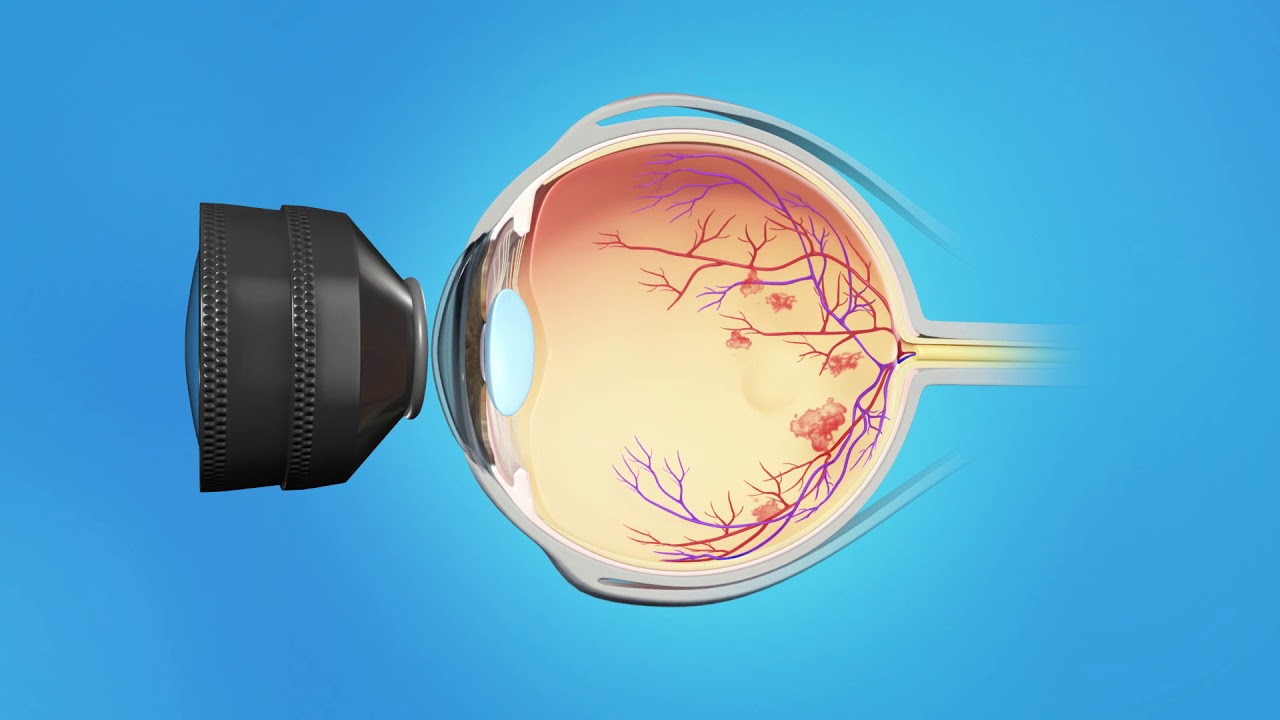
Central Retinal Vein Occlusion (CRVO) is a serious and potentially sight-threatening eye condition that occurs when the central retinal vein becomes blocked or occluded. The central retinal vein is responsible for draining deoxygenated blood from the retina, the light-sensitive layer of tissue at the back of the eye. When this vein becomes blocked, blood flow to the retina is impaired, leading to retinal hemorrhages, fluid accumulation, and in some cases, significant damage to the retina. CRVO is one of the leading causes of vision loss among adults, particularly those over the age of 50.
CRVO can be classified into two types: non-ischemic and ischemic. Non-ischemic CRVO, also known as the "better" form, involves less severe retinal damage and usually carries a better prognosis. Ischemic CRVO, however, results in reduced blood flow to the retina and is associated with more severe vision loss.
Timely intervention and management of CRVO are essential in preventing further complications, such as macular edema, neovascularization, and glaucoma. With appropriate treatment, many individuals can recover some degree of vision or prevent further vision deterioration.
The exact cause of CRVO is not always clear, but it is primarily associated with several underlying factors that affect blood flow in the eye. The most common cause of CRVO is retinal vein thrombosis—the formation of a blood clot in the retinal vein, which can block or reduce blood flow. Below are the main causes and risk factors associated with this condition:
1. Age
As individuals age, the risk of CRVO increases significantly. The condition is more common in those over 50 and becomes even more prevalent in individuals aged 70 and older.
2. Hypertension (High Blood Pressure)
One of the most significant risk factors for CRVO is hypertension. High blood pressure causes increased pressure in the blood vessels, which can lead to the narrowing and thickening of the retinal veins, making them more prone to occlusion.
3. Atherosclerosis (Hardening of the Arteries)
Atherosclerosis, which is the buildup of plaque inside the arteries, is another contributing factor. This condition affects the circulation throughout the body, including the eye, and may increase the risk of blood clot formation in the retinal vein.
4. Diabetes
Individuals with diabetes, particularly those with poorly controlled blood sugar levels, are at a significantly increased risk of CRVO. Diabetic retinopathy, a condition caused by damage to the blood vessels of the retina, can also predispose individuals to retinal vein occlusion.
5. Glaucoma
Glaucoma and other optic nerve diseases are associated with CRVO. These conditions can cause elevated pressure in the eye, which may contribute to the blockage of the retinal vein.
6. Blood Clotting Disorders
Certain blood clotting disorders, such as antiphospholipid syndrome and factor V Leiden, increase the risk of blood clots. These disorders can lead to the formation of clots in the retinal veins, resulting in CRVO.
7. Smoking
Smoking is a well-known risk factor for various cardiovascular diseases, and it can also increase the risk of retinal vein occlusion. Smoking accelerates the process of atherosclerosis and impairs circulation, including in the eye.
8. Hyperlipidemia (High Cholesterol)
High cholesterol levels can contribute to the narrowing and thickening of the blood vessels, making them more susceptible to blockage. This increases the likelihood of developing retinal vein occlusion.
9. Sleep Apnea
Obstructive sleep apnea (OSA), a condition characterized by intermittent cessation of breathing during sleep, is associated with an increased risk of CRVO. Sleep apnea leads to fluctuations in blood oxygen levels and can contribute to the development of retinal vein thrombosis.
10. Other Risk Factors
Other risk factors for CRVO include obesity, sedentary lifestyle, and oral contraceptive use (especially in women over the age of 35 who smoke). Additionally, pregnancy and postpartum status have been linked to an increased risk of CRVO in some cases.
CRVO can be asymptomatic in its early stages, particularly in the non-ischemic form, and may only be detected during an eye examination. However, as the condition progresses, several symptoms and signs may become apparent. These can vary depending on the severity of the blockage and whether the condition is ischemic or non-ischemic.
1. Sudden Vision Loss
One of the most noticeable symptoms of CRVO is sudden, painless vision loss. This vision loss can occur in one or both eyes and can range from mild to severe, depending on the degree of retinal damage. In some cases, vision may blur or become distorted.
2. Blurred or Cloudy Vision
Patients with CRVO may experience blurred vision in one eye due to swelling and fluid accumulation in the retina (particularly the macula, the central part of the retina responsible for sharp, detailed vision). This is a common symptom, especially in the presence of macular edema.
3. Distorted Vision
Another common sign is distorted vision, where straight lines appear wavy or bent. This is due to the swelling and changes in the retina that occur with CRVO, affecting the macula’s function.
4. Visual Field Defects
Patients with CRVO may experience visual field defects, such as the loss of peripheral vision or the appearance of blind spots. This is especially common in ischemic CRVO, where severe damage to the retinal tissue occurs.
5. Floaters
Some individuals with CRVO may notice floaters—small specks, cobwebs, or threads that float in the field of vision. These can be caused by the leakage of blood or fluid into the vitreous humor, the gel-like substance in the eye.
6. Eye Redness
In some cases, patients may experience eye redness due to bleeding in the retina, which can cause the eye's blood vessels to become congested.
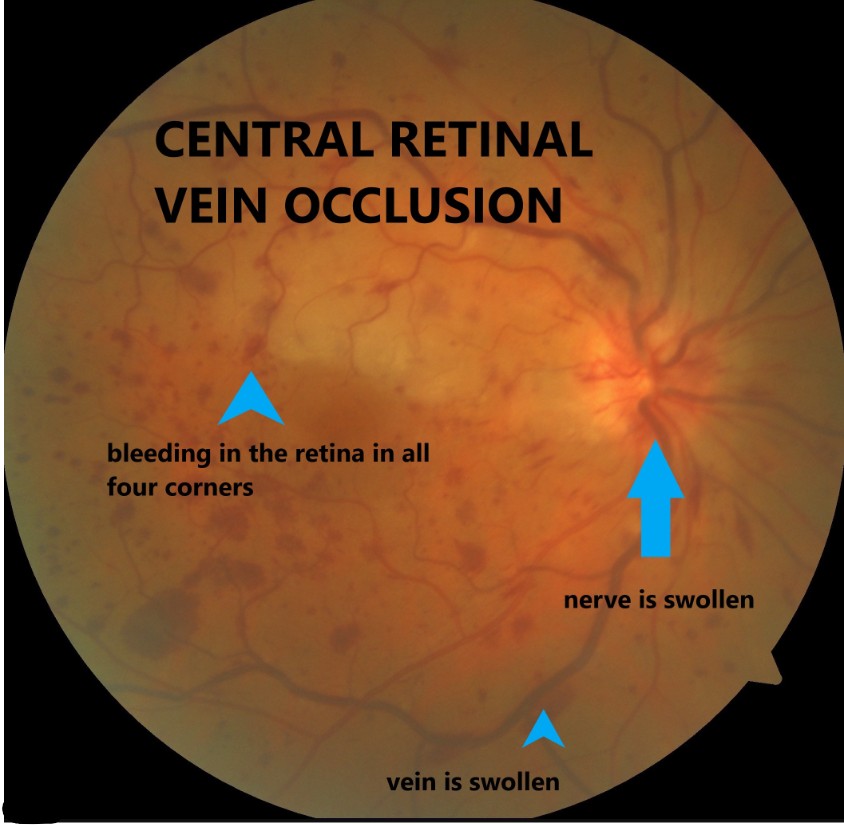
The diagnosis of CRVO involves a thorough eye examination and a combination of tests to assess the severity and extent of the condition. The following diagnostic techniques are commonly used:
1. Comprehensive Eye Exam
An eye care professional will conduct a comprehensive eye exam, which includes assessing visual acuity (sharpness of vision), examining the retina with an ophthalmoscope, and evaluating the optic nerve for any signs of damage.
2. Fluorescein Angiography
Fluorescein angiography is a procedure in which a fluorescent dye is injected into the bloodstream, and photographs of the retina are taken as the dye circulates through the retinal blood vessels. This test helps identify areas of retinal ischemia (lack of blood flow), hemorrhages, and leaks.
3. Optical Coherence Tomography (OCT)
OCT provides cross-sectional images of the retina, allowing the ophthalmologist to assess the thickness of the retina and detect any swelling or fluid accumulation, particularly in the macula. OCT can also help monitor the progression of the condition and the response to treatment.
4. Visual Field Test
A visual field test is used to detect any blind spots or defects in the field of vision. This test can help assess the extent of vision loss caused by CRVO.
5. Retinal Imaging
Advanced retinal imaging techniques, such as fundus photography, can provide detailed images of the retina and help identify any retinal hemorrhages, swelling, or changes in the retinal blood vessels associated with CRVO.
Treatment for CRVO depends on the type and severity of the occlusion, as well as the presence of associated complications such as macular edema or neovascularization. The goal of treatment is to reduce swelling, control intraocular pressure (IOP), and prevent further damage to the retina.
1. Medications
-
Anti-VEGF Injections: Anti-vascular endothelial growth factor (VEGF) injections are commonly used to treat macular edema resulting from CRVO. These medications, such as ranibizumab (Lucentis) or aflibercept (Eylea), inhibit the growth of abnormal blood vessels and reduce fluid leakage in the retina.
-
Corticosteroids: Steroid injections or implants (such as dexamethasone implants) can help reduce inflammation and swelling in the retina, particularly when macular edema is present.
-
Oral Medications: In some cases, oral medications to manage underlying conditions like hypertension or diabetes are necessary to control the risk factors contributing to CRVO.
2. Laser Treatment
-
Laser Photocoagulation: In cases of ischemic CRVO or when neovascularization occurs, laser photocoagulation may be used to target the abnormal blood vessels and prevent further complications such as neovascular glaucoma.
3. Surgery
-
Vitrectomy: In severe cases of CRVO, particularly when the condition is accompanied by retinal hemorrhages or vitreous hemorrhage, a vitrectomy may be performed. This surgical procedure involves removing the vitreous humor and any blood or debris from the eye to improve visual clarity and prevent retinal damage.
4. Monitoring and Follow-Up Care
Patients with CRVO require regular follow-up appointments to monitor the effectiveness of treatment and to track any changes in retinal health. Continuous monitoring is essential for detecting complications such as neovascularization or glaucoma, which can occur after CRVO.
While it is not always possible to prevent CRVO, there are steps individuals can take to reduce the risk of developing the condition and to manage it effectively:
1. Managing Underlying Health Conditions
-
Controlling hypertension and diabetes is crucial in preventing CRVO. Proper management of these conditions can reduce the likelihood of retinal vein occlusion.
-
Cholesterol and triglyceride management through a healthy diet, exercise, and medications can help lower the risk of vascular problems in the eye.
2. Lifestyle Modifications
-
Quitting smoking and maintaining a healthy weight can reduce the risk of developing atherosclerosis and vascular problems that contribute to CRVO.
3. Regular Eye Exams
-
Routine eye exams with an eye care professional are essential for detecting early signs of CRVO or other eye conditions that could affect vision. Early diagnosis allows for timely treatment and intervention to prevent further vision loss.
If left untreated or not adequately managed, CRVO can lead to several serious complications, including:
-
Macular Edema: Swelling of the macula, which is the central part of the retina, is one of the most common complications of CRVO and can cause significant vision loss.
-
Neovascularization: The formation of abnormal blood vessels in the retina, which can lead to further complications such as neovascular glaucoma.
-
Glaucoma: In some cases, neovascular glaucoma can develop as a result of abnormal blood vessel growth in the eye, leading to increased IOP and further optic nerve damage.
-
Vitreous Hemorrhage: Bleeding into the vitreous humor can occur due to retinal neovascularization and can result in vision impairment.
Living with CRVO requires ongoing management and care to prevent vision loss and manage complications. Patients need to adhere to treatment regimens, including medications, regular eye exams, and possibly surgical interventions.
1. Visual Rehabilitation
-
For patients experiencing vision loss due to CRVO, low vision rehabilitation can help them adapt to their visual changes. This includes using assistive devices, such as magnifiers, and learning new techniques to perform daily activities.
2. Emotional and Psychological Support
-
Vision loss can be emotionally challenging. Patients may benefit from psychological counseling and support groups to help cope with the emotional impact of the disease.
3. Ongoing Monitoring
-
Patients must attend regular follow-up visits with their ophthalmologist to monitor the condition’s progression and the effectiveness of treatment. This includes assessing the retina, checking for complications, and adjusting treatment plans as necessary.
1. What is Central Retinal Vein Occlusion (CRVO)?
Answer:
Central Retinal Vein Occlusion (CRVO) is a condition in which the main vein that drains
blood
from the retina, the central retinal vein, becomes blocked. This blockage can lead to a
buildup
of fluid in the retina, causing swelling (edema) and damage to the retinal tissue. CRVO can
result in sudden vision loss in one eye and is a serious condition that requires prompt
attention and treatment.
2. What causes Central Retinal Vein Occlusion (CRVO)?
Answer:
CRVO is often caused by a blockage in the central retinal vein, usually due to a clot or
narrowing of the vein. The main risk factors for CRVO include:
-
High blood pressure (hypertension)
-
Diabetes
-
Atherosclerosis (hardening of the arteries)
-
Glaucoma
-
Age: CRVO is more common in individuals over the age of 60.
-
Blood clotting disorders: Conditions that increase blood clotting may raise the risk.
-
Smoking and obesity can also contribute to the development of CRVO.
3. What are the symptoms of Central Retinal Vein Occlusion (CRVO)?
Answer:
The symptoms of CRVO can vary depending on the severity of the blockage. Common symptoms
include:
-
Sudden, painless vision loss in one eye
-
Blurry vision
-
Distorted vision
-
Swelling in the retina (which may be detected during an eye exam)
-
Visual disturbances like seeing a dark spot in the center of vision
If left untreated, CRVO can lead to permanent vision loss.
4. How is Central Retinal Vein Occlusion diagnosed?
Answer:
CRVO is diagnosed through a comprehensive eye exam, which includes:
-
Fundus exam: The doctor will look inside the eye using a special light to examine the retina and identify any signs of swelling or hemorrhages.
-
Optical coherence tomography (OCT): This imaging test provides cross-sectional images of the retina to detect fluid accumulation and swelling.
-
Fluorescein angiography: A dye is injected into the bloodstream, and special photos are taken of the retina to assess blood flow and the extent of the blockage.
-
Visual field test: This test checks the peripheral vision to determine the degree of vision loss.
5. What are the treatment options for Central Retinal Vein Occlusion (CRVO)?
Answer:
The treatment for CRVO depends on the severity of the condition and the presence of
complications such as macular edema. Treatment options include:
-
Anti-VEGF injections: Medications like Avastin, Lucentis, or Eylea are injected into the eye to reduce swelling and improve vision.
-
Steroid injections: Steroids can help reduce inflammation in the retina.
-
Laser therapy: Laser treatment may be used to treat areas of the retina that are affected by swelling or ischemia (lack of blood flow).
-
Management of underlying conditions: Controlling risk factors such as high blood pressure or diabetes is critical in managing CRVO.
6. What are the complications of Central Retinal Vein Occlusion (CRVO)?
Answer:
Complications of CRVO can be severe if the condition is not treated or managed
appropriately.
These may include:
-
Macular edema: Swelling in the central part of the retina (the macula), which is the area responsible for sharp, central vision.
-
Neovascularization: Abnormal blood vessel growth on the retina, which can lead to further vision problems and may cause bleeding in the eye.
-
Glaucoma: Elevated intraocular pressure due to abnormal blood vessel growth or other factors.
-
Permanent vision loss: If the condition is not treated in time, CRVO can lead to permanent vision impairment or blindness.
7. What is the prognosis for someone with Central Retinal Vein Occlusion (CRVO)?
Answer:
The prognosis for CRVO depends on several factors, including the severity of the blockage,
the
presence of macular edema, and how quickly treatment is initiated. Some individuals may
experience partial or complete recovery of vision, especially with early and effective
treatment. However, in some cases, CRVO can lead to permanent vision loss, especially if
complications like macular edema or neovascularization occur. Regular monitoring and
management
of underlying health conditions can improve the outlook for many patients.
8. Can Central Retinal Vein Occlusion (CRVO) be prevented?
Answer:
While CRVO cannot always be prevented, certain steps can reduce the risk of developing the
condition:
-
Manage underlying health conditions: Keeping blood pressure and blood sugar levels under control can reduce the risk of CRVO.
-
Maintain a healthy lifestyle: This includes eating a balanced diet, exercising regularly, and quitting smoking.
-
Regular eye exams: Early detection and monitoring of any eye health issues can help catch CRVO or other eye conditions before they cause significant damage.
9. Is Central Retinal Vein Occlusion (CRVO) a lifelong condition?
Answer:
CRVO can be a lifelong condition, but with prompt and effective treatment, many people can
manage the condition and prevent further vision loss. Some individuals may experience
long-term
visual impairment, while others may regain much of their vision, particularly if macular
edema
is treated early. Regular follow-up visits with an ophthalmologist are essential to manage
the
condition and address any changes in vision over time.
10. What is the long-term care for someone with Central Retinal Vein Occlusion (CRVO)?
Answer:
Long-term care for someone with CRVO involves:
-
Regular monitoring: Ongoing eye exams and imaging to track changes in the retina and vision.
-
Management of underlying health conditions: Controlling risk factors such as hypertension, diabetes, and cholesterol.
-
Monitoring for complications: Keeping an eye on possible complications like macular edema, glaucoma, or neovascularization.
-
Vision rehabilitation: If there is lasting vision loss, patients may benefit from vision rehabilitation programs to improve quality of life and adapt to changes in vision.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.