Pharyngoplasty is a surgical procedure aimed at correcting the structure and function of the pharynx (throat) to improve speech, swallowing, and breathing. The most common use of pharyngoplasty is in patients with velopharyngeal insufficiency (VPI), which is a condition where the soft palate does not adequately close the space between the nasal and oral cavities during speech. This leads to symptoms like hypernasality and nasal air emission.
VPI may occur due to a variety of reasons, including congenital defects, trauma, or complications from previous surgeries, such as cleft palate repairs. In addition to speech issues, pharyngoplasty can be indicated for improving airway obstruction in conditions like obstructive sleep apnea (OSA), where the pharyngeal muscles or tissue structures block airflow during sleep.
Pharyngoplasty techniques vary based on the underlying condition, the severity of symptoms, and the specific anatomy of the individual. The main goal is to improve the functional and aesthetic aspects of the pharyngeal region to restore normal speech and breathing patterns.
Pharyngoplasty is often necessary when the velopharyngeal mechanism (the structure involving the soft palate and pharyngeal walls) does not function properly. There are various causes of this dysfunction, some of which are congenital, while others are acquired over time.
Congenital Causes:
-
Cleft Palate: A cleft palate is one of the most common congenital defects leading to velopharyngeal insufficiency. This occurs when the palate does not fully fuse during fetal development, leading to a gap or hole in the upper part of the mouth.
-
Submucous Cleft Palate: A less visible form of cleft palate that can cause VPI, where the tissues covering the palate appear intact, but the underlying muscles and structures are not fully formed.
-
Congenital Hypotonia: Some individuals are born with weak muscles, including the muscles controlling the soft palate and pharyngeal structures, leading to VPI and subsequent need for pharyngoplasty.
Acquired Causes:
-
Neuromuscular Disorders: Conditions such as cerebral palsy, muscular dystrophy, or other neurogenic conditions can affect the pharyngeal muscles, leading to speech and swallowing difficulties.
-
Trauma or Injury: Accidents or surgical interventions that damage the pharyngeal or soft palate muscles may cause VPI, particularly if the muscle control necessary for speech or swallowing is compromised.
-
Post-surgical Complications: Some patients who have undergone surgeries like adenoidectomy, tonsillectomy, or cleft palate repair may develop issues with velopharyngeal closure, necessitating pharyngoplasty.
Risk Factors:
-
Age: Children and adults may experience different challenges in treatment, and the success of surgery may vary depending on the age of the patient.
-
Severity of Condition: Those with more severe cases of VPI or sleep apnea may require more complex and invasive surgical options.
-
Underlying Health Conditions: Individuals with respiratory issues, chronic allergies, or other pre-existing health problems may face additional complications during or after surgery.
-
Genetics: In some cases, a genetic predisposition to conditions like cleft palate or other congenital abnormalities can increase the likelihood of needing pharyngoplasty.
The need for pharyngoplasty is often driven by noticeable symptoms that impair speech and/or breathing. Common symptoms that may indicate the necessity for pharyngoplasty include:
Speech-related Symptoms:
-
Hypernasality: This refers to speech that has an excessively nasal quality due to incomplete closure of the velopharyngeal port (the space between the soft palate and the pharyngeal walls).
-
Nasal Air Emission: Air escaping through the nose during speech, which is often coupled with hypernasality.
-
Weak or Inconsistent Speech: In some cases, the person may have difficulty producing certain consonant sounds, especially pressure sounds like "p," "t," "k," and "s."
-
Speech Delay or Developmental Issues: Children with VPI may experience delayed speech development due to the difficulties in vocalization caused by the inability to close the palate properly.
Breathing and Swallowing Symptoms:
-
Obstructive Sleep Apnea (OSA): Many individuals with VPI or other pharyngeal issues experience sleep apnea, characterized by interrupted or shallow breathing during sleep. This occurs when the tissues in the pharynx collapse and obstruct the airway.
-
Snoring: Excessive snoring is another common symptom of sleep-related issues due to inadequate airway function.
-
Difficulty Swallowing: If the pharyngeal muscles are impaired, swallowing food or liquid may become difficult or uncomfortable.
-
Frequent Ear Infections: If the Eustachian tube, which connects the ear to the throat, is not functioning correctly, it can lead to ear infections.
A thorough diagnostic process is essential for determining whether pharyngoplasty is needed and which type of surgery is appropriate. Several tests and evaluations may be performed to assess the condition of the velopharyngeal mechanism.
1. Clinical Evaluation:
A healthcare provider will begin by reviewing the patient’s medical history and conducting a physical examination. This may involve checking for signs of VPI, such as nasal speech or difficulty swallowing.
2. Nasopharyngoscopy:
This procedure involves inserting a flexible endoscope through the nose to observe the velopharyngeal area while the patient speaks. It allows the surgeon to directly assess the functioning of the soft palate, pharyngeal walls, and nasal cavity.
3. Videofluoroscopy:
In this diagnostic test, X-ray images are captured while the patient speaks. This allows the doctor to observe how the soft palate moves and whether there is any abnormality in the velopharyngeal closure during speech.
4. Speech Assessment:
Speech-language pathologists will evaluate the patient’s speech patterns, including resonance and articulation. This helps to determine how much speech therapy or surgical intervention may be necessary.
5. Sleep Studies (Polysomnography):
For individuals with suspected sleep apnea, a sleep study is essential to diagnose the severity of the condition and to assess the need for surgical intervention for airway obstruction.
Pharyngoplasty surgery comes in several variations, depending on the specific needs and anatomy of the patient. Each type of pharyngoplasty aims to improve the function of the velopharyngeal mechanism, resulting in clearer speech and better airflow.
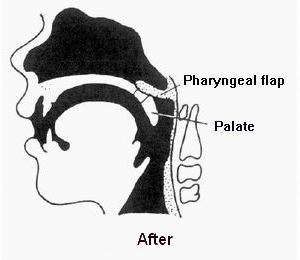
1. Pharyngeal Flap Surgery:
In pharyngeal flap surgery, a tissue flap from the posterior pharyngeal wall is attached to the soft palate, creating a more effective seal during speech. This method is commonly used to treat VPI in individuals with cleft palate or other congenital issues.
2. Sphincter Pharyngoplasty:
In sphincter pharyngoplasty, tissue from the tonsillar region is used to create a sphincter-like mechanism at the back of the throat. This helps improve the closure between the oral and nasal cavities during speech, reducing nasal air emission and improving speech resonance.
3. Lateral Pharyngoplasty:
Lateral pharyngoplasty is used to treat obstructive sleep apnea and involves surgical modifications to the lateral pharyngeal walls. This approach can help to prevent airway collapse during sleep by enhancing the structural integrity of the pharynx.
4. Injection Pharyngoplasty:
For less severe cases of VPI, injection pharyngoplasty can be an option. In this procedure, a substance like fat or collagen is injected into the soft palate to increase tissue bulk and improve closure. This is a minimally invasive procedure compared to more extensive surgeries.
5. Palatoplasty (Palatal Advancement Surgery):
In some cases, especially for individuals with cleft palate, the soft palate may need to be surgically repositioned or lengthened to improve its ability to close the velopharyngeal port. Palatoplasty is often performed in conjunction with other pharyngoplasty techniques.
While some conditions requiring pharyngoplasty are congenital and cannot be prevented, there are steps individuals can take to minimize the risk or severity of related problems:
-
Early Diagnosis: Identifying conditions like cleft palate or other speech disorders early in childhood can lead to early intervention, reducing the need for more extensive surgery later.
-
Speech Therapy: Children and adults experiencing speech issues related to velopharyngeal insufficiency should undergo speech therapy, which may delay or even prevent the need for surgery in some cases.
-
Regular Follow-ups: Individuals with known risk factors should maintain regular follow-up visits with an ENT specialist or speech-language pathologist to monitor speech and swallowing functions.
-
Healthy Lifestyle: For those with obstructive sleep apnea, maintaining a healthy weight and avoiding smoking or alcohol consumption can help manage symptoms and reduce the likelihood of surgical intervention.
As with any surgery, pharyngoplasty carries a risk of complications, both in the short and long term:
Short-term Risks:
-
Bleeding during or after surgery.
-
Infection at the surgical site.
-
Swelling and discomfort that may temporarily impair breathing or swallowing.
-
Pain following surgery, which is typically managed with pain medications.
Long-term Risks:
-
Persistent hypernasality or speech issues if the surgery does not adequately address the condition.
-
Scar tissue formation that may impact function.
-
Sleep-disordered breathing if the surgery does not fully correct airway obstruction.
-
Regrowth of tissue that may necessitate a follow-up procedure.
Following surgery, many individuals experience improved speech and breathing, leading to a better quality of life. However, living with the condition requires ongoing care:
-
Speech Therapy: Ongoing speech therapy is often essential to ensure that speech improves following surgery.
-
Regular Monitoring: Individuals should continue to follow up with their healthcare provider to ensure proper healing and that no new complications arise.
-
Lifestyle Adjustments: Those who underwent surgery for sleep apnea may need to adopt certain lifestyle changes, such as losing weight or using CPAP machines for optimal breathing during sleep.
1. What is pharyngoplasty?
Pharyngoplasty is a surgical procedure aimed at improving the function or appearance of the pharynx (the back part of the throat). It is often performed to treat issues like velopharyngeal insufficiency (VPI), speech difficulties, swallowing problems, or to reconstruct the pharynx following trauma or surgery.
2. Why is pharyngoplasty performed?
Pharyngoplasty is typically performed to address conditions such as speech disorders, particularly those caused by a cleft palate or velopharyngeal insufficiency, where the soft palate cannot close off the nasopharynx effectively. It can also be done to treat swallowing difficulties or improve the function of the airway.
3. How is pharyngoplasty performed?
The procedure involves modifying or reconstructing the pharyngeal muscles, soft palate, or the structures that aid in speech and swallowing. It may include tissue repositioning, muscle repair, or the insertion of a prosthesis to improve closure between the nasopharynx and the oral cavity. The surgery is typically done under general anesthesia.
4. Is pharyngoplasty painful?
The surgery is performed under general anesthesia, so patients do not feel pain during the procedure. After surgery, some discomfort, such as a sore throat or difficulty swallowing, is common but can be managed with pain medications.
5. What is the recovery time after pharyngoplasty?
Recovery time typically takes a few weeks. Swelling, throat discomfort, and difficulty swallowing are common during the first few days after surgery. Most patients can return to normal activities within 1 to 2 weeks, but full healing may take several months.
6. Are there any risks or complications associated with pharyngoplasty?
As with any surgical procedure, risks include infection, bleeding, scarring, and difficulty swallowing. In some cases, the changes to the pharynx may not fully resolve the speech or swallowing issues, and further treatment may be necessary.
7. How should I prepare for pharyngoplasty surgery?
Preparation involves a complete medical evaluation, including imaging studies like CT scans or MRIs to assess the pharyngeal structure. You may need to avoid eating or drinking for several hours before surgery and stop certain medications like blood thinners.
8. Will pharyngoplasty improve my speech?
In cases of velopharyngeal insufficiency or cleft palate-related speech disorders, pharyngoplasty can significantly improve speech by helping to create a more effective closure of the nasopharynx. This allows better air control and reduces hypernasality.
9. Can pharyngoplasty be repeated if necessary?
Yes, if the initial surgery does not fully address the issue or if there are complications, a secondary pharyngoplasty may be performed to further improve the function or appearance of the pharynx.
10. How can I ensure the best results from pharyngoplasty?
To ensure optimal results, it’s important to follow post-operative care instructions, including speech therapy or swallowing therapy, and attend follow-up appointments to monitor recovery. Maintaining a healthy lifestyle and avoiding smoking can also help promote healing.
The other ENT Procedures are:
Few Popular Hospitals for Pharyngoplasty are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Pharyngoplasty | Doctors For Pharyngoplasty | Cost For Pharyngoplasty | Treatment For Pharyngoplasty | Destinations For Pharyngoplasty | Risks Pharyngoplasty | Pharyngoplasty In India | Pharyngoplasty Recovery | Pharyngoplasty Information | Pharyngoplasty Thailand | Pharyngoplasty In Malaysia | Pharyngoplasty Abroad | Pharyngoplasty Overseas | Pharyngoplasty Low Cost | Pharyngoplasty In Singapore | Pharyngoplasty In Argentina | Surgery Pharyngoplasty | Pharyngoplasty In Singapore General Hospital | Pharyngoplasty In Apollo Hospitals | Soft Palate | Cleft Lip | Cleft Palate | Vpi | Velo Pharyngeal Incompetence | Pharyngoplasty In Florence Nightingale Hospital
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


