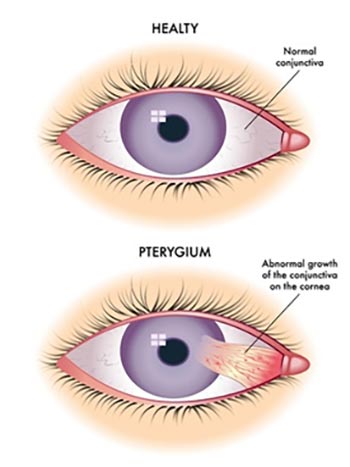
Pterygium is a growth of fleshy tissue on the conjunctiva, the clear membrane covering the white part of the eye (sclera), which can extend onto the cornea (the transparent front part of the eye). Pterygium is often called "surfer's eye" due to its association with prolonged sun exposure, particularly in individuals who spend a lot of time outdoors in sunny and windy conditions. Though it is a benign (non-cancerous) growth, if it becomes large enough, it can distort vision, cause discomfort, and even impair the clarity of vision if it covers the cornea.
Pterygium removal refers to the surgical excision of this tissue, and it is typically performed when the growth causes visual disturbances or significant eye irritation. While smaller pterygia may be managed conservatively with eye drops or UV protection, larger, more symptomatic pterygia may require surgical intervention.
The procedure to remove a pterygium is typically performed under local anesthesia, and it is relatively straightforward. However, because the growth tends to recur, surgeons often use advanced techniques like conjunctival autografting or amniotic membrane grafting to reduce the likelihood of recurrence. After the surgery, patients are generally advised to follow post-operative care instructions, including the use of eye drops and maintaining eye protection.
The goal of pterygium removal surgery is to restore clear vision, relieve symptoms such as irritation and dryness, and prevent further growth of the tissue, especially over the cornea.
Pterygium occurs when the conjunctiva (the thin tissue covering the white part of the eye) becomes abnormal due to excessive irritation or inflammation. While the exact cause of pterygium is not fully understood, certain environmental and genetic factors contribute significantly to its development. Here are the common causes and risk factors associated with pterygium:
1. UV Radiation Exposure
Prolonged exposure to ultraviolet (UV) radiation, particularly UV-B rays, is the primary cause of pterygium. UV rays from the sun can damage the delicate tissues of the conjunctiva, leading to the abnormal growth of tissue. Individuals who spend a lot of time outdoors, especially in sunny and tropical climates, are at higher risk of developing pterygium.
2. Environmental Irritants
In addition to UV radiation, dust, wind, pollution, and other environmental irritants can damage the eyes and promote the growth of pterygium. This is especially true for individuals who work in dusty or windy environments, such as construction sites, agriculture, or manufacturing, where eye irritation is more likely to occur.
3. Age
Age is a significant risk factor for pterygium. While it can develop at any age, pterygium is most commonly diagnosed in individuals aged 20 to 50 years, and the prevalence increases with age. This is partly due to the cumulative effects of UV radiation and long-term exposure to environmental irritants over time.
4. Gender
Men are generally more likely than women to develop pterygium, likely due to greater exposure to the sun and environmental factors. Outdoor workers and those who engage in outdoor sports are particularly at risk, and the condition is more commonly diagnosed in men due to their higher rates of outdoor activities.
5. Genetic Predisposition
A family history of pterygium can increase the risk of developing the condition, suggesting a potential genetic link. If an individual’s close family members have had pterygium, they may be more susceptible to developing it themselves.
6. Pre-existing Eye Conditions
Certain ocular conditions, such as dry eye syndrome or ocular surface disease, may increase the risk of developing pterygium. In addition, individuals who have had previous eye surgeries, such as cataract surgery, may be at increased risk of developing pterygium, particularly if there is scarring of the ocular surface.
Pterygium can cause a variety of symptoms, depending on the size and location of the growth. While smaller pterygia may not cause significant issues, larger ones can interfere with vision and cause discomfort. Common symptoms and signs that may lead to pterygium removal include:
1. Redness in the Eye
A visible redness or inflammation in the white part of the eye is one of the first signs of pterygium. The abnormal tissue can cause irritation, which leads to an increase in blood vessels and redness.
2. Foreign Body Sensation
People with pterygium often describe a sensation of something being in the eye, similar to the feeling of a foreign body or sand. This discomfort can be persistent, especially in the morning or after long hours of outdoor activity.
3. Blurry Vision
If the pterygium grows over the cornea, it can distort vision by changing the shape of the cornea, leading to blurry or distorted vision. This can be particularly problematic when the pterygium extends into the visual axis.
4. Dryness and Irritation
Pterygium can lead to dry eye symptoms, such as burning, itching, and excessive tearing. The growth can disrupt the normal tear film on the eye’s surface, leading to dryness and discomfort.
5. Sensitivity to Light (Photophobia)
As the pterygium irritates the eye, it can lead to increased sensitivity to light (photophobia). People with pterygium may find it uncomfortable to be in bright environments, or experience discomfort when exposed to fluorescent lighting.
6. Increased Growth
In some cases, the pterygium may continue to grow across the cornea, leading to increasing visual disturbances and discomfort. The decision to undergo pterygium removal is often made when the growth becomes large enough to affect vision or quality of life.
The diagnosis of pterygium is typically made during a comprehensive eye exam. The ophthalmologist will evaluate the severity of the growth and its effect on vision, and determine if surgical removal is necessary. Diagnostic tests may include:
1. Visual Acuity Test
A visual acuity test is used to assess how well the patient can see at various distances. If the pterygium is interfering with vision, this test will help determine the extent of the impairment.
2. Slit Lamp Examination
A slit lamp is an essential tool for diagnosing pterygium. It allows the ophthalmologist to examine the cornea, conjunctiva, and retina under high magnification. The doctor can assess the size, shape, and location of the pterygium and determine whether it is affecting the visual axis.
3. Corneal Topography
If the pterygium has caused significant distortion in the cornea, corneal topography may be used to map the surface of the cornea. This can help assess the degree of astigmatism or corneal irregularity caused by the pterygium.
4. Pachymetry
Pachymetry is used to measure the thickness of the cornea. This can help assess the impact of the pterygium on the deeper layers of the cornea and whether it has caused any permanent damage to the corneal structure.
When a pterygium causes discomfort or visual impairment, surgical removal is often necessary. Treatment options include:
1. Conservative Treatments
For small pterygia that do not cause significant discomfort or vision impairment, conservative treatments such as artificial tears, anti-inflammatory medications, and UV protection (such as wearing sunglasses) may be sufficient to manage symptoms. These treatments help to reduce irritation, dryness, and swelling, but they do not remove the growth.
2. Surgical Removal
For larger or more symptomatic pterygia, surgical excision is the most effective treatment. The surgery typically involves:
-
Removing the abnormal tissue from the conjunctiva.
-
Using a graft of tissue from the patient’s own eye or an amniotic membrane to cover the surgical site, which helps reduce the risk of recurrence.
There are various surgical techniques for pterygium removal, including:
-
Simple excision: The pterygium is surgically removed, and the area is sutured closed.
-
Conjunctival autografting: A graft from the patient’s own eye is used to cover the surgical site, significantly reducing the likelihood of recurrence.
-
Amniotic membrane grafting: The amniotic membrane is used as a graft to promote healing and reduce scarring.
3. Post-Surgical Care
After surgery, patients are often prescribed antibiotic and anti-inflammatory eye drops to prevent infection and reduce swelling. UV-blocking sunglasses are also recommended to protect the healing eye from harmful sun exposure.
While it may not always be possible to prevent pterygium, there are several steps individuals can take to reduce the risk and manage existing conditions:
1. UV Protection
The best preventive measure for pterygium is protection from UV radiation. Wearing sunglasses with UV protection and wide-brimmed hats can reduce the exposure of the eyes to harmful rays. It is important to wear sunglasses whenever outdoors, particularly in sunny or high-altitude areas.
2. Avoiding Environmental Irritants
Wearing protective eyewear (such as goggles) in windy, dusty, or polluted environments can help reduce the irritation that may lead to pterygium formation. This is particularly important for people working in construction, agriculture, or mining, where eye protection is crucial.
3. Regular Eye Exams
Routine eye exams, especially for individuals at higher risk (e.g., those with prolonged sun exposure or a family history of pterygium), can help detect pterygium early and allow for timely intervention if necessary.
While pterygium removal surgery is generally safe, there are potential risks and complications, including:
1. Recurrence
One of the most common complications after pterygium removal is recurrence, where the pterygium regrows. This is especially common in individuals who continue to be exposed to UV radiation or who have large pterygia. To reduce the risk of recurrence, surgeons often use conjunctival autografts or amniotic membrane grafts.
2. Infection
Although rare, infections can occur after pterygium removal surgery. Following the surgeon’s post-operative care instructions and using antibiotic eye drops can help minimize the risk of infection.
3. Scarring
Some patients may develop scarring at the site of the excision, leading to vision distortion or discomfort. Proper healing and avoiding unnecessary eye strain are important to minimize scarring.
4. Dry Eyes
After surgery, some individuals may experience dry eyes or irritation due to changes in the eye’s surface. This can usually be managed with artificial tears and other lubricating eye drops.
After pterygium removal surgery, most patients experience significant improvement in vision and a reduction in discomfort. However, post-operative care and lifestyle changes are essential for optimal recovery:
1. Follow-Up Care
It is crucial to attend follow-up appointments with your ophthalmologist to monitor the healing process, check for any complications (such as infection or recurrence), and adjust medications as necessary.
2. Eye Protection
To prevent recurrence, it is essential to wear UV-blocking sunglasses when outdoors and avoid prolonged exposure to sun or environmental irritants. Protective eyewear can help shield the eyes from potential damage.
3. Managing Dryness
Some patients may experience dry eye symptoms following surgery. Using artificial tears and avoiding rubbing the eyes can help manage this condition and improve comfort.
4. Adjusting to Vision Changes
If a pterygium has caused astigmatism or changes in the shape of the cornea, you may need to adjust to new vision after surgery. Some individuals may benefit from glasses or contact lenses to correct any residual refractive error.
1. What is pterygium?
Pterygium is a non-cancerous growth of tissue on the conjunctiva (the clear membrane covering the white part of the eye) that can extend onto the cornea (the clear front part of the eye). It is often referred to as "surfer’s eye" because it is more common in people who spend long periods in the sun, particularly in outdoor environments. Pterygium is typically caused by environmental factors, such as prolonged exposure to UV light, dust, and wind.
2. What are the symptoms of pterygium?
Pterygium can cause a variety of symptoms, including:
-
Redness and irritation in the eye.
-
A feeling of something in the eye (foreign body sensation).
-
Blurred vision, particularly if the pterygium grows over the cornea.
-
Dryness and discomfort, particularly in windy or sunny conditions.
-
Cosmetic concerns: The growth can become visible on the eye, causing aesthetic issues for some individuals.
3. What is pterygium removal surgery?
Pterygium removal surgery is a procedure to remove the growth of tissue (pterygium) from the surface of the eye. The goal is to improve vision and alleviate discomfort caused by the pterygium. During the surgery, the pterygium tissue is carefully excised from the eye, and the area is typically covered with a small graft (either from the patient’s own tissue or from a donor) to help prevent recurrence and promote healing.
4. Why is pterygium removal necessary?
Pterygium removal is usually necessary when:
-
The pterygium interferes with vision by growing onto the cornea.
-
There is significant irritation, redness, or discomfort that doesn't improve with medications or eye drops.
-
The appearance of the pterygium becomes bothersome.
-
The pterygium recurs despite conservative treatments or eye drops.
In some cases, pterygium can cause astigmatism (distorted vision), making removal more crucial.
5. How is pterygium removal surgery performed?
Pterygium removal surgery typically involves the following steps:
-
Anesthesia: The patient is given local anesthesia to numb the eye.
-
Incision: A small incision is made, and the pterygium is carefully removed from the eye’s surface.
-
Graft placement: To reduce the risk of recurrence, a graft (either from the patient’s own conjunctiva or a donor tissue) is placed over the area where the pterygium was removed.
-
Sutures: Small stitches are used to secure the graft in place, though in some cases, sutures may not be needed.
-
Recovery: The eye is bandaged, and the patient is provided with medications to prevent infection and reduce inflammation.
The procedure is typically performed on an outpatient basis, meaning the patient can go home the same day.
6. What is the recovery like after pterygium removal surgery?
Recovery from pterygium removal surgery generally takes a few weeks:
-
First few days: The eye may feel scratchy, and there could be mild redness and swelling. Pain can usually be managed with prescribed eye drops and over-the-counter pain relief.
-
1-2 weeks: Most patients can resume normal activities, but it’s important to avoid strenuous activities, rubbing the eye, or exposure to irritants like smoke or dust.
-
1 month: Vision typically stabilizes, and the eye heals fully, with follow-up visits to ensure proper healing and to monitor for any signs of recurrence.
Full recovery can take up to 6 weeks, depending on the individual’s healing process.
7. Are there any risks or complications associated with pterygium removal surgery?
While pterygium removal surgery is generally safe, there are potential risks and complications, including:
-
Recurrence: The pterygium can return after surgery, especially if the graft doesn’t fully adhere.
-
Infection: As with any surgery, there is a risk of infection, though it is rare.
-
Scarring: Some patients may develop scarring or irregular healing on the surface of the eye.
-
Dry eye: Post-surgical dryness or irritation can occur as the eye heals.
-
Glare or visual disturbances: Some patients may experience increased sensitivity to light or glare during recovery.
Your surgeon will provide specific instructions to minimize these risks and help ensure a smooth recovery.
8. How long does it take for the pterygium to heal after surgery?
Healing after pterygium removal surgery typically takes a few weeks, with most patients seeing improvement in vision and comfort within 2 to 4 weeks. Full healing, including the absorption of the graft, can take 1 to 2 months. Regular follow-up visits will be necessary to monitor progress and ensure there are no complications during recovery.
9. Will I need glasses after pterygium removal surgery?
Most patients do not need glasses after pterygium removal surgery unless the pterygium caused significant vision changes prior to surgery. If the pterygium caused astigmatism, the surgery should help improve vision, though glasses or contact lenses may be needed if astigmatism persists. After healing, your doctor will assess your vision and may recommend corrective lenses if necessary.
10. How can I prevent pterygium from returning after surgery?
To prevent recurrence of pterygium after surgery, the following measures are recommended:
-
Protection from UV light: Wear sunglasses or a wide-brimmed hat to protect your eyes from harmful UV rays, as exposure to the sun is a primary risk factor for pterygium development.
-
Avoid irritants: Minimize exposure to wind, dust, or smoke, as these can irritate the eye and potentially lead to recurrence.
-
Follow-up care: Attend all post-operative appointments and follow your surgeon’s recommendations for recovery, including the use of prescribed eye drops to reduce inflammation and prevent infection.
By following these guidelines, you can reduce the risk of pterygium returning and promote long-term eye health.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.