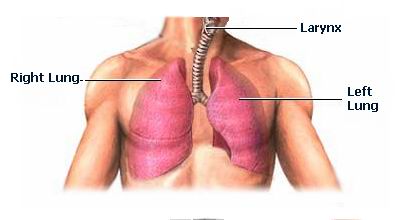
A lung transplant is a surgical procedure in which a diseased or failing lung is replaced with a healthy lung from a donor. This procedure is typically performed on individuals with end-stage lung disease who have not responded to other treatments, including medications or mechanical ventilation. The goal of a lung transplant is to restore lung function, alleviate symptoms, and improve the patient's quality of life.
Several chronic lung diseases can lead to irreversible lung damage, necessitating a lung transplant. Understanding the underlying causes of lung disease can help in identifying candidates for this life-saving procedure.
Common Causes of Lung Disease Needing a Transplant:
-
Chronic Obstructive Pulmonary Disease (COPD): A progressive lung disease that causes airflow obstruction, often due to smoking, resulting in difficulty breathing, cough, and frequent respiratory infections.
-
Pulmonary Fibrosis: A condition in which lung tissue becomes scarred and stiff, making it difficult for the lungs to expand and oxygenate the body. This can be caused by various factors, including environmental exposures and autoimmune diseases.
-
Cystic Fibrosis: A genetic disorder that leads to thick, sticky mucus accumulation in the lungs, causing respiratory problems, infections, and eventually lung failure.
-
Idiopathic Pulmonary Hypertension: A rare condition where high blood pressure occurs in the arteries of the lungs, causing the heart to work harder and eventually leading to heart and lung failure.
-
Pulmonary Arterial Hypertension: A type of high blood pressure that affects the arteries in the lungs, leading to heart failure and requiring a transplant when other treatments fail.
-
Alpha-1 Antitrypsin Deficiency: A genetic disorder that can cause lung and liver damage, leading to early-onset emphysema and COPD.
-
Lung Cancer: In some cases, lung cancer patients may undergo a lung transplant following the removal of a tumor if the cancer has not spread.
-
Severe, Refractory Asthma: In rare cases, severe asthma that cannot be controlled by other treatments may require a lung transplant.
Risk Factors for Lung Disease:
-
Smoking: The leading cause of COPD and lung cancer. Long-term smoking significantly increases the risk of developing chronic lung diseases.
-
Genetics: Inherited conditions like cystic fibrosis and alpha-1 antitrypsin deficiency increase the risk of lung disease.
-
Environmental Factors: Exposure to pollutants, toxins, and chemicals can damage the lungs and contribute to conditions like pulmonary fibrosis.
-
Age: The risk of lung disease increases with age, especially for diseases like pulmonary fibrosis and COPD.
Lung transplant candidates typically experience severe symptoms as their lung function declines. These symptoms can significantly affect daily life and the ability to perform routine tasks. Common symptoms indicating the need for a lung transplant include:
Common Symptoms of End-Stage Lung Disease:
-
Severe shortness of breath: Difficulty breathing even at rest or with minimal physical exertion.
-
Fatigue: Feeling excessively tired, even after rest, due to the body’s reduced oxygen supply.
-
Chronic cough: A persistent cough that does not improve, often accompanied by phlegm.
-
Chest tightness: A sensation of pressure or discomfort in the chest, making it hard to breathe deeply.
-
Cyanosis: A bluish tint to the lips, fingers, or toes caused by low oxygen levels in the blood.
-
Swelling: Fluid retention in the legs, ankles, or abdomen due to reduced heart and lung function.
-
Frequent respiratory infections: Recurrent pneumonia or bronchitis due to weakened lung defenses.
-
Decreased ability to perform daily activities: Patients may find it increasingly difficult to complete tasks such as walking, climbing stairs, or carrying groceries.
If a person experiences any of these symptoms, especially if they are progressively worsening, it’s important to consult a healthcare provider to determine whether a lung transplant is necessary.
The decision to proceed with a lung transplant involves a thorough evaluation to assess the patient's overall health, the severity of lung disease, and the likelihood of success from the surgery. Several tests and diagnostic tools are used to determine whether a lung transplant is appropriate.
Diagnostic Tests Include:
-
Pulmonary Function Tests (PFTs): These tests measure lung capacity, airflow, and oxygen exchange, helping to assess the severity of lung dysfunction.
-
Chest X-ray: A chest X-ray provides an image of the lungs and can help identify abnormalities such as fluid buildup, scarring, or masses.
-
High-Resolution CT Scan: Provides detailed images of the lungs to evaluate lung tissue damage and other conditions such as pulmonary fibrosis or emphysema.
-
Arterial Blood Gas Test: Measures oxygen levels in the blood to assess the lungs' ability to oxygenate the body effectively.
-
6-Minute Walk Test: Assesses exercise tolerance and oxygen saturation during physical activity.
-
Echocardiogram: Evaluates heart function and checks for signs of pulmonary hypertension, a condition that may affect the eligibility for a lung transplant.
-
Blood Tests: Used to evaluate the patient's overall health, including kidney and liver function, and to screen for infections or other underlying health conditions.
-
Psychosocial Assessment: Psychological and social evaluations are crucial to ensure that the patient can handle the emotional and lifestyle challenges that come with a lung transplant.
Once these tests are completed, a multidisciplinary team—including pulmonologists, transplant surgeons, and other specialists—will review the results to determine whether a lung transplant is appropriate.
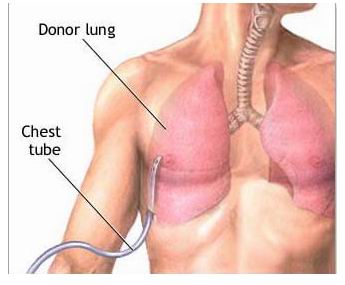
A lung transplant is a complex and highly specialized surgery that involves removing one or both of the patient's damaged lungs and replacing them with healthy donor lungs. The procedure is usually performed under general anesthesia and involves the following steps:
Steps Involved in Lung Transplant Surgery:
-
Preparation: The patient is placed under general anesthesia and is intubated with a ventilator to assist with breathing during surgery.
-
Incision: An incision is made in the chest, typically through the sternum (breastbone) or side of the chest, depending on whether one or both lungs are being transplanted.
-
Removal of the damaged lung: The damaged lung(s) are carefully removed, ensuring that the surrounding tissue is preserved as much as possible.
-
Transplantation of the donor lung: The healthy donor lung is then placed into the chest cavity, and the bronchus, arteries, and veins are connected to the patient’s circulatory system.
-
Closure and recovery: After ensuring the lung is properly connected and functioning, the chest incision is closed. The patient is then placed on a ventilator and closely monitored in an intensive care unit (ICU) for several days.
Lung transplants may involve either a single-lung transplant or a double-lung transplant, depending on the patient’s condition and the availability of suitable donor lungs.
As with any major surgery, lung transplantation carries risks, particularly due to the complexity of the procedure and the need for lifelong immunosuppressive medications to prevent organ rejection. Some potential risks and complications include:
Rejection of the donor lung: The body may recognize the transplanted lung as foreign and attempt to reject it. This is managed with immunosuppressive medications, but rejection can still occur.
-
Infection: After surgery, the immune system is suppressed, which increases the risk of infections.
-
Blood clots: Clots may form in the lungs or other areas of the body after surgery, leading to complications such as pulmonary embolism.
-
Lung dysfunction: The transplanted lung may not function properly, leading to a need for additional treatments or interventions.
-
Chronic rejection: Over time, the transplanted lung may begin to show signs of chronic rejection, leading to reduced lung function and possibly the need for another transplant.
Your transplant team will closely monitor you for these risks and provide medications and interventions as needed to address any issues that arise.
After a lung transplant, patients must undergo a significant recovery period, including a hospital stay and continued monitoring for complications. Most patients spend several weeks in the hospital, where they are monitored for signs of rejection, infection, and other complications.
Recovery Tips:
-
Follow-up appointments: Frequent visits to the transplant center are necessary to monitor lung function and detect any signs of rejection.
-
Medications: Lifelong use of immunosuppressive medications is required to prevent rejection. Patients must also take medications to manage infections and other health conditions.
-
Physical therapy: Patients will need to participate in pulmonary rehabilitation to regain strength and improve lung function.
-
Lifestyle changes: Patients are encouraged to maintain a healthy diet, avoid smoking or exposure to harmful substances, and stay active to optimize lung function.
The recovery process can be long and challenging, but with proper care and monitoring, most patients experience significant improvements in their quality of life.
A lung transplant can significantly improve the quality of life for individuals with severe lung disease. While the recovery process is long, many patients can return to normal activities, including walking, exercising, and enjoying daily tasks. Lifestyle Considerations: Physical activity: Regular exercise is vital to maintain lung function and overall health after the transplant. Diet: A healthy diet can help prevent complications such as high blood pressure, diabetes, and other issues that may affect long-term health. Support groups: Joining a lung transplant support group can help patients cope with the emotional and physical challenges of recovery. With proper care, a lung transplant can extend life expectancy, improve the quality of life, and allow patients to resume many normal activities.
The other major Cardiac procedures are:
Few Major Hospitals for Lung Transplantation are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Cystic Fibrosis | Living Donor Lobar Lung Transplant | Lung Function Test | Blood Gas Test | Arterial | Double Transplant | Bilateral Transplant | Chest Cavity | Drainage Tubes | Single Lung Transplantation | Immunosuppressant Medicines | Bronchus | Pulmonary Artery | Pulmonary Vein | Hospitals Lung Transplant | Doctors Lung Transplant | Surgery Lung Transplant | Cost Lung Transplant | Treatment Lung Transplant | Destinations Lung Transplant | Lung Transplant India | Lung Transplant Recovery | Lung Transplant Information | Lung Transplant Thailand | Lung Transplant Malaysia | Lung Transplant Abroad | Lung Transplant Overseas | Lung Transplant Low Cost
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


