Kidney transplantation is a surgical procedure in which a diseased or failing kidney is replaced with a healthy kidney from a donor. The kidneys play a crucial role in the body by filtering waste and excess fluids from the blood, regulating blood pressure, balancing electrolytes, and producing hormones that are important for overall health. When both kidneys fail, a kidney transplant becomes a vital treatment option to restore kidney function and improve the patient's quality of life.
Kidney transplants are generally recommended when a person has end-stage renal disease (ESRD), a condition in which the kidneys lose nearly all of their function. ESRD can occur due to various underlying conditions such as diabetes, hypertension, or glomerulonephritis, where the kidneys are damaged beyond repair. While dialysis can help manage kidney failure for a time, a kidney transplant is often the best long-term solution.
The kidney transplant procedure involves the implantation of a healthy donor kidney into the recipient's body, which will take over the kidney functions. The procedure can offer many benefits, including improved quality of life, reduced dependence on dialysis, and prolonged survival. However, a successful kidney transplant requires careful matching between the donor and recipient, as well as lifelong monitoring and immunosuppressive medication to prevent graft rejection.
Kidney transplantation is generally considered for individuals whose kidneys have failed, and this failure is often due to one of several underlying conditions. Below are the most common causes and risk factors associated with kidney failure and the need for a kidney transplant:
1. Diabetes
Diabetes is the leading cause of kidney failure. Over time, high blood sugar levels can damage the blood vessels in the kidneys, impairing their ability to filter waste and fluids. Diabetic nephropathy, a type of kidney damage caused by diabetes, is a major contributor to the development of end-stage renal disease.
2. Hypertension
Chronic high blood pressure (hypertension) is the second most common cause of kidney failure. Uncontrolled hypertension can damage the blood vessels in the kidneys, leading to kidney disease and ultimately kidney failure. Hypertension-related kidney disease can progress to end-stage renal disease if left untreated.
3. Glomerulonephritis
Glomerulonephritis refers to inflammation of the glomeruli, which are the filtering units within the kidneys. This condition can lead to kidney damage and is often a result of autoimmune diseases or infections. If glomerulonephritis progresses, it can cause chronic kidney disease and kidney failure, necessitating a transplant.
4. Polycystic Kidney Disease (PKD)
Polycystic kidney disease is an inherited condition in which fluid-filled cysts grow on the kidneys, leading to progressive kidney damage and, eventually, kidney failure. PKD is one of the genetic disorders that can lead to the need for a kidney transplant.
5. Chronic Kidney Infections (Pyelonephritis)
Repeated kidney infections can scar the kidneys and impair their function over time. Severe or recurrent pyelonephritis can lead to kidney failure, making a transplant necessary when the kidneys can no longer function properly.
6. Acute Kidney Injury (AKI)
Severe episodes of acute kidney injury, often caused by trauma, infection, or severe dehydration, can result in permanent kidney damage. In cases where AKI leads to permanent kidney damage that cannot be reversed, a kidney transplant may be the only viable treatment option.
7. Autoimmune Diseases
Certain autoimmune diseases like lupus and Goodpasture's syndrome can attack and damage the kidneys, leading to kidney failure. These conditions may require a transplant if kidney function is severely compromised.
8. Obesity
Obesity increases the risk of developing conditions like diabetes and hypertension, which are both risk factors for kidney disease. Morbid obesity can exacerbate kidney damage and accelerate the progression of kidney failure.
9. Family History and Genetics
A family history of kidney disease, particularly polycystic kidney disease, diabetic nephropathy, or hypertension-related kidney disease, increases the likelihood of developing kidney failure. Genetic predisposition can play a significant role in the development of kidney disease, necessitating a kidney transplant in some cases.
The symptoms that lead to the consideration of kidney transplantation typically result from the gradual decline in kidney function. Kidney failure causes a range of signs and symptoms that affect a person’s health and well-being:
1. Decreased Urine Output
A common sign of kidney failure is a significant decrease in urine output. The kidneys are unable to filter waste and produce urine, leading to retention of fluids and waste products in the body.
2. Swelling (Edema)
Kidney failure leads to fluid retention, which can cause swelling in the legs, ankles, feet, and face. Swelling is due to the kidneys’ inability to remove excess fluid from the body, leading to edema.
3. Fatigue
Fatigue and weakness are common in kidney failure because the kidneys can no longer filter waste from the blood effectively, leading to the buildup of toxins that make the body feel sluggish and tired.
4. Shortness of Breath
Shortness of breath can occur due to the accumulation of fluid in the lungs (pulmonary edema) as a result of kidney failure. This can make it difficult to breathe, particularly when lying flat or engaging in physical activity.
5. High Blood Pressure
Hypertension or high blood pressure is both a cause and a symptom of kidney failure. When the kidneys are not functioning properly, the body has difficulty regulating blood pressure, leading to persistent hypertension.
6. Nausea and Vomiting
Nausea and vomiting often occur in individuals with kidney failure due to the buildup of uremia (waste products) in the bloodstream. This can lead to discomfort, loss of appetite, and weight loss.
7. Confusion and Cognitive Impairment
As kidney function declines, toxins and waste products accumulate in the body, which can affect brain function. This can lead to confusion, difficulty concentrating, or more severe symptoms like delirium.
8. Persistent Itching
Pruritus or persistent itching can occur when waste products build up in the bloodstream. This symptom can be distressing and is common in individuals with chronic kidney disease (CKD) or end-stage renal disease (ESRD).
9. Metallic Taste in Mouth
Uremia can cause a metallic taste in the mouth, which may reduce appetite and contribute to malnutrition. This occurs when waste products build up in the body and affect the taste buds.
The decision to undergo a kidney transplant is made after thorough evaluation by a medical team to ensure the patient is a suitable candidate. The following diagnostic tests are essential for evaluating kidney function and determining whether a transplant is necessary:
1. Blood Tests
-
Serum Creatinine: A blood test that measures the level of creatinine, a waste product normally filtered by the kidneys. Elevated levels indicate kidney dysfunction.
-
Glomerular Filtration Rate (GFR): The GFR is a measure of how well the kidneys are filtering blood. A GFR below 15 mL/min/1.73m² indicates kidney failure and the need for a transplant.
-
Blood Urea Nitrogen (BUN): This test measures the amount of urea nitrogen in the blood, another waste product the kidneys normally filter. High BUN levels indicate impaired kidney function.
2. Urine Tests
-
Urinalysis: A urine test that examines the presence of protein, blood, or abnormal cells in the urine. Proteinuria (excessive protein in the urine) is a common sign of kidney damage.
-
24-Hour Urine Collection: This test measures the total amount of waste products being filtered by the kidneys over a 24-hour period, helping to assess kidney function.
3. Kidney Biopsy
In some cases, a kidney biopsy may be performed to assess the extent of kidney damage. A small sample of kidney tissue is extracted and examined under a microscope to determine the cause and stage of kidney disease.
4. Imaging Studies
-
Ultrasound: A kidney ultrasound can evaluate the size, shape, and structure of the kidneys and identify any blockages, cysts, or tumors.
-
CT Scan: A computed tomography (CT) scan may be used to assess kidney anatomy and identify any structural abnormalities.
5. Electrocardiogram (ECG)
An ECG may be performed to assess heart function, especially since heart disease is a common complication of kidney failure.
Kidney transplantation is the treatment of choice for individuals with end-stage renal disease (ESRD) when other treatments like dialysis are not sufficient. Below are the key treatment options:
1. Dialysis (Pre-Transplantation)
While waiting for a kidney transplant, individuals may undergo dialysis to perform the function of the kidneys. Hemodialysis and peritoneal dialysis are two main types of dialysis that help remove waste products and excess fluids from the body. Dialysis is not a cure for kidney failure but helps manage symptoms while awaiting a transplant.
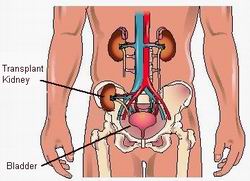
2. Kidney Transplant Surgery
When a suitable donor kidney becomes available, the patient undergoes kidney transplant surgery. The transplant involves:
-
Removal of the diseased kidney (in some cases).
-
Implantation of the donor kidney in the lower abdomen.
-
Connection of the new kidney to the patient’s blood vessels and urinary tract.
3. Immunosuppressive Medications
After the transplant, the patient will need to take immunosuppressive drugs to prevent graft rejection, which occurs when the body's immune system recognizes the new kidney as foreign and attempts to attack it. These medications are crucial for the success of the transplant but come with the risk of infection and organ damage.
While kidney transplantation is a life-saving procedure, the following steps are important for managing kidney health before, during, and after transplantation:
1. Control of Underlying Conditions
Patients with conditions such as diabetes or hypertension must work closely with their healthcare team to manage these conditions to prevent further kidney damage and complications.
2. Regular Monitoring
After transplantation, the patient will require regular follow-up visits to monitor kidney function, check for signs of rejection, and adjust medications as necessary. This includes regular blood tests, urine tests, and imaging studies.
3. Adherence to Medication
Adhering to prescribed immunosuppressive medications and other post-transplant drugs is crucial to the success of the transplant. Missing doses can increase the risk of rejection or infection.
While kidney transplantation offers significant benefits, it also carries certain risks and potential complications:
1. Graft Rejection
Graft rejection occurs when the immune system recognizes the transplanted kidney as foreign and attacks it. Symptoms of rejection include fever, pain at the transplant site, and decreased urine output.
2. Infection
Post-transplant patients are at an increased risk of infections due to the use of immunosuppressive medications that weaken the immune system. Common infections include urinary tract infections, pneumonia, and wound infections.
3. Cardiovascular Disease
Kidney transplant patients are at an increased risk of developing heart disease and hypertension, both of which can impact kidney function and overall health.
4. Diabetes
Immunosuppressive medications can increase the risk of new-onset diabetes, making blood sugar management important post-transplant.
Living with a kidney transplant requires ongoing care, lifestyle changes, and a commitment to medical management:
1. Follow-Up Care
Frequent check-ups with a transplant nephrologist are necessary to monitor kidney function, adjust medications, and address any potential issues early. Patients may need routine lab tests, imaging, and visits to specialized clinics.
2. Emotional Support
Living with a transplant can be both physically and emotionally challenging. Psychological support and counseling may help individuals manage the emotional impact of the transplant process.
3. Healthy Lifestyle
Maintaining a healthy diet, regular physical activity, and adequate rest is essential for transplant success. Preventing obesity, maintaining a healthy weight, and avoiding smoking can improve transplant outcomes and overall health.
1. What is kidney transplantation?
Kidney transplantation is a surgical procedure in which a healthy kidney from a donor is placed into a patient whose kidneys are no longer functioning properly. The new kidney helps filter waste products and excess fluid from the body, replacing the function of the patient's failed kidneys. Kidney transplants are typically performed when a person has end-stage kidney failure, which can be caused by diseases like diabetes, hypertension, or polycystic kidney disease.
2. Why is kidney transplantation needed?
Kidney transplantation is needed for patients suffering from end-stage renal disease (ESRD), also known as kidney failure, when the kidneys can no longer perform their essential functions. This can occur due to:
-
Chronic conditions: Diabetes, hypertension, and glomerulonephritis can lead to kidney damage over time.
-
Polycystic kidney disease: A genetic disorder that leads to the formation of cysts in the kidneys.
-
Acute kidney injury: Resulting from trauma, infections, or severe dehydration.
When kidney function drops to a critical level, dialysis (a process that mimics kidney function) may be required, and a kidney transplant becomes the most effective treatment option.
3. What are the types of kidney transplants?
There are two main types of kidney transplants:
-
Living donor transplant: A kidney is donated by a living person, usually a relative or friend who is a compatible match. Living donor transplants tend to have better outcomes due to shorter wait times and the generally healthier condition of the kidney.
-
Deceased donor transplant: A kidney is donated by a person who has passed away. These kidneys are allocated based on compatibility, blood type, and the urgency of the recipient’s condition.
4. How is kidney transplantation performed?
Kidney transplantation involves the following steps:
-
Anesthesia: The patient is given general anesthesia to ensure they are unconscious and pain-free during the procedure.
-
Incision: The surgeon makes an incision in the lower abdomen to place the donor kidney.
-
Removal of failed kidneys (optional): In most cases, the recipient’s damaged kidneys are left in place. Only in certain cases will the failed kidneys be removed.
-
Placement of the new kidney: The donor kidney is placed in the lower abdomen, and blood vessels are connected to the new kidney.
-
Closure: The incision is closed, and the kidney is monitored to ensure it starts functioning properly.
The surgery typically lasts about 3 to 4 hours, and the patient is closely monitored in the hospital for recovery.
5. Is kidney transplantation a painful procedure?
Kidney transplantation is performed under general anesthesia, so patients do not experience pain during the surgery. After the procedure, some discomfort, soreness, or pain at the incision site is normal, but this can usually be managed with pain medication. Patients may also experience mild swelling or bruising. The recovery process varies from person to person, but most patients begin to feel better within a few days to weeks.
6. What is the recovery time after kidney transplantation?
The recovery time after kidney transplantation varies, but generally:
-
Hospital stay: Most patients stay in the hospital for 7 to 10 days for initial recovery and monitoring of kidney function.
-
First few weeks: Patients may experience fatigue, mild discomfort, and gradual improvements in kidney function. Follow-up visits are necessary to monitor the new kidney’s performance.
-
Long-term recovery: It can take several months to fully recover and adapt to life with the new kidney. Patients may need to take immunosuppressive medications to prevent organ rejection.
-
Full recovery: In most cases, patients are able to return to normal activities, including work and exercise, within 3 to 6 months.
7. What are the risks and complications of kidney transplantation?
As with any surgery, kidney transplantation carries some risks and potential complications, including:
-
Rejection: The body’s immune system may recognize the new kidney as foreign and try to reject it. This is why immunosuppressive medications are given to prevent rejection.
-
Infection: Due to the use of immunosuppressive drugs, patients are at higher risk of infections.
-
Delayed graft function: In some cases, the new kidney may take time to start working, requiring temporary dialysis.
-
Blood clots: There is a risk of blood clots forming in the kidney’s blood vessels.
-
Cancers: Long-term use of immunosuppressive drugs can increase the risk of certain cancers, especially skin cancer.
-
High blood pressure and diabetes: Some medications and the transplant process may increase the risk of high blood pressure or diabetes.
8. How long does a kidney transplant last?
A kidney transplant can last for 10 to 20 years or more, depending on factors like the patient’s age, overall health, the quality of the donor kidney, and how well the patient follows their post-transplant care plan. Most transplanted kidneys begin to lose function over time, but with proper management, many patients can enjoy years of healthy living with a transplanted kidney. Regular check-ups and taking immunosuppressive medications are crucial to maintaining kidney function.
9. Will I need to take medications after a kidney transplant?
Yes, after a kidney transplant, patients must take immunosuppressive medications to prevent rejection of the new kidney. These medications suppress the immune system, making it less likely to attack the transplanted organ. Patients will also need other medications to control blood pressure, cholesterol, and prevent infections. These medications must be taken exactly as prescribed, and regular follow-up visits with the transplant team are essential to monitor for side effects and adjust dosages.
10. Can kidney transplantation cure kidney disease?
While kidney transplantation can effectively restore kidney function and improve quality of life, it is not a cure for kidney disease. The underlying cause of kidney failure, such as diabetes, hypertension, or polycystic kidney disease, may still be present and requires ongoing management. The new kidney may eventually fail over time, which could require dialysis or another transplant. However, kidney transplantation provides a significant improvement in life expectancy and quality of life for many patients compared to staying on dialysis.
The other Organ Transplant Procedures are:
- Lung Transplantation
- Bone Marrow Transplantation
- Cornea Transplantation
- Heart Transplantation… etc
Few Major Hospitals for Kidney Transplant are:
- Wockhardt Hospitals
- Apollo Hospitals
- Max Healthcare
- Amrita Institute of Medical Sciences
- Piyavate Hospital
- Florence Nightingale Hospital
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



