Endoscopic Retrograde Cholangiopancreatography (ERCP) is a sophisticated procedure used to diagnose and treat various conditions affecting the bile ducts, pancreatic ducts, and gallbladder. It combines endoscopy and fluoroscopy to allow doctors to examine the bile and pancreatic ducts and treat any blockages or abnormalities.
ERCP is typically performed for conditions that cause obstructions, inflammation, or other complications in the bile or pancreatic ducts. These can include gallstones, tumors, strictures (narrowing of the ducts), and pancreatitis (inflammation of the pancreas). The procedure is often used in patients who have symptoms like abdominal pain, jaundice, and unexplained weight loss, and when other diagnostic methods, like ultrasound or CT scans, are insufficient.
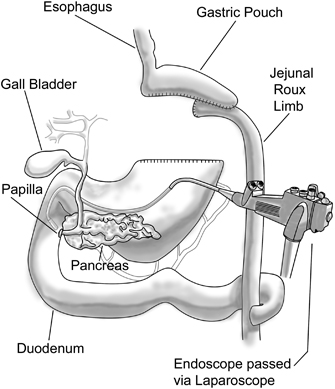
During the ERCP procedure, a flexible tube (an endoscope) with a light and camera is inserted into the body via the mouth, esophagus, and stomach, and into the small intestine. A special dye is injected through the endoscope into the bile or pancreatic ducts, and X-ray images are then taken to assess any issues.
While ERCP is primarily used for diagnosis, it is also a therapeutic procedure, allowing the removal of stones, placement of stents, and even biopsy collection for suspected cancers or other disorders.
The need for ERCP typically arises when certain diseases or conditions affect the bile or pancreatic ducts. Understanding these causes and risk factors helps to identify who is more likely to benefit from ERCP:
1. Gallstones (Cholelithiasis)
Gallstones are hardened deposits of bile that form in the gallbladder. When they travel into the bile ducts, they can block the flow of bile, causing pain, infections, and jaundice. ERCP can be used to locate and remove these stones, allowing the normal flow of bile to resume.
2. Bile Duct Strictures (Narrowing)
Bile duct strictures can develop as a result of scarring from surgery, infections, or inflammatory conditions like primary sclerosing cholangitis (PSC). These strictures narrow the bile ducts, impeding bile flow, and are often treated with ERCP by placing stents to keep the ducts open.
3. Pancreatitis
Pancreatitis is the inflammation of the pancreas, often caused by gallstones that block the pancreatic duct. This blockage can result in pain, nausea, vomiting, and fever. ERCP helps diagnose the blockage and can be used therapeutically to remove stones or place stents.
4. Tumors
Tumors in the pancreas or bile ducts, including cholangiocarcinoma (bile duct cancer) and pancreatic cancer, can obstruct bile flow and cause jaundice. ERCP helps diagnose these cancers and can be used to obtain tissue samples through biopsy or insert stents to maintain bile flow.
5. Infections
Cholangitis, an infection of the bile ducts, can occur when there is an obstruction. Bacterial infections in the bile ducts can lead to fever, pain, and jaundice. ERCP can be used to drain infected bile and remove the blockage to prevent further infections.
6. Post-Surgical Complications
After certain surgeries, especially those involving the gallbladder or bile ducts, patients may develop leaks or blockages that require ERCP to clear. ERCP can help to diagnose and treat these post-surgical complications.
The symptoms that might indicate the need for ERCP typically stem from blockages or other issues in the bile or pancreatic ducts. Common symptoms include:
1. Jaundice
Jaundice (yellowing of the skin and eyes) occurs when there is a blockage in the bile ducts that prevents bile from being processed correctly. This leads to an accumulation of bilirubin in the blood. Jaundice is often one of the primary symptoms that prompts doctors to recommend ERCP.
2. Abdominal Pain
Pain in the upper right abdomen is common in patients with gallstones or bile duct blockages. This pain may be intermittent or constant and can be accompanied by nausea and vomiting. In more severe cases, the pain may radiate to the back or shoulder.
3. Nausea and Vomiting
Persistent nausea or vomiting that occurs alongside abdominal pain or jaundice could suggest that there is a blockage or infection in the bile ducts. This symptom often leads to the decision to perform an ERCP for diagnosis and treatment.
4. Unexplained Weight Loss
Weight loss, particularly when associated with jaundice, abdominal pain, and fatigue, can indicate the presence of a tumor or infection in the pancreas or bile ducts. ERCP may be performed to diagnose and treat the underlying cause.
5. Fever and Chills
Fever, particularly when it occurs with jaundice and abdominal pain, may indicate cholangitis, an infection of the bile ducts. In this case, ERCP can help drain infected bile and relieve the blockage.
6. Dark Urine and Pale Stools
Dark urine and pale stools are signs of bile duct obstruction. When bile can't flow into the intestines, it leads to darker urine and lighter stools. ERCP is used to identify and treat the underlying obstruction.
ERCP is both a diagnostic and therapeutic procedure, which means it is used not only to identify the causes of symptoms but also to treat underlying conditions. The diagnostic process leading to ERCP typically includes:
1. Medical History and Physical Exam
A healthcare provider will start by taking a detailed medical history and performing a physical exam to understand the patient's symptoms. This includes questions about pain, nausea, vomiting, history of gallstones, or any other underlying liver or gastrointestinal issues.
2. Imaging Tests
-
Ultrasound: Ultrasound is often the first test performed to evaluate the liver, gallbladder, and bile ducts. It can identify gallstones, enlarged bile ducts, or tumors in the liver or pancreas.
-
CT Scan: A CT scan is often used to provide a detailed look at the abdomen, liver, and pancreas, and can reveal blockages, tumors, or inflammation that may require ERCP.
-
MRI and MRCP: Magnetic Resonance Cholangiopancreatography (MRCP) is a specialized MRI technique used to visualize the bile ducts and pancreatic ducts without the need for invasive procedures. MRCP can help identify obstructions or abnormalities before proceeding to ERCP.
3. Blood Tests
Blood tests can assess liver function, the presence of infection, and other relevant markers. Liver function tests are essential for diagnosing liver damage, while amylase and lipase tests can help diagnose pancreatitis.
4. Urodynamic Studies
In certain cases, urodynamic studies may be used to assess how well the bladder and urethra are functioning together. This test helps determine if there is any impaired function or blockage that needs surgical intervention.
ERCP is both a diagnostic and therapeutic procedure, which means it can be used to treat conditions after identifying them. The treatment options during ERCP typically include:
1. Stone Removal
The most common use of ERCP is the removal of gallstones or pancreatic duct stones. This is done using a variety of tools, including a basket or balloon to grasp and remove the stones from the ducts.
2. Stent Placement
When there is a stricture (narrowing) in the bile ducts or pancreatic ducts, stent placement can help keep the duct open. A small, flexible tube (stent) is placed in the narrowed area to allow bile to flow freely again.
3. Dilation of Strictures
In cases of bile duct strictures or narrowing, ERCP can be used to perform a procedure called balloon dilation, where a balloon catheter is inflated inside the narrowed duct to widen it and restore normal bile flow.
4. Biopsy Collection
During ERCP, biopsy samples may be taken if cancer or other abnormalities are suspected. The endoscope is used to collect tissue samples from the bile ducts or pancreas for further analysis.
5. Drainage of Infected Bile
In cases of cholangitis or infected bile ducts, ERCP can be used to drain infected bile and remove any blockages causing the infection.
While some causes of bile duct and pancreatic issues are unavoidable, there are several preventive measures that can reduce the risk of requiring ERCP:
1. Maintain a Healthy Diet
A diet low in fat and high in fiber can help prevent the formation of gallstones, one of the most common reasons for ERCP. Reducing alcohol intake can also prevent liver disease and pancreatitis.
2. Manage Existing Health Conditions
Conditions such as diabetes and high cholesterol can increase the risk of liver and bile duct issues. Regular monitoring and proper management of these conditions can help reduce the need for ERCP.
3. Regular Health Screenings
Routine screenings and check-ups, especially for individuals at higher risk of bile duct blockages (e.g., those with gallstones or a family history of liver disease), can help detect issues early before they require more invasive treatment.
While ERCP is a valuable procedure, it does come with potential risks and complications:
1. Pancreatitis
One of the most common complications of ERCP is pancreatitis, which is inflammation of the pancreas. This occurs when the procedure irritates or injures the pancreatic ducts. While most cases are mild, severe pancreatitis can require hospitalization.
2. Infection
As with any invasive procedure, there is a risk of infection. Infections in the bile ducts or pancreas can occur, especially if there is a delay in treating blockages or infections.
3. Bleeding
Minor bleeding can occur during ERCP, especially if a biopsy is performed or a stent is placed. In rare cases, more significant bleeding may require additional treatment.
4. Perforation
In rare instances, the endoscope or other instruments used in ERCP can accidentally perforate the bile ducts or the surrounding tissue, leading to further complications that require surgical repair.
1. Rest and Recovery:
-
Most patients can return to normal activities within a few days after ERCP. Rest is important during the recovery phase, especially if any therapeutic interventions were performed.
2. Diet and Hydration:
-
Patients are usually advised to follow a liquid diet for a short time after the procedure, progressing to soft foods before returning to a regular diet. Staying hydrated is essential for kidney and liver health.
3. Monitoring for Complications:
-
Patients should watch for signs of infection, fever, or worsening pain. Follow-up appointments with the physician are necessary to monitor recovery and address any complications that may arise.
1. What is ERCP?
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a procedure used to diagnose and treat problems in the bile ducts, gallbladder, and pancreas. During ERCP, a flexible tube (endoscope) is inserted through the mouth, down the esophagus, into the stomach, and into the duodenum (the first part of the small intestine). A contrast dye is then injected into the bile or pancreatic ducts, and X-rays are taken to identify blockages, strictures, or other abnormalities.
2. Why is ERCP performed?
ERCP is performed to diagnose and treat conditions affecting the bile ducts, pancreas, or gallbladder, including:
-
Gallstones: To detect and remove stones from the bile duct.
-
Bile duct obstruction: Caused by tumors, scar tissue, or strictures.
-
Pancreatitis: To evaluate the cause of inflammation in the pancreas.
-
Cholangiocarcinoma: To diagnose cancer of the bile ducts.
-
Jaundice: To identify the underlying cause of yellowing of the skin or eyes.
-
Narrowing or strictures in the bile or pancreatic ducts: Often caused by scarring from previous conditions or surgeries.
ERCP helps both in diagnosing and treating these conditions by allowing the doctor to take tissue samples, remove blockages, and place stents if needed.
3. What happens during an ERCP procedure?
During an ERCP, the following steps are typically involved:
-
Sedation: The patient is given a sedative to relax and a local anesthetic to numb the throat.
-
Insertion of the endoscope: A flexible tube (endoscope) is inserted through the mouth and gently advanced into the duodenum.
-
Contrast dye injection: A small catheter is threaded through the endoscope into the bile or pancreatic ducts, and a contrast dye is injected.
-
X-ray imaging: X-rays are taken to evaluate the bile ducts, pancreatic ducts, and other structures for any abnormalities.
-
Treatment (if needed): If necessary, the doctor can remove stones, take biopsies, place stents, or dilate strictures during the same procedure.
The procedure typically takes 30 to 60 minutes.
4. Is ERCP painful?
Most patients experience little to no pain during an ERCP procedure due to the use of sedation and local anesthetics. However, some discomfort, such as bloating, mild cramping, or a sore throat, is common afterward as the body recovers from the procedure. Pain medications can be prescribed if needed, and these symptoms generally subside within a few hours to a day.
5. What are the risks and complications of ERCP?
While ERCP is generally safe, there are some risks and potential complications, including:
-
Pancreatitis: Inflammation of the pancreas, which can occur after ERCP in about 5% of cases.
-
Infection: In rare cases, infection can occur in the bile ducts or pancreas.
-
Perforation: The endoscope or instruments may cause a tear in the digestive tract, though this is rare.
-
Bleeding: There is a small risk of bleeding, particularly if a biopsy is taken or a stent is placed.
-
Allergic reactions: Rare reactions to the contrast dye or medications used during the procedure.
Your doctor will evaluate the risks and benefits and take steps to minimize complications.
6. How long does it take to recover from ERCP?
ERCP is generally an outpatient procedure, meaning patients can usually go home the same day. Most people can resume normal activities within 24 to 48 hours after the procedure. However, some mild discomfort, such as bloating or a sore throat, may persist for a few days. If any treatments (such as stent placement) were performed, additional recovery time may be necessary, and follow-up appointments will be scheduled to monitor healing.
7. How do I prepare for an ERCP?
To prepare for ERCP, you will typically need to:
-
Fast: You will be asked to avoid eating or drinking for 6 to 8 hours before the procedure to ensure an empty stomach.
-
Medications: Inform your doctor about any medications you are taking, as certain medications (such as blood thinners) may need to be temporarily adjusted.
-
Consent: You will need to sign a consent form after discussing the procedure and any potential risks with your doctor.
Your healthcare provider will give you detailed instructions before the procedure, and it’s essential to follow them carefully to ensure the best results.
8. What is the recovery time after ERCP?
Most patients recover quickly after ERCP:
-
Immediate recovery: After the procedure, you will be monitored in a recovery area for 1 to 2 hours until the sedative wears off.
-
Return to activities: You can usually return to light activities within 1 to 2 days. However, it’s important to avoid heavy lifting or strenuous activities for a few days.
-
Follow-up: If any treatments were performed, such as stone removal or stent placement, additional follow-up may be required to ensure proper healing.
Your doctor will provide instructions for post-procedure care, which may include dietary restrictions or taking prescribed medications.
9. Can ERCP be used to treat problems, or is it just diagnostic?
ERCP is both a diagnostic and a therapeutic procedure. It allows doctors to identify problems in the bile ducts, pancreatic ducts, or gallbladder, but it can also be used to treat certain conditions during the same procedure. Some common therapeutic treatments performed during ERCP include:
-
Stone removal: Stones blocking the bile ducts can be removed using specialized tools.
-
Stent placement: Stents may be inserted to keep ducts open and allow proper bile flow.
-
Dilation: Strictures (narrowed areas) in the bile or pancreatic ducts can be stretched to improve flow.
-
Biopsy: Tissue samples can be taken for further analysis if cancer or other conditions are suspected.
10. How much does ERCP cost?
The cost of ERCP can vary based on factors such as the complexity of the procedure, the healthcare facility, and the region in which it is performed. On average, the cost of an ERCP procedure can range from $1,500 to $5,000. Additional costs may be incurred if therapeutic treatments (such as stone removal or stent placement) are required. Insurance often covers ERCP if it is medically necessary, but it’s important to check with your insurance provider for specific coverage details.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.

