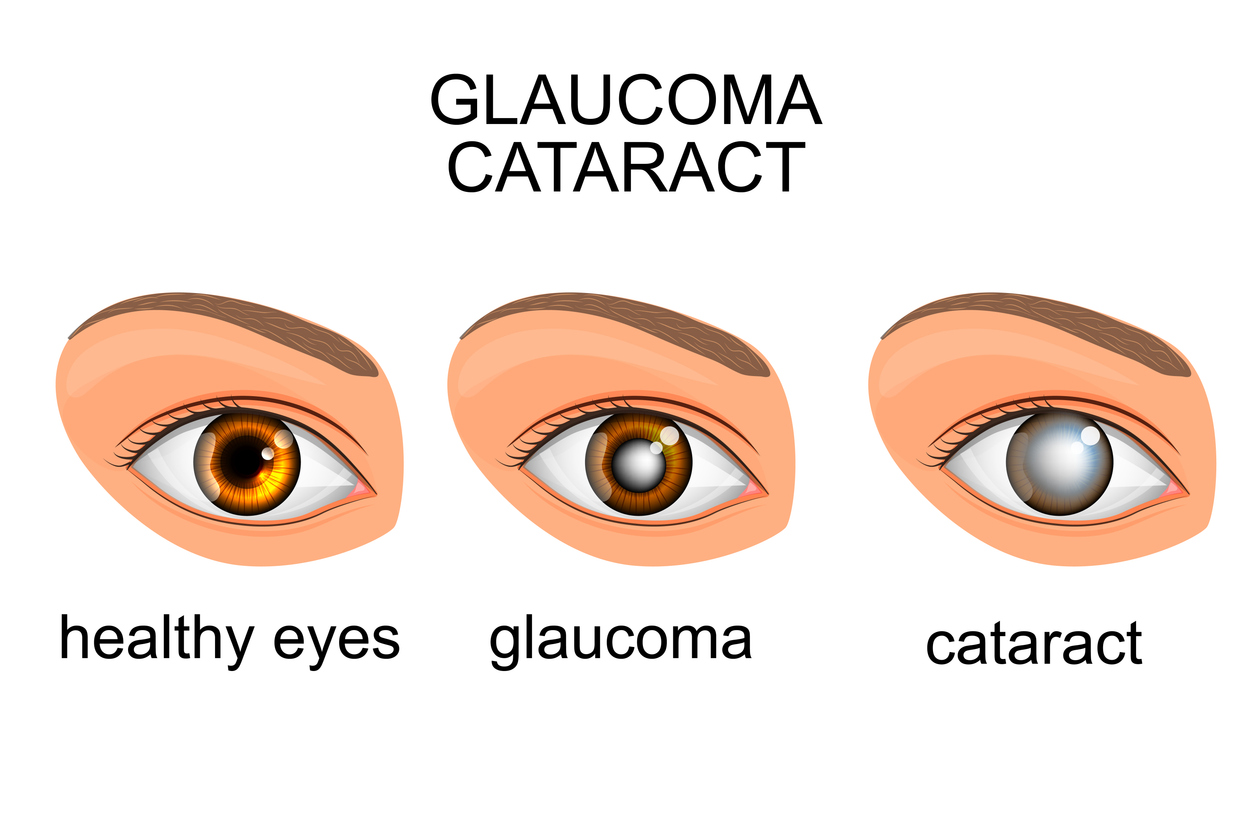
A cataract is the clouding of the lens inside the eye, which obstructs the passage of light and causes blurred or dimmed vision. The lens is responsible for focusing light onto the retina, where the image is processed and transmitted to the brain. When the lens becomes cloudy, it disrupts this process and leads to visual disturbances. Cataracts are most commonly associated with aging, although they can also result from trauma, certain medical conditions, or the use of certain medications.
Cataracts develop gradually over time, and the condition usually affects both eyes, although they may not progress at the same rate. Cataracts are one of the leading causes of reversible blindness, and surgical removal of the cataract is the most effective treatment to restore vision. The procedure, known as cataract surgery, involves removing the cloudy lens and replacing it with a synthetic intraocular lens (IOL) to restore vision.
Glaucoma:
On the other hand, glaucoma refers to a group of diseases that damage the optic nerve, which is essential for transmitting visual information from the retina to the brain. The primary cause of this damage is usually elevated intraocular pressure (IOP), which can cause the optic nerve fibers to deteriorate. The most common form of glaucoma, primary open-angle glaucoma, develops gradually and silently, often without symptoms in the early stages. By the time symptoms become noticeable, significant damage to the optic nerve may have already occurred.
Glaucoma is the second leading cause of blindness worldwide, and once the optic nerve is damaged, the vision loss is typically permanent. Regular eye examinations are crucial for detecting glaucoma early, as timely treatment can prevent further damage to the optic nerve and preserve vision.
While cataract surgery is highly effective in restoring vision, glaucoma management requires ongoing treatment, often through medications or surgery, to control IOP and prevent further nerve damage.
Causes and Risk Factors of Cataract
Cataracts develop when the proteins within the lens of the eye begin to break down and aggregate, leading to clouding. While aging is the most common cause of cataracts, several other factors can contribute to their development:
1. Age:
As individuals age, the proteins in the lens naturally begin to break down and form clumps, leading to cataract formation. By the time people reach their 60s and 70s, many will develop cataracts to some degree. Cataracts are considered a natural part of the aging process, and nearly everyone will experience some form of cataract if they live long enough.
2. Genetics:
A family history of cataracts can increase the likelihood of developing cataracts at an earlier age. In some cases, genetic mutations can lead to congenital cataracts that are present at birth or develop in childhood.
3. Diabetes:
People with diabetes are more likely to develop cataracts, and often at a younger age. High blood sugar levels can affect the lens of the eye, causing it to become cloudy over time. Cataracts in diabetic patients may also progress more rapidly.
4. Smoking:
Smoking accelerates the formation of cataracts, as the chemicals in cigarettes contribute to oxidative stress in the eye. Studies have shown that smokers have a higher risk of developing cataracts compared to non-smokers, and smoking may cause cataracts to develop at a younger age.
5. UV Light Exposure:
Long-term exposure to ultraviolet (UV) rays from the sun or artificial sources can damage the lens of the eye and increase the risk of cataract development. UV radiation can cause oxidative damage to the eye tissues, leading to cataracts over time.
6. Medications:
Some medications, particularly corticosteroids, can increase the risk of cataract formation. Long-term use of steroid medications, whether in the form of pills or eye drops, can lead to the development of cataracts as a side effect.
7. Eye Injuries:
Trauma to the eye, including blunt force trauma or penetrating injuries, can lead to cataracts. Even if the trauma is not severe, it can cause the lens to become clouded and impair vision. Cataracts caused by trauma may develop immediately or years later.
Glaucoma is a group of diseases that cause damage to the optic nerve, typically due to increased intraocular pressure (IOP). While the exact cause of glaucoma is not always clear, several factors contribute to the development of the disease:
1. Increased Intraocular Pressure (IOP):
The most common risk factor for glaucoma is elevated intraocular pressure. IOP is determined by the balance between the production and drainage of aqueous humor (the fluid inside the eye). When the drainage system becomes blocked or inefficient, fluid builds up, increasing the pressure in the eye. High IOP puts pressure on the optic nerve, leading to nerve damage over time.
2. Age:
Glaucoma is more common in people over the age of 60, and the risk increases with age. Even though glaucoma can develop at any age, it typically manifests in older adults.
3. Family History:
Having a family history of glaucoma significantly increases the risk of developing the condition. Genetics play a major role in the development of glaucoma, and those with close relatives who have the disease are more likely to develop it themselves.
4. Ethnicity:
Certain ethnic groups are at higher risk for glaucoma. African Americans are more likely to develop primary open-angle glaucoma at an earlier age and with more severe outcomes. Asians are more susceptible to developing angle-closure glaucoma, which is another type of glaucoma caused by a narrowing or blockage of the drainage angle.
5. High Blood Pressure and Diabetes:
Chronic conditions such as hypertension (high blood pressure) and diabetes can increase the risk of glaucoma. These conditions can damage the blood vessels that supply the optic nerve, contributing to nerve damage.
6. Eye Injuries:
Trauma to the eye can increase the risk of glaucoma. Injuries may cause changes in the drainage system or the anatomy of the eye, leading to increased IOP. Surgical procedures involving the eye can also elevate the risk of developing glaucoma.
7. Prolonged Use of Steroids:
Long-term use of steroidal medications, particularly corticosteroids, can increase the risk of developing secondary glaucoma. These medications can interfere with the eye's ability to drain fluid properly, leading to increased IOP.
Symptoms of Cataracts
The symptoms of cataracts can be subtle at first but typically worsen over time. Common symptoms include:
-
Blurred Vision: The primary symptom of cataracts is blurry or cloudy vision. As the cataract progresses, it may become more difficult to see clearly, particularly in low-light conditions.
-
Glare and Halos: People with cataracts often report increased sensitivity to light, as well as seeing halos around lights, especially at night when driving. This occurs due to the scattering of light by the cloudy lens.
-
Difficulty Seeing at Night: Cataracts can make it harder to see at night or in low-light conditions, a condition known as nyctalopia.
-
Fading or Yellowing of Colors: Cataracts can cause colors to appear dimmer or yellowed, making it difficult to differentiate between hues.
-
Double Vision: Some people with cataracts may experience double vision in one eye. This occurs when the cataract causes light to scatter before it reaches the retina, leading to visual distortions.
-
Frequent Changes in Eyeglass Prescription: Cataracts can lead to frequent changes in the need for glasses. People may find that their glasses prescription becomes less effective over time.
Symptoms of Glaucoma
Glaucoma is often referred to as the silent thief of sight because it develops gradually without noticeable symptoms until significant vision loss occurs. Common symptoms of advanced glaucoma include:
-
Loss of Peripheral Vision: The early stages of glaucoma often involve the gradual loss of side (peripheral) vision. Patients may not notice this loss until it becomes significant.
-
Tunnel Vision: As glaucoma progresses, it may cause a reduction in peripheral vision, leading to the development of tunnel vision—a condition in which only central vision remains intact.
-
Eye Pain and Redness: Some types of glaucoma, particularly acute angle-closure glaucoma, can cause sudden and severe eye pain, redness, nausea, and vomiting.
-
Blurred Vision: Elevated IOP can cause blurry vision and may also lead to visual disturbances, including seeing halos around lights.
-
Sudden Vision Loss: In severe cases, glaucoma can cause sudden vision loss, especially if the IOP rises rapidly.
-
Headaches and Nausea: Increased eye pressure can lead to headaches, often accompanied by nausea and vomiting, particularly in cases of acute angle-closure glaucoma.
Diagnosis of Cataracts
-
Eye Exam: An eye doctor will perform a comprehensive eye exam to assess the health of the eye and the extent of cataract development.
-
Slit Lamp Examination: A slit lamp microscope is used to examine the lens and the interior of the eye in detail. This helps identify cloudiness or other abnormalities in the lens.
-
Visual Acuity Test: This test measures how clearly a person can see at various distances, helping to determine the impact of cataracts on vision.
-
Retinal Exam: During this test, the doctor examines the retina and the back of the eye to rule out other causes of vision loss, such as macular degeneration or diabetic retinopathy.
Diagnosis of Glaucoma
-
Intraocular Pressure (IOP) Test: The most important test for diagnosing glaucoma is measuring the IOP using tonometry. Elevated IOP is a strong indicator of glaucoma.
-
Optic Nerve Examination: The ophthalmologist will examine the optic nerve for signs of damage, such as cupping, which is a hallmark of glaucoma.
-
Visual Field Test: This test assesses peripheral vision to detect blind spots or other changes that are characteristic of glaucoma.
-
Gonioscopy: This test allows the doctor to examine the drainage angle of the eye to determine the type of glaucoma.
-
Optical Coherence Tomography (OCT): OCT provides detailed images of the optic nerve and retina, helping detect early structural changes associated with glaucoma.
Treatment of Cataracts
-
Surgical Removal: Cataract surgery is the most effective and common treatment. The surgeon removes the cloudy lens and replaces it with an artificial intraocular lens (IOL).
-
Lens Implants: There are different types of IOLs, including monofocal, multifocal, and toric lenses, depending on the patient's needs.
Treatment of Glaucoma
-
Medications: The first-line treatment for glaucoma is eye drops or oral medications to reduce IOP. These include:
-
Prostaglandin analogs
-
Beta-blockers
-
Alpha agonists
-
Carbonic anhydrase inhibitors
-
-
Laser Therapy: Laser treatments, such as laser trabeculoplasty for open-angle glaucoma and laser iridotomy for angle-closure glaucoma, can improve fluid drainage and reduce IOP.
-
Surgical Procedures: In advanced cases, surgery may be required, including trabeculectomy and tube shunt surgery, to create a new drainage pathway for aqueous humor.
Prevention of Cataracts and Glaucoma
-
Regular Eye Exams: Regular check-ups with an eye care professional can help detect both conditions early, even in the absence of symptoms.
-
Protecting Eyes from UV Light: Wearing sunglasses with UV protection can help prevent cataracts caused by UV exposure.
-
Healthy Lifestyle: Eating a diet rich in antioxidants, managing diabetes, quitting smoking, and avoiding excessive alcohol consumption can help reduce the risk of cataracts and glaucoma.
Management of Cataracts and Glaucoma
-
Post-Surgical Care: After cataract surgery, proper post-operative care, including eye drops and avoiding heavy lifting, is essential to ensure recovery.
-
Glaucoma Medication Adherence: Patients with glaucoma must adhere to a strict medication regimen to control IOP and prevent vision loss.
Cataract Complications
-
Vision Loss: Untreated cataracts can lead to permanent vision loss.
-
Glare and Poor Night Vision: Even after surgery, some people may experience residual glare or halos around lights.
Glaucoma Complications
-
Permanent Vision Loss: If left untreated, glaucoma can lead to irreversible blindness.
-
Medication Side Effects: Some glaucoma medications can cause side effects like dry eyes, stinging, or systemic effects like low blood pressure.
Living with cataracts and glaucoma requires ongoing care and adaptations:
-
Cataract Surgery Recovery: Most people experience significant improvement in vision after cataract surgery. However, recovery can take a few weeks, during which the patient must follow the doctor's instructions carefully.
-
Glaucoma Management: Patients must commit to a lifelong treatment plan that includes medication, regular monitoring, and sometimes surgery to prevent vision loss.
1. What are cataracts?
A cataract is a clouding of the eye's natural lens, which is located behind the iris and the pupil. This clouding causes blurred or distorted vision and can eventually lead to complete vision loss if left untreated. Cataracts often develop slowly over time, and the condition is most commonly associated with aging, but it can also result from other factors such as injury, genetics, or certain medical conditions like diabetes.
2. What is glaucoma?
Glaucoma refers to a group of eye diseases that damage the optic nerve, which is crucial for vision. It is often caused by high intraocular pressure (IOP) inside the eye. If left untreated, glaucoma can lead to permanent vision loss. There are different types of glaucoma, with open-angle glaucoma and angle-closure glaucoma being the most common. Both types affect the drainage of fluid in the eye, leading to increased pressure and nerve damage.
3. What causes cataracts?
Cataracts are primarily caused by aging, as the proteins in the lens of the eye naturally break down over time, leading to cloudiness. However, other factors that can contribute to cataract formation include:
-
Genetics: Family history of cataracts increases the risk.
-
Injury to the eye: Trauma can lead to cataracts forming.
-
Health conditions: Diabetes, high blood pressure, and obesity can contribute to cataracts.
-
Medication use: Long-term use of corticosteroids has been linked to cataract formation.
-
Excessive UV exposure: Spending too much time in direct sunlight without eye protection can increase the risk.
4. What causes glaucoma?
The exact cause of glaucoma is not fully understood, but it is generally associated with increased intraocular pressure (IOP), which damages the optic nerve. Factors that contribute to glaucoma include:
-
High eye pressure: Caused by a build-up of fluid inside the eye that does not drain properly.
-
Age: People over the age of 60 are at higher risk, though it can occur at any age.
-
Family history: A family history of glaucoma increases the risk.
-
Race: African Americans and Hispanics are more likely to develop glaucoma at a younger age.
-
Medical conditions: Conditions like diabetes and high blood pressure may contribute to glaucoma development.
5. What are the symptoms of cataracts?
The symptoms of cataracts may include:
-
Blurry vision or double vision in one eye
-
Faded or yellowed colors
-
Glare: Difficulty seeing in bright light or headlights at night
-
Frequent prescription changes for glasses or contact lenses
-
Halos around lights
-
Difficulty seeing at night due to reduced night vision
Since cataracts develop gradually, many people may not notice symptoms until the condition is more advanced.
6. What are the symptoms of glaucoma?
The symptoms of glaucoma can vary depending on the type. Open-angle glaucoma often has no noticeable symptoms until significant damage has occurred. However, common signs include:
-
Gradual loss of peripheral vision (often unnoticed initially)
-
Blurred vision
-
Severe eye pain (more common in acute angle-closure glaucoma)
-
Redness in the eye
-
Halos around lights
-
Nausea and vomiting (associated with acute glaucoma)
7. How are cataracts treated?
The primary treatment for cataracts is surgery, in which the clouded lens is removed and replaced with a clear artificial lens (intraocular lens or IOL). Cataract surgery is typically a quick, minimally invasive procedure with a high success rate, and most patients experience improved vision after recovery. If cataracts are diagnosed early, corrective lenses (glasses or contacts) can be used to manage symptoms, but surgery is the only definitive treatment.
8. How is glaucoma treated?
Glaucoma treatment focuses on reducing intraocular pressure to prevent further damage to the optic nerve. Common treatment options include:
-
Eye drops: These reduce the fluid production in the eye or help the fluid drain more efficiently.
-
Oral medications: In some cases, oral medications are prescribed to lower eye pressure.
-
Laser therapy: Used to improve the drainage of fluid within the eye (laser trabeculoplasty).
-
Surgery: For advanced cases, surgery may be performed to create a new drainage channel or to implant a device to reduce pressure.
Regular monitoring of eye pressure and vision is important to manage glaucoma over time.
9. Can cataracts and glaucoma occur together?
Yes, cataracts and glaucoma can occur together, particularly in older adults. In fact, the presence of glaucoma can complicate cataract surgery. Glaucoma treatment needs to be considered before, during, and after cataract surgery to ensure that intraocular pressure is well-controlled. If glaucoma is not properly managed before cataract surgery, it can lead to further vision loss. Eye doctors carefully assess both conditions to create a treatment plan that addresses both cataracts and glaucoma.
10. What is the prognosis for cataracts and glaucoma?
-
Cataracts: With proper treatment, typically through surgery, the prognosis for cataracts is excellent, and most people experience significant improvement in their vision. Surgery has a very high success rate, with minimal complications.
-
Glaucoma: The prognosis for glaucoma depends on how early it is detected and how well it is managed. If glaucoma is caught early, treatment can help control the condition and prevent further vision loss. However, once damage to the optic nerve occurs, it cannot be reversed. Ongoing treatment and regular monitoring are essential for preserving vision.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


