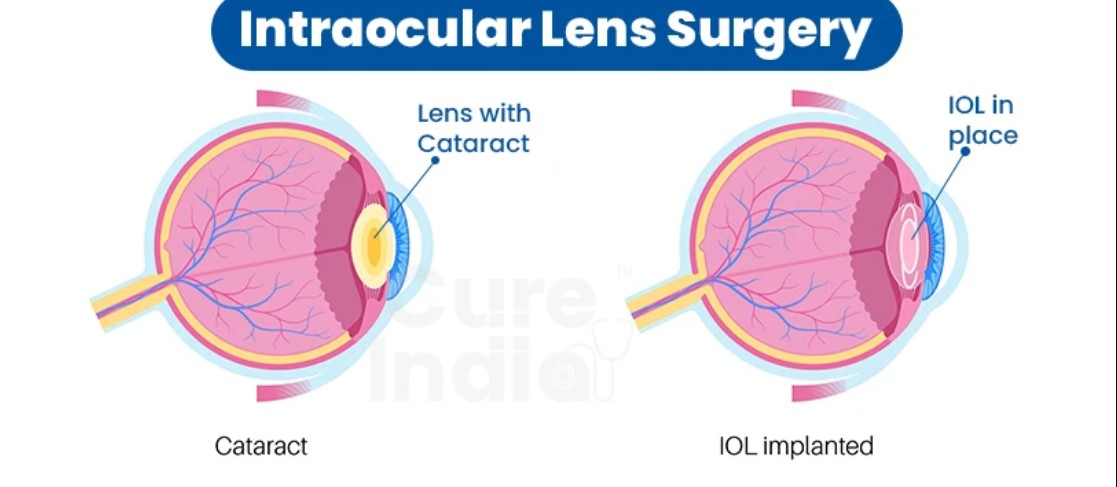
Intraocular Lens Implant Surgery is a well-established and highly effective surgical procedure primarily used to restore vision in individuals suffering from cataracts or other conditions affecting the natural lens of the eye. Cataracts, a clouding of the natural lens, are one of the leading causes of visual impairment worldwide. As the clouded lens impairs light transmission to the retina, individuals may experience blurry or dimmed vision, difficulty seeing in low light, glare, and halos around lights.
Intraocular lenses (IOLs) are artificial lenses that replace the natural, cloudy lens during cataract surgery or refractive surgeries aimed at correcting significant vision issues. This procedure has become one of the most common and successful types of surgery globally, with over 20 million cataract surgeries performed annually.
The main goal of IOL implantation is to restore vision and improve the quality of life of patients affected by vision impairment due to cataracts, refractive errors, or eye injuries. This procedure has gained significant popularity not only for cataract treatment but also as a solution for correcting myopia (nearsightedness), hyperopia (farsightedness), astigmatism, and presbyopia (the inability to focus on close objects as we age). The advent of new and advanced lens technology allows for multifocal vision, and some lenses are even designed to accommodate, much like the natural lens.
The need for IOL implantation arises from various causes that affect the eye’s natural lens, including age-related cataracts, refractive errors, or trauma. Below are the main causes and risk factors that may lead to the need for IOL implant surgery:
1. Cataracts
Cataracts are the leading cause of IOL implantation surgery. They occur when the natural lens of the eye becomes cloudy, blocking light from passing through to the retina. Cataracts are primarily an age-related condition, though they can also result from trauma, genetics, or certain health conditions, such as diabetes.
2. Refractive Errors (Myopia, Hyperopia, Astigmatism)
Refractive errors occur when the eye does not bend light correctly, leading to blurred vision. Some individuals with severe refractive errors (high degrees of nearsightedness or farsightedness) may choose to undergo IOL implant surgery as a part of refractive surgery to reduce or eliminate the need for glasses or contact lenses.
3. Trauma or Eye Injury
Eye injuries or trauma can result in damage to the eye's natural lens, leading to lens dislocation or clouding. In these cases, IOL implantation is often necessary to restore vision.
4. Age and Health Conditions
As people age, the lens in the eye naturally becomes more prone to clouding, leading to age-related cataracts. In addition, health conditions like diabetes or high blood pressure can increase the risk of cataracts and necessitate IOL implantation surgery.
5. Previous Eye Surgery
Certain prior eye surgeries, such as cataract surgery or refractive surgery (e.g., LASIK), may cause complications or vision changes that result in the need for IOL implantation. In some cases, patients who have undergone cataract surgery without IOL implantation may require the procedure later to correct vision problems.
6. Genetic Predisposition
A family history of cataracts or other lens-related issues can increase the likelihood of developing cataracts and the subsequent need for IOL implantation surgery.
The main reason for IOL implantation surgery is to address visual impairment caused by conditions such as cataracts and refractive errors. Symptoms and signs that may indicate the need for IOL implantation surgery include:
1. Cloudy or Blurred Vision
This is one of the hallmark signs of cataracts. As the lens becomes cloudy, individuals may notice blurred or dimmed vision, particularly in low-light conditions. Objects may appear less distinct, and colors may seem dull or faded.
2. Increased Sensitivity to Light (Photophobia)
People with cataracts or other lens issues may experience heightened sensitivity to light, making it difficult to see in bright environments. Glare or halo effects around lights, especially at night, are common complaints.
3. Difficulty with Night Vision
As cataracts develop, night vision often becomes impaired. This can make activities like driving at night dangerous due to a decrease in contrast sensitivity and difficulty seeing in low-light conditions.
4. Double Vision (Diplopia)
Some individuals with cataracts or refractive errors may experience double vision in one or both eyes. This happens because the lens becomes uneven or dislocated, resulting in misalignment and blurred images.
5. Frequent Changes in Eyeglass Prescription
People with cataracts or high refractive errors may notice that their eyeglass prescription is changing more frequently. This is because the lens of the eye becomes less effective at focusing light as cataracts develop or refractive errors increase.
6. Visual Discomfort and Eye Fatigue
People with cataracts or other vision problems may experience eye strain or fatigue, particularly when reading or performing tasks that require focused vision.
Before recommending IOL implant surgery, a comprehensive evaluation by an ophthalmologist or optometrist is essential. Diagnostic steps typically involve:
1. Comprehensive Eye Examination
An ophthalmologist will begin with a thorough eye examination to assess visual acuity, eye health, and the extent of any lens-related problems, such as cataracts or refractive errors.
2. Slit Lamp Examination
A slit lamp is a special microscope that allows the doctor to examine the front structures of the eye, including the cornea, iris, lens, and anterior chamber. This helps to identify cataracts or other eye conditions affecting the lens.
3. Visual Acuity Test
This test involves measuring how clearly a person can see at various distances using an eye chart. The doctor may assess vision with and without corrective lenses to determine the severity of vision impairment.
4. Refraction Test
In this test, the doctor uses lenses of different strengths to determine the exact prescription required to correct refractive errors like nearsightedness, farsightedness, or astigmatism.
5. Ophthalmoscopy
An ophthalmoscope is used to examine the retina and the optic nerve at the back of the eye. This test helps detect signs of cataracts, retinal diseases, or other conditions that could affect the outcome of IOL implant surgery.
6. Biometry (A-Scan Ultrasound)
This test measures the length of the eye and corneal curvature, which are necessary for selecting the correct type of IOL. An ultrasound device is used to assess the axial length of the eye to determine the appropriate lens power.
There are several types of intraocular lenses (IOLs) used in IOL implantation surgery, depending on the patient's condition, preferences, and goals for post-surgical vision:
1. Monofocal IOLs
Monofocal IOLs are the most commonly used type of intraocular lens and provide excellent vision at a single distance, typically for distance vision. Patients who choose monofocal IOLs often require glasses for near tasks like reading or using a computer.
2. Multifocal IOLs
Multifocal IOLs provide multiple points of focus, allowing for better vision at both near and far distances without the need for glasses. These lenses are ideal for patients who want to reduce their dependence on glasses for both distance and near tasks.
3. Toric IOLs
Toric IOLs are specifically designed to correct astigmatism, a condition where the cornea is unevenly shaped, causing blurred vision. Toric lenses provide clearer vision for patients with moderate to high astigmatism.
4. Accommodative IOLs
Accommodative IOLs are designed to mimic the natural focusing ability of the eye. These lenses can shift position inside the eye, allowing the patient to focus on objects at varying distances, offering better flexibility and reducing the need for glasses.
5. Phakic IOLs
In some cases, phakic IOLs are implanted to treat severe refractive errors in patients who are not suitable candidates for laser vision correction surgery like LASIK. These IOLs are placed in the eye without removing the natural lens.
While intraocular lens implant surgery is an effective treatment for restoring vision, it is essential to manage post-operative care to ensure the success of the procedure:
1. Post-Surgical Care
-
Follow-up Appointments: Regular follow-ups with the ophthalmologist are crucial to monitor the healing process, check for complications, and ensure the IOL is functioning correctly.
-
Use of Eye Drops: Patients are typically prescribed antibiotic and anti-inflammatory eye drops to reduce the risk of infection and inflammation after surgery.
-
Protecting the Eye: Patients are advised to wear protective eye shields during sleep and avoid rubbing or pressing on the eye to prevent injury.
2. Lifestyle Modifications
-
Avoiding Heavy Lifting: Patients should refrain from heavy physical activity or lifting objects that could put stress on the eye for several weeks after surgery.
-
Proper Sun Protection: Wearing sunglasses to protect the eye from UV rays can help minimize glare and improve comfort during recovery.
3. Managing Other Eye Conditions
-
If the patient has pre-existing conditions like dry eye or glaucoma, they should follow a management plan in collaboration with their healthcare provider to ensure these conditions do not interfere with the success of the IOL implantation.
While IOL implantation surgery is typically safe and effective, it can still present some risks and potential complications, including:
1. Infection
-
Endophthalmitis, a rare but serious infection inside the eye, can occur after any eye surgery. Proper post-operative care and use of antibiotics help minimize this risk.
2. Graft Rejection
-
Though rare, the body may reject the IOL implant, leading to inflammation, pain, and a loss of vision. Patients may require medications to manage this complication.
3. Glaucoma
-
Some patients may develop elevated intraocular pressure (IOP) following surgery, which can lead to glaucoma if not treated promptly.
4. Lens Dislocation
-
In rare cases, the IOL may shift out of place, leading to vision impairment or the need for additional surgery.
5. Posterior Capsule Opacification (PCO)
-
PCO is a common post-surgical complication where the back of the lens capsule becomes cloudy. This condition can be treated with a YAG laser to restore clear vision.
Most individuals who undergo IOL implant surgery experience significant improvements in vision and a restoration of their quality of life. However, there are important factors to consider during the recovery process and beyond:
1. Vision Rehabilitation
-
Some patients may require vision rehabilitation to adjust to their new IOLs, especially if they are using multifocal or accommodative IOLs. Visual aids or learning new strategies to perform daily tasks may be necessary for some patients.
2. Long-Term Monitoring
-
Even after the successful implantation of an IOL, regular eye exams are essential to ensure the health of the eye and monitor for any potential complications, such as glaucoma or cataracts.
3. Emotional Support
-
For those who have had significant vision loss due to cataracts or other eye conditions, emotional support may be necessary to adjust to the changes in vision and fully appreciate the benefits of the surgery.
1. What is intraocular lens (IOL) implant surgery?
Intraocular lens (IOL) implant surgery is a procedure used to replace a patient's natural lens when it becomes cloudy due to cataracts or other conditions. The surgeon removes the cloudy lens and replaces it with an artificial lens, known as an intraocular lens (IOL). This surgery restores vision and can reduce the need for glasses or contact lenses, depending on the type of IOL used.
2. Why is IOL implant surgery performed?
IOL implant surgery is commonly performed to treat cataracts, which cause clouding of the natural lens in the eye, leading to blurry vision. It is also used to treat other vision problems, such as presbyopia (age-related difficulty focusing), or in some cases, to correct refractive errors like myopia (nearsightedness) or hyperopia (farsightedness) after cataract removal.
3. How does IOL implant surgery work?
During the procedure:
-
Anesthesia: Local anesthesia is applied to numb the eye. The patient may also receive a mild sedative for relaxation.
-
Incision: A small incision is made on the cornea to access the lens.
-
Lens removal: The cloudy natural lens is gently removed using ultrasonic waves (phacoemulsification).
-
IOL implantation: A synthetic intraocular lens is implanted into the eye where the natural lens was removed. The IOL is folded for insertion and then unfolded inside the eye.
-
Recovery: The incision is self-sealing, and no stitches are required in most cases. The procedure usually takes about 15 to 30 minutes.
4. What are the different types of IOLs?
There are several types of intraocular lenses, each designed for specific vision needs:
-
Monofocal IOLs: These provide clear vision at one distance (near, intermediate, or far) and typically require glasses for tasks like reading.
-
Multifocal IOLs: These provide clear vision at multiple distances, reducing the need for glasses for most activities.
-
Accommodating IOLs: These lenses can shift position within the eye, offering improved focus for near and distant vision.
-
Toric IOLs: Designed for patients with astigmatism, these lenses help correct the irregular shape of the cornea.
5. Is intraocular lens implant surgery safe?
Yes, IOL implant surgery is generally very safe and one of the most common and successful procedures performed in ophthalmology. Complications are rare, but as with any surgery, there is some risk. Possible risks include infection, bleeding, retinal detachment, or issues with the lens positioning. Your surgeon will assess your specific case and take necessary precautions to minimize these risks.
6. What is the recovery process after IOL implant surgery?
Recovery after IOL implant surgery is typically quick and straightforward:
-
First few days: Patients may experience mild discomfort, blurry vision, or sensitivity to light.
-
Eye protection: It's important to wear an eye shield or glasses, especially at night, to protect the eye.
-
Medication: Postoperative eye drops are prescribed to prevent infection and reduce inflammation.
-
Follow-up visits: Regular follow-up visits with the surgeon will be scheduled to monitor healing and check for any complications.
-
Return to normal activities: Most patients can resume normal activities within a few days, though strenuous activities or heavy lifting should be avoided for a few weeks.
7. Are there any risks or complications associated with IOL implant surgery?
Although rare, some risks and complications associated with IOL implant surgery include:
-
Infection (Endophthalmitis): This can occur if bacteria enter the eye during surgery, although it is uncommon.
-
Posterior capsule opacification (PCO): Sometimes called a "secondary cataract," this is a condition where the membrane behind the IOL becomes cloudy, affecting vision. It can be treated with a quick laser procedure.
-
Retinal detachment: In some cases, the retina may detach after surgery, requiring prompt treatment.
-
Displacement of the IOL: If the lens shifts out of position, a follow-up surgery may be needed.
8. How long will the results of IOL implant surgery last?
The results of IOL implant surgery are long-lasting. The IOL itself is designed to last a lifetime, and most patients experience a significant improvement in their vision that remains stable. However, the natural aging process may continue to affect vision over time, and in rare cases, additional treatment may be required, such as a YAG laser capsulotomy to treat posterior capsule opacification (PCO).
9. Will I need glasses after IOL implant surgery?
It depends on the type of IOL used and your individual vision needs. For example:
-
Monofocal IOLs: Most patients will need glasses for near vision (reading) after surgery.
-
Multifocal and accommodating IOLs: These lenses can reduce or eliminate the need for glasses, providing good vision at multiple distances.
-
Toric IOLs: These can correct astigmatism, potentially reducing or eliminating the need for glasses for distance vision, but you may still need reading glasses.
10. Can I have IOL implant surgery if I have other eye conditions?
In many cases, patients with other eye conditions such as glaucoma or macular degeneration can still undergo IOL implant surgery, but careful consideration and pre-surgical evaluation are required. The surgeon will assess the overall health of your eyes to determine whether IOL implantation is a suitable option. If you have significant eye disease, your surgeon may recommend alternative treatments or IOL options that are better suited to your condition.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.