Childhood Visual Pathway Glioma (VP Glioma) is a rare, but significant, form of brain tumor that affects the visual pathway, which includes the optic nerves, optic chiasm, and the associated optic tracts. These tumors grow in the brain’s region responsible for transmitting visual information from the eyes to the brain. Visual pathway gliomas are a subtype of gliomas, which are tumors that arise from glial cells—supportive cells in the nervous system.
VP gliomas most commonly occur in children, particularly those under the age of 10. They are often associated with neurofibromatosis type 1 (NF1), a genetic disorder that predisposes individuals to a variety of tumors, including gliomas. In fact, visual pathway gliomas are considered one of the hallmark features of NF1.
These tumors can cause a variety of symptoms, ranging from visual disturbances to more severe complications if left untreated. The severity of the tumor depends on the location, size, and growth pattern of the glioma, as well as the age of the child when diagnosed. Early detection and treatment are crucial to improving outcomes and preventing long-term vision loss or other complications.
Causes of Childhood Visual Pathway Glioma
The exact cause of childhood visual pathway gliomas remains unclear, though genetic mutations and abnormal cellular growth are believed to play a major role. Visual pathway gliomas are typically primary tumors, meaning they originate in the glial cells of the brain rather than spreading from other parts of the body.
The two most significant contributors to the development of visual pathway gliomas are:
-
Neurofibromatosis Type 1 (NF1):
-
NF1 is the leading genetic cause of visual pathway gliomas. It is an autosomal dominant genetic disorder that predisposes individuals to developing various types of benign and malignant tumors, including gliomas. NF1 is caused by mutations in the NF1 gene, which is responsible for producing a protein called neurofibromin that regulates cell growth.
-
Children with NF1 have a significantly higher risk of developing optic nerve gliomas. In fact, around 15-20% of children with NF1 will develop these gliomas, often before the age of 10.
-
-
Sporadic Cases:
-
Sporadic visual pathway gliomas occur without any underlying genetic condition like NF1. These tumors may arise from mutations or abnormal growth of glial cells in the visual pathway. In these cases, the exact cause of the tumor is unknown, and genetic predisposition may not be involved.
-
Risk Factors for Childhood Visual Pathway Glioma
-
Genetics (NF1):
-
NF1 is the most significant risk factor for visual pathway gliomas. As mentioned, children with NF1 are at a much higher risk of developing gliomas in the optic pathway. These tumors are generally diagnosed before the age of 10 in children with NF1.
-
-
Age:
-
Visual pathway gliomas most commonly affect children under the age of 10, with the majority of diagnoses occurring in children between 3 and 8 years old. The age of onset plays a role in the potential severity and treatment approach for the tumor.
-
-
Gender:
-
Some studies suggest a slight male predominance in the occurrence of visual pathway gliomas, although the disease affects both genders.
-
-
Family History:
-
A family history of NF1 or brain tumors can increase the risk of developing childhood visual pathway gliomas, especially in families with a known genetic predisposition to such tumors.
-
-
Other Genetic Conditions:
-
Rare genetic syndromes like Li-Fraumeni syndrome or Turcot syndrome that predispose individuals to various cancers may also increase the risk of gliomas. However, these conditions are much less common compared to NF1.
-
The symptoms of Childhood Visual Pathway Glioma vary depending on the tumor's location, size, and whether it is affecting both optic nerves. The visual pathway is responsible for processing and transmitting visual information, so damage to these structures can lead to significant visual problems. Here are the most common symptoms and signs of VP gliomas:
1. Vision Problems:
-
Loss of Vision: One of the most prominent symptoms of visual pathway glioma is progressive vision loss. The vision loss often begins with the loss of peripheral vision or blurred vision and may advance to complete central vision loss. The visual disturbance may be gradual or sudden, depending on the tumor’s growth.
-
Double Vision (Diplopia): Children with VP gliomas may experience double vision as the tumor presses on the optic nerves or the optic chiasm, interfering with the normal visual processing.
-
Squinting or Head Tilting: To compensate for vision problems, children with visual pathway gliomas may squint or tilt their head. This compensatory behavior can indicate difficulty focusing or seeing objects clearly.
-
Impaired Color Vision: Some children may have difficulty distinguishing colors due to damage to the optic pathways.
2. Eye Abnormalities:
-
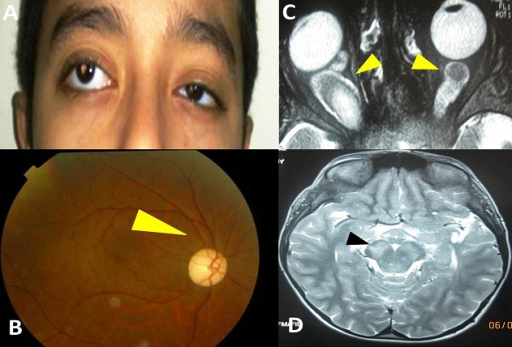
Proptosis (Bulging Eyes): In some cases, the growth of the tumor may cause bulging eyes (proptosis). This occurs when the tumor pushes against the optic nerves or the surrounding tissues, causing pressure and affecting the position of the eyes.
-
Papilledema: Swelling of the optic disc (papilledema) can be seen upon eye examination, particularly in cases where there is increased intracranial pressure due to tumor growth. This swelling is a result of poor circulation and can lead to further visual impairment.
3. Neurological Symptoms:
-
Headaches: Persistent or recurring headaches are a common symptom of visual pathway gliomas. The pressure caused by the tumor growing in the brain can lead to increased intracranial pressure, resulting in headaches, especially in the morning or after physical exertion.
-
Nausea and Vomiting: In cases where the tumor causes significant increased intracranial pressure, children may experience nausea and vomiting.
-
Seizures: Though rare, seizures may occur if the tumor grows and causes irritation or damage to the brain tissue around the optic pathways.
4. Endocrine Symptoms:
-
Growth Delay: In some cases, VP gliomas may involve the pituitary gland, which regulates hormones responsible for growth. Children with VP gliomas may show signs of delayed growth or puberty due to hormonal imbalances caused by pituitary dysfunction.
-
Hormonal Imbalances: The tumor can affect other hormones controlled by the pituitary gland, leading to symptoms such as increased thirst, frequent urination, and weight changes.
Diagnosing Childhood Visual Pathway Glioma involves a combination of clinical examination, imaging studies, and ocular tests to confirm the presence of the tumor, assess its size and location, and evaluate the impact on vision. Here are the steps involved in the diagnostic process:
1. Medical History and Physical Examination:
-
A comprehensive medical history and physical exam are the first steps in diagnosing a visual pathway glioma. This includes a thorough neurological evaluation, an eye exam, and questions about the child's symptoms.
2. Ophthalmic Examination:
-
Fundus Examination: An eye specialist will conduct a fundus exam to check for signs of optic nerve swelling (papilledema) or other abnormalities that might suggest the presence of a glioma.
-
Visual Field Testing: This test assesses peripheral vision and can help detect vision loss or other visual disturbances caused by the tumor.
-
OCT (Optical Coherence Tomography): OCT is a non-invasive imaging test that provides detailed cross-sectional images of the retina and optic nerve. It helps assess the structural changes caused by the tumor.
3. Imaging Studies:
-
MRI (Magnetic Resonance Imaging): The gold standard for diagnosing VP gliomas is MRI. This imaging technique provides highly detailed images of the brain and the visual pathways. MRI is used to confirm the presence of a glioma, assess its size and location, and determine the impact on surrounding structures like the optic nerves.
-
CT Scan (Computed Tomography): While MRI is more commonly used, CT scans may be utilized in certain situations, particularly in emergency cases or when MRI is not available. A CT scan can provide information about the tumor's size, location, and potential calcifications.
4. Genetic Testing and Counseling:
-
For children diagnosed with visual pathway gliomas, particularly those with neurofibromatosis type 1 (NF1), genetic testing is recommended to confirm the diagnosis and assess the risk of other associated tumors or complications.
Treatment of Childhood Visual Pathway Glioma depends on various factors, including the size, location, and type of the tumor, as well as the child’s age and overall health. The goal of treatment is to reduce tumor size, preserve vision, and improve quality of life. Here are the common treatment options for this condition:
1. Observation and Monitoring:
-
In non-progressive cases of VP gliomas, especially if the tumor is small and not causing significant symptoms, watchful waiting or active surveillance may be recommended. Regular MRI scans and eye exams are used to monitor the tumor for any changes or growth.
2. Surgery:
-
Surgical resection may be an option if the tumor is localized and accessible. However, surgery for visual pathway gliomas is complex due to the tumor’s location near critical structures like the optic nerves and chiasm. The goal of surgery is to remove as much of the tumor as possible while preserving vision and avoiding damage to the optic pathways.
3. Radiation Therapy:
-
Radiation therapy is often used to treat gliomas that cannot be surgically removed. It is effective in reducing tumor size and controlling growth. However, radiation can have side effects, including growth hormone deficiencies, cognitive delays, and increased risk of other cancers later in life.
-
Proton beam therapy may be preferred over traditional radiation due to its ability to deliver targeted treatment with less damage to surrounding healthy tissue.
4. Chemotherapy:
-
Chemotherapy is often used for tumors that are inoperable or have recurred after surgery or radiation. Chemotherapy drugs like carboplatin and temozolomide are commonly used to treat childhood gliomas and can help shrink the tumor and slow its growth.
5. Targeted Therapy and Clinical Trials:
-
Targeted therapies, which focus on specific molecules involved in tumor growth, are emerging as a promising treatment for gliomas. Clinical trials are ongoing to evaluate the effectiveness of drugs that target specific pathways involved in glioma growth, such as angiogenesis inhibitors or immunotherapy.
Currently, there is no known way to prevent childhood visual pathway gliomas, especially since they are often caused by genetic mutations (NF1) or occur sporadically. However, early detection, genetic counseling, and regular monitoring are crucial for managing the condition effectively.
1. Regular Follow-ups:
-
Regular MRI scans and eye exams are essential for monitoring the tumor’s growth and detecting changes early. This is particularly important for children with NF1, who are at a higher risk for developing visual pathway gliomas.
2. Genetic Counseling:
-
Families with a history of NF1 should undergo genetic counseling to better understand the risks of developing gliomas and other related tumors. Genetic testing can also help in planning surveillance and treatment strategies.
3. Symptom Management:
-
Managing the visual and neurological symptoms of the glioma is a key aspect of treatment. Children may benefit from vision therapy, rehabilitation, or educational support to cope with any developmental delays or visual impairments.
While many children with visual pathway gliomas respond well to treatment, complications can occur, particularly if the tumor is large or left untreated. Common complications include:
-
Vision Loss: The most significant complication of VP gliomas is permanent vision loss. Tumor growth can damage the optic nerve or retina, leading to vision impairment or blindness.
-
Endocrine Issues: Tumors affecting the pituitary gland can lead to hormonal imbalances, such as growth hormone deficiencies or delayed puberty.
-
Cognitive and Developmental Delays: Radiation therapy, surgery, or tumor growth near critical brain structures can lead to neurodevelopmental delays, including difficulties with learning and memory.
-
Recurrence: VP gliomas can recur even after surgery or radiation, particularly if the tumor was not completely removed.
Living with a childhood visual pathway glioma requires a multi-disciplinary approach to care, including medical, psychological, and emotional support. Regular follow-up exams, including imaging and eye exams, are essential to monitor for recurrence or changes in the tumor. Families should also be aware of the potential long-term effects of treatment, such as cognitive development issues, visual rehabilitation, and the emotional challenges of managing a chronic illness.
Children with visual pathway gliomas may need special education services, adaptive technologies for vision, and therapy to cope with potential developmental delays or changes in behavior. With early diagnosis, appropriate treatment, and ongoing care, many children with visual pathway gliomas can lead fulfilling and productive lives.
1. What is Childhood Visual Pathway Glioma?
Childhood visual pathway glioma (VPG) is a rare type of brain tumor that affects the visual pathway, which includes the optic nerve, optic chiasm, and other structures involved in vision processing. Gliomas are a group of tumors that arise from glial cells (supporting cells in the brain). These tumors are often slow-growing and can cause visual problems due to their location near the optic nerve. VPG primarily affects children and is most commonly associated with neurofibromatosis type 1 (NF1), a genetic condition.
2. What causes Childhood Visual Pathway Glioma?
The exact cause of Childhood Visual Pathway Glioma is not fully understood. However, it is most commonly linked to genetic conditions, particularly neurofibromatosis type 1 (NF1). NF1 is a genetic disorder that increases the risk of developing tumors in the nervous system, including gliomas in the visual pathway. In many cases, VPG develops in children with NF1, although it can occur in children without the condition as well.
3. What are the symptoms of Childhood Visual Pathway Glioma?
The symptoms of Childhood Visual Pathway Glioma can vary depending on the tumor's size and location, but they typically involve vision-related problems, including:
-
Vision loss or blurred vision, often in one or both eyes
-
Changes in visual field, such as loss of peripheral vision
-
Nystagmus (involuntary eye movements)
-
Squinting or difficulty seeing objects clearly
-
Headaches
-
Developmental delays or problems with coordination (if the tumor affects other brain areas)
Since the tumor often grows slowly, symptoms may develop gradually and might be mistaken for less severe issues.
4. How is Childhood Visual Pathway Glioma diagnosed?
Diagnosis of Childhood Visual Pathway Glioma usually involves a combination of the following:
-
Comprehensive eye exam: An ophthalmologist checks for signs of visual impairment and other related symptoms.
-
MRI or CT scans: These imaging tests are used to visualize the tumor's size, location, and involvement with the optic nerve and other areas of the visual pathway.
-
Neuroimaging: MRI is particularly helpful in detecting the tumor and determining whether it’s associated with other brain structures.
-
Genetic testing: In cases where neurofibromatosis is suspected, genetic testing can confirm the diagnosis.
5. What are the treatment options for Childhood Visual Pathway Glioma?
Treatment for Childhood Visual Pathway Glioma depends on the size, location, and symptoms associated with the tumor. Options may include:
-
Observation: If the glioma is small, asymptomatic, and not growing, doctors may recommend regular monitoring with imaging and eye exams.
-
Surgery: In cases where the tumor is causing significant vision loss or other symptoms, surgical removal of the tumor may be considered, though it can be challenging due to its location near sensitive structures.
-
Chemotherapy: This is commonly used for more aggressive or large gliomas to shrink the tumor and manage symptoms.
-
Radiation therapy: This may be considered in cases where surgery is not possible or effective, though it is typically avoided in very young children due to the potential long-term effects on brain development.
6. What is the prognosis for children with Visual Pathway Glioma?
The prognosis for children with Visual Pathway Glioma depends on various factors, including tumor size, location, and whether it is associated with other conditions like neurofibromatosis. Most visual pathway gliomas grow slowly and may be manageable with regular monitoring or non-invasive treatment. However, if the tumor causes significant vision loss or other neurological issues, the outlook can be more complicated. With appropriate treatment, many children have a good quality of life and can maintain vision. Early detection and treatment are crucial for improving the prognosis.
7. How does neurofibromatosis type 1 (NF1) relate to Childhood Visual Pathway Glioma?
Neurofibromatosis type 1 (NF1) is a genetic disorder that increases the risk of developing various types of tumors, including Childhood Visual Pathway Glioma. Around 15-20% of children with NF1 will develop a visual pathway glioma. These tumors are often diagnosed before the age of 6 and can be asymptomatic for a long time. While NF1-related gliomas are typically slow-growing, they require monitoring to prevent complications like vision loss. Treatment for NF1-related gliomas may be tailored to the child’s specific symptoms and needs.
8. What are the potential complications of Childhood Visual Pathway Glioma?
Potential complications of Childhood Visual Pathway Glioma include:
-
Vision impairment: The most common complication, as the tumor can damage the optic nerve and other parts of the visual pathway.
-
Hormonal imbalances: If the tumor affects the hypothalamus or pituitary gland, it may cause hormonal issues.
-
Developmental delays: Large or invasive tumors can affect other areas of the brain, leading to developmental delays or coordination problems.
-
Neurological complications: In rare cases, the tumor can interfere with brain function, leading to headaches, nausea, or seizures.
9. Can Childhood Visual Pathway Glioma recur after treatment?
Yes, Childhood Visual Pathway Glioma can recur, especially if the tumor was not fully removed or if it was treated with less aggressive methods. Tumors that are observed and not treated with surgery or chemotherapy may also grow over time. Regular follow-up appointments with an ophthalmologist and neurologist are essential to monitor for recurrence or new symptoms. If the tumor recurs, additional treatments such as chemotherapy or radiation may be considered.
10. Is there a way to prevent Childhood Visual Pathway Glioma?
There is currently no known way to prevent Childhood Visual Pathway Glioma, especially in children with neurofibromatosis type 1 (NF1). However, early detection through regular eye exams, especially for children diagnosed with NF1 or other genetic conditions, can help detect the tumor at an early, treatable stage. Genetic counseling may also be helpful for families with a history of NF1 to understand the risks and monitor their children closely.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


