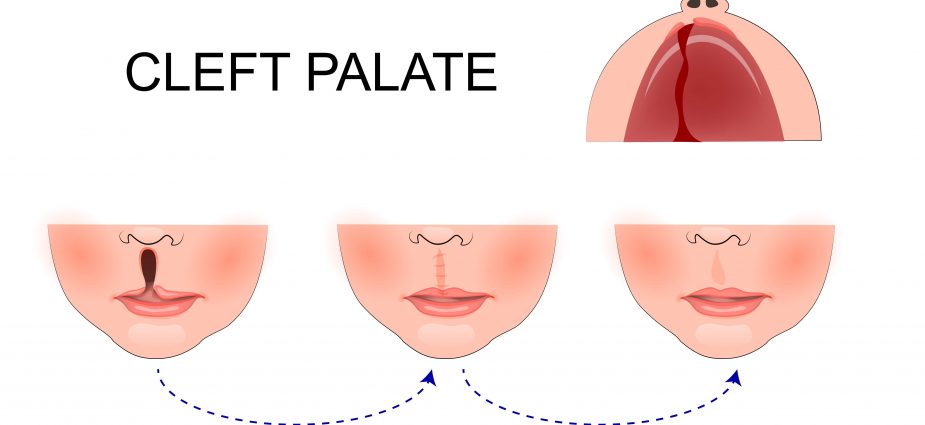
Cleft palate is a congenital deformity characterized by an opening or split in the roof of the mouth that occurs when the tissues of the palate do not fuse completely during fetal development. This defect can vary in severity from a small notch in the soft palate to a large gap extending through both the soft and hard palate, affecting the function and appearance of the oral cavity.
The cleft palate may occur alone or in conjunction with a cleft lip, which involves a fissure in the upper lip. Both conditions are among the most common birth defects globally, affecting approximately 1 in every 700 live births, although incidence rates vary by ethnicity and geographic location.
The condition impacts essential functions such as feeding, speech, hearing, and dental development, often resulting in complications like recurrent ear infections and difficulties with speech intelligibility. Fortunately, cleft palate repair surgery, coupled with a multidisciplinary care approach, allows most patients to achieve near-normal oral function and appearance.
This article delves into the causes, symptoms, diagnosis, treatment options, preventive strategies, possible complications, and lifelong management associated with cleft palate and its repair.
The formation of the palate occurs between the 6th and 9th weeks of embryonic development. During this period, two shelves of tissue grow on either side of the developing mouth and normally fuse in the midline. Failure of this fusion results in a cleft palate.
Genetic Factors
Genetic predisposition plays a significant role in cleft palate formation:
-
Familial inheritance: Children born to parents or siblings with clefts have a higher risk.
-
Chromosomal abnormalities: Certain chromosomal syndromes, such as Trisomy 13 or 18, are associated with cleft anomalies.
-
Single-gene mutations: Mutations in genes involved in craniofacial development (e.g., IRF6, MSX1) can lead to isolated clefts or syndromic clefts.
-
Syndromes: Around 30% of cleft palate cases are part of syndromes, such as Pierre Robin sequence, Stickler syndrome, or Treacher Collins syndrome, where multiple congenital anomalies co-exist.
Environmental and Maternal Risk Factors
Non-genetic factors contributing to cleft palate include:
-
Maternal smoking and alcohol consumption: Both are teratogenic and increase the risk of orofacial clefts.
-
Nutritional deficiencies: Lack of folic acid, vitamin B6, or zinc during pregnancy can impair normal palate formation.
-
Exposure to teratogens: Certain medications (like anticonvulsants—phenytoin, valproic acid), illicit drugs, or environmental toxins have been linked to clefts.
-
Maternal health conditions: Uncontrolled diabetes mellitus, infections such as rubella, and obesity have been implicated.
-
Advanced maternal age also appears to slightly elevate risk.
Multifactorial Etiology
Most cases of cleft palate are attributed to a combination of multiple genes interacting with environmental factors. The precise mechanisms are still under investigation, but this interplay influences palate development outcomes.
The clinical presentation of cleft palate varies depending on the size and location of the defect, but commonly includes:
Feeding and Nutrition Issues
-
Newborns with cleft palate often have difficulty creating suction due to the open connection between the mouth and nasal cavity.
-
Infants may exhibit prolonged feeding times, choking, gagging, or nasal regurgitation of milk.
-
Poor weight gain and failure to thrive may result if feeding problems are not managed early.
Speech and Language Difficulties
-
A cleft palate interferes with normal speech production by affecting airflow and resonance.
-
Common speech problems include hypernasality (excessive nasal sound), articulation errors, nasal air escape, and compensatory speech habits.
-
Without repair and therapy, speech intelligibility can be severely compromised, affecting social development.
Ear and Hearing Problems
-
Dysfunction of the Eustachian tube due to abnormal palate muscles leads to middle ear fluid accumulation.
-
This increases the risk of recurrent otitis media (ear infections) and conductive hearing loss.
-
Untreated hearing loss may further impair speech and language development.
Dental and Facial Anomalies
-
Malformed, missing, or misaligned teeth near the cleft site are frequent.
-
The alveolar ridge (bone holding teeth) may be interrupted, complicating tooth eruption.
-
Facial growth may be affected, resulting in maxillary hypoplasia (underdeveloped upper jaw).
Psychological and Social Impact
-
Children with visible clefts may experience psychosocial challenges including self-esteem issues and social stigma.
-
Early intervention and supportive care are critical to help children and families cope.
Early and accurate diagnosis is vital to coordinate appropriate care and plan treatment.
Prenatal Diagnosis
-
Ultrasound Imaging: Routine second-trimester ultrasound can detect cleft lip and sometimes cleft palate. The sensitivity varies and isolated cleft palate can be difficult to identify prenatally.
-
3D/4D Ultrasound: Offers enhanced visualization of facial structures, improving diagnostic accuracy.
-
Fetal MRI: Utilized in select cases for detailed anatomical assessment.
-
Genetic Testing: If there is suspicion of associated syndromes, chromosomal microarray or targeted gene panels may be performed.
Postnatal Clinical Assessment
-
At birth, the cleft palate is typically visible on physical examination.
-
A careful oral examination is performed, sometimes requiring use of a flashlight or palpation.
-
Feeding assessment is conducted to identify swallowing or sucking difficulties.
-
Hearing evaluation with tympanometry or audiometry is important due to risk of otitis media.
-
Speech evaluation usually starts once the child develops vocalization skills.
Multidisciplinary Evaluation
-
A cleft team typically includes plastic surgeons, ENT specialists, pediatricians, speech-language pathologists, orthodontists, and geneticists.
-
This team performs comprehensive assessments to plan individualized treatment.
Cleft palate treatment is primarily surgical, with a timeline and approach tailored to the child’s age, cleft severity, and associated conditions.
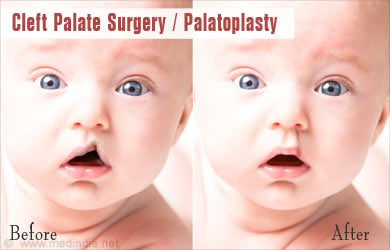
Surgical Repair (Palatoplasty)
-
Surgery is generally scheduled between 6 and 18 months to optimize speech outcomes.
-
The goal is to close the cleft, restore the muscular sling of the soft palate, and create a functional separation between the oral and nasal cavities.
-
Common surgical techniques:
-
Furlow Double Opposing Z-plasty: Reconstructs the soft palate muscles to improve speech.
-
Von Langenbeck Palatoplasty: Raises mucoperiosteal flaps to close the cleft.
-
Two-flap Palatoplasty: Widely used for wide clefts.
-
-
Some children may require multiple surgeries for complete closure or revision.
Adjunctive Treatments
-
Feeding support: Specialized bottles and feeding devices aid nutrition before surgery.
-
Speech therapy: Initiated postoperatively to correct articulation and resonance problems.
-
Ear tube placement: Myringotomy with ventilation tubes is commonly done to prevent fluid buildup and hearing loss.
-
Orthodontic treatment: Starts in early childhood to address dental crowding or malocclusion.
-
Alveolar bone grafting: Typically performed around 7-9 years old to support teeth and stabilize the maxilla.
-
Secondary surgeries: May be required for speech improvement (velopharyngeal insufficiency correction) or cosmetic refinements.
Emerging and Supportive Therapies
-
Research continues on tissue engineering, stem cell therapies, and genetic approaches to enhance repair outcomes.
-
Psychosocial counseling and parental education are vital components of comprehensive care.
Though not all clefts are preventable, several strategies can reduce risk:
Prevention
-
Prenatal vitamins: Folic acid supplementation before conception and during pregnancy reduces cleft risk.
-
Avoiding teratogens: Pregnant women should avoid smoking, alcohol, and unnecessary medications.
-
Maternal health optimization: Managing chronic diseases and infections during pregnancy is critical.
-
Genetic counseling: Families with history of clefts or syndromes benefit from risk assessment and counseling.
-
Public health awareness: Education about nutrition and prenatal care improves outcomes.
Management
-
Early referral to a cleft team ensures coordinated care from birth.
-
Supportive therapies address feeding, speech, hearing, and dental needs.
-
Family-centered care provides emotional support and guidance.
-
Long-term follow-up extends into adolescence and adulthood to monitor facial growth, speech, and psychosocial development.
Despite surgical advancements, some complications may arise:
Surgical Complications
-
Fistula formation: Persistent openings between the oral and nasal cavities may develop post-surgery.
-
Velopharyngeal insufficiency: Incomplete closure of the soft palate during speech causing hypernasality.
-
Scarring and tissue contracture: Affecting palate mobility.
-
Anesthetic risks: Especially in infants, including airway difficulties and systemic complications.
Functional Complications
-
Hearing impairment: Ongoing middle ear problems may require repeated interventions.
-
Speech disorders: Some children need further speech therapy or corrective surgeries.
-
Dental and orthodontic issues: Malocclusion or jaw growth abnormalities may necessitate surgical correction.
-
Psychological impact: Body image concerns or social challenges persist if not adequately addressed.
Prevention of Complications
-
Close follow-up and early intervention reduce severity.
-
Multidisciplinary care allows for timely management of arising problems.
Children born with cleft palate can lead healthy, fulfilling lives with comprehensive treatment and support.
Medical and Therapeutic Follow-Up
-
Regular visits to cleft teams, speech therapists, audiologists, and orthodontists are essential.
-
Early intervention promotes optimal speech and hearing development.
-
Surgical and orthodontic treatments may continue through adolescence.
Psychosocial Wellbeing
-
Children may face challenges related to appearance, speech, or social acceptance.
-
Counseling, peer support groups, and educational assistance help foster confidence and resilience.
-
Families play a crucial role in advocacy and emotional support.
Adult Life and Transition
-
Adults who had cleft repair may require ongoing dental care or cosmetic procedures.
-
Speech issues usually stabilize but therapy remains helpful if needed.
-
Awareness and acceptance have improved, reducing stigma.
1. What is cleft palate repair surgery?
Cleft palate repair is a surgical procedure to close the opening in the roof of the mouth (palate) caused by a cleft. This helps restore normal function for eating, speaking, and breathing.
2. At what age is cleft palate repair usually performed?
The surgery is commonly performed when a baby is between 6 to 18 months old. Timing depends on the child’s health, cleft severity, and surgeon’s recommendation.
3. What causes a cleft palate?
A cleft palate occurs due to incomplete fusion of the tissues in the roof of the mouth during fetal development. Causes may include genetic factors, environmental exposures, or a combination of both.
4. How is the surgery performed?
The surgeon carefully repositions and stitches the muscles and tissues of the palate to close the gap. This reconstructs the palate, enabling better feeding and speech development.
5. What are the risks and complications of cleft palate repair?
Risks include bleeding, infection, fistula formation (small holes reopening), speech difficulties, and anesthesia-related complications. These are minimized by experienced surgical teams and proper care.
6. How long does the surgery take?
The procedure typically lasts 1 to 3 hours depending on the complexity of the cleft and the surgical technique used.
7. What is the recovery process like?
Post-surgery, babies may stay in the hospital for 1-2 days for monitoring. Feeding instructions and wound care are critical. Most children heal well within a few weeks.
8. Will my child need speech therapy after surgery?
Many children benefit from speech therapy to improve articulation and language skills after surgery, especially if there were delays or difficulties before repair.
9. Can cleft palate be completely fixed with surgery?
Surgery can close the cleft and restore function, but some children may need additional surgeries or therapies to address speech, dental, or hearing issues.
10. How can I prepare my child for cleft palate repair?
Follow your surgeon’s pre-op guidelines, ensure the child is healthy, and discuss any concerns. Emotional support and understanding are important for parents and caregivers.
The other Cosmetic Procedures are:
Few Popular Hospitals for Cleft Palate Repair are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.