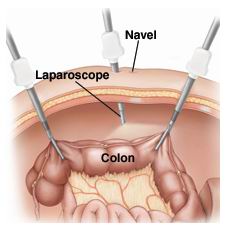
Laparoscopic colon surgery, often referred to as minimally invasive colon surgery, is a technique used by surgeons to treat various conditions affecting the colon (large intestine) and rectum, such as colorectal cancer, diverticulitis, inflammatory bowel disease (IBD), colonic polyps, and obstructions. This surgery is performed through small incisions (usually 3 to 5), using specialized tools such as a laparoscope (a long, flexible tube with a camera) to visualize the inside of the colon and the surrounding organs. Surgeons then use these small incisions to remove tumors, affected parts of the colon, or to correct other colon issues.
Laparoscopic surgery is preferred over traditional open surgery due to its numerous benefits. These benefits include smaller scars, reduced risk of infection, shorter hospital stays, and a faster recovery time. This has revolutionized the approach to colon surgery, enabling patients to return to their normal routines more quickly with less postoperative discomfort.
This surgery can be used for both diagnostic and therapeutic purposes. It allows surgeons to not only address the immediate issue, such as removing cancerous tissues or repairing obstructions, but also provides opportunities for precise staging of colorectal cancer, planning future treatments, and monitoring disease progression.
Laparoscopic colon surgery is performed for a variety of conditions that affect the colon. Understanding the causes and risk factors that lead to the need for this surgery is essential for both patients and healthcare providers.
Common Causes of Colon Problems Requiring Surgery:
-
Colorectal Cancer:
-
Colorectal cancer is one of the most common reasons for laparoscopic colon surgery. Tumors that develop in the colon or rectum may need to be surgically removed. Laparoscopy is preferred in early-stage cancers and for tumor resection to preserve the integrity of surrounding tissue.
-
-
Diverticulitis:
-
Diverticulitis occurs when small pouches (diverticula) in the colon become inflamed or infected. This can lead to severe pain, bleeding, and even perforation of the colon, making surgery necessary to remove the affected portion of the colon.
-
-
Inflammatory Bowel Disease (IBD):
-
Conditions like Crohn’s disease and ulcerative colitis are types of inflammatory bowel disease (IBD) that cause chronic inflammation in the colon. In some cases, when medical management is insufficient or complications arise, surgical intervention may be required to remove the affected portion of the colon.
-
-
Colon Obstruction:
-
Colon obstruction can be caused by tumors, scar tissue, hernias, or intussusception (where one part of the intestine slides into another). This can lead to severe discomfort and requires surgical intervention to relieve the blockage.
-
-
Colonic Perforation:
-
A perforation in the colon (a hole or tear) can occur due to trauma, infection, or other diseases. If untreated, it can lead to peritonitis (infection of the abdominal cavity), which requires emergency surgery.
-
-
Colon Polyps:
-
Colon polyps are abnormal growths that can develop on the lining of the colon. While most are benign, certain types can become cancerous over time. Surgical removal of the polyps is often necessary to prevent the development of cancer.
-
Risk Factors for Colon Problems:
-
Age:
-
The risk of developing colorectal conditions increases with age, particularly after the age of 50. Regular screening is important for early detection of colon cancer or other related issues.
-
-
Family History:
-
A family history of colorectal cancer or IBD can increase a person’s risk of developing similar conditions. People with a family history of these conditions may need to undergo more frequent screenings.
-
-
Diet and Lifestyle:
-
Diets high in red and processed meats and low in fiber are linked to an increased risk of colon cancer. Additionally, lack of physical activity, smoking, and heavy alcohol consumption can increase the risk of developing colon problems.
-
-
Obesity:
-
Obesity is a major risk factor for various gastrointestinal issues, including colon cancer and diverticulitis.
-
Laparoscopic colon surgery is typically performed when a patient presents with symptoms of colon-related conditions that require surgical intervention. Some of the symptoms associated with the need for colon surgery may include:
Symptoms Indicative of Conditions Requiring Laparoscopic Surgery:
-
Abdominal Pain and Cramping:
-
Persistent abdominal pain, cramping, and discomfort, especially in the lower abdomen, may be a sign of conditions like diverticulitis, colorectal cancer, or IBD, which may require surgical intervention.
-
-
Chronic Diarrhea or Constipation:
-
Patients with IBD, colon obstruction, or colon cancer often experience chronic diarrhea or constipation. These symptoms may not respond to medication and can significantly impact the patient's quality of life.
-
-
Rectal Bleeding or Blood in Stool:
-
Rectal bleeding or noticing blood in the stool is a common symptom of colorectal cancer, diverticulitis, or colon polyps. It requires immediate medical evaluation and may lead to the decision to perform laparoscopic colon surgery.
-
-
Unexplained Weight Loss:
-
Unintentional weight loss, particularly accompanied by other gastrointestinal symptoms like nausea, vomiting, or loss of appetite, may indicate the presence of colon cancer or another serious condition requiring surgery.
-
-
Bloating and Feeling of Fullness:
-
Abdominal bloating or a persistent feeling of fullness, especially after eating small amounts, can occur in patients with colon obstructions, IBD, or colorectal cancer.
-
-
Nausea and Vomiting:
-
Nausea and vomiting, particularly when associated with abdominal pain or bloating, may indicate a bowel obstruction or other gastrointestinal disorder that requires surgical treatment.
-
The diagnosis of conditions requiring laparoscopic colon surgery involves a combination of medical history review, physical examination, imaging tests, and diagnostic procedures to evaluate the underlying cause.
Diagnostic Tests:
-
Colonoscopy:
-
Colonoscopy is a crucial diagnostic tool used to visualize the inside of the colon and rectum. During this procedure, a long, flexible tube with a camera is inserted into the rectum, allowing the surgeon to observe polyps, tumors, inflammation, or other abnormalities.
-
-
CT Scan (Abdominal and Pelvic Imaging):
-
A CT scan is used to assess the colon and surrounding structures for tumors, obstructions, and signs of disease. It can also help evaluate the extent of inflammation in IBD or identify complications such as colon perforation or diverticulitis.
-
-
Barium Enema (X-ray):
-
A barium enema is an X-ray procedure that uses contrast material to outline the colon, helping to detect abnormalities such as polyps, diverticulosis, or tumors.
-
-
Blood Tests:
-
Blood tests may be used to assess the presence of infection, anemia (a sign of internal bleeding), or elevated tumor markers (such as CEA for colon cancer).
-
-
Endoscopy (for Gastric Concerns):
-
If the patient is also suspected to have gastric polyps or ulcers, gastroscopy (upper endoscopy) may be performed to visualize the stomach and upper part of the small intestine.
-
-
Biopsy:
-
During colonoscopy or endoscopy, if any suspicious tissue is detected, a biopsy may be performed to collect a sample for laboratory testing to confirm whether a growth is benign or cancerous.
-
Laparoscopic colon surgery is primarily a treatment for conditions that affect the colon and rectum, and the exact procedure depends on the underlying condition being treated.
Common Treatment Options:
-
Colon Resection (Partial or Total):
-
The most common surgical procedure is colon resection, where a portion of the colon is removed to treat cancer, diverticulitis, or other diseases. This may involve removing only a small segment of the colon or, in severe cases, the entire colon.
-
-
Colectomy (Total Removal of the Colon):
-
For certain conditions like colon cancer or severe IBD, a total colectomy may be necessary. This involves removing the entire colon and may be followed by the creation of an ileostomy (a surgical opening in the abdomen) to allow waste to exit the body.
-
-
Colostomy or Ileostomy Creation:
-
If a portion of the colon needs to be removed and reconnection is not possible, a colostomy or ileostomy may be created to allow stool to exit through an opening in the abdomen. This can be either permanent or temporary, depending on the condition.
-
-
Polypectomy:
-
For patients with colon polyps, a polypectomy may be performed during colonoscopy. If polyps are cancerous or precancerous, they will be removed during the procedure.
-
-
Bowel Resection with Anastomosis:
-
If part of the colon is removed, the remaining sections are often reconnected through a process called anastomosis. This can be done laparoscopically, minimizing recovery time.
-
-
Stoma Reversal:
-
If a stoma was created as part of the surgery (such as in the case of an ileostomy or colostomy), a stoma reversal may be performed later to reconnect the intestines.
-
Although laparoscopic colon surgery is effective for treating various colon conditions, prevention strategies can help reduce the need for surgery in the first place.
Prevention Strategies:
-
Routine Screening:
-
Regular colonoscopy screenings are essential for individuals over the age of 50 (or earlier for those with a family history of colorectal cancer). Early detection of polyps can prevent the need for more invasive surgeries.
-
-
Dietary Modifications:
-
A diet rich in fiber, fruits, vegetables, and whole grains can help prevent constipation and reduce the risk of developing colon cancer. Limiting processed meats and red meats is also recommended.
-
-
Regular Exercise:
-
Physical activity helps maintain healthy bowel function and reduces the risk of obesity, which is a significant risk factor for colon cancer.
-
-
Weight Management:
-
Maintaining a healthy weight can reduce the risk of developing gastrointestinal issues, including colon cancer and diverticulitis.
-
-
Smoking Cessation and Limiting Alcohol Intake:
-
Quitting smoking and moderating alcohol intake can lower the risk of developing colorectal cancer.
-
While laparoscopic colon surgery is generally safe,
there are potential risks and complications that patients should be aware of:
-
Infection:
-
Infection can occur at the site of the incisions or internally in the abdominal cavity. Proper post-surgical care and antibiotic therapy help minimize this risk.
-
-
Bleeding:
-
Some degree of bleeding is common after surgery, but in rare cases, excessive bleeding may require additional intervention.
-
-
Bowel Obstruction:
-
Post-surgical adhesions (scar tissue) can cause bowel obstructions, which may require further treatment or surgery.
-
-
Perforation:
-
Although rare, perforation of the colon can occur during surgery, leading to peritonitis (infection of the abdominal cavity), which requires immediate treatment.
-
-
Anastomotic Leak:
-
If the colon sections are reconnected, there is a small risk that the anastomosis (surgical join) could leak, leading to infection or other complications.
-
After laparoscopic colon surgery, patients typically need to adjust to changes in their diet, lifestyle, and overall health. Recovery can vary, but most patients experience quicker healing times compared to traditional open surgery.
Post-Surgery Care and Lifestyle Adjustments:
-
Post-Surgical Recovery:
-
Patients will need to rest and follow their surgeon’s recommendations for wound care, pain management, and activity restrictions. Most people are able to return to normal activities within a few weeks.
-
-
Dietary Changes:
-
A high-fiber diet is encouraged to promote healthy digestion and bowel function after surgery. Small, frequent meals may be recommended initially as the digestive system recovers.
-
-
Follow-up Care:
-
Regular follow-up appointments with the surgeon are important to monitor recovery, check for complications, and evaluate the patient’s progress in terms of diet, weight management, and bowel function.
-
-
Psychosocial Support:
-
Support groups or counseling may be helpful for patients who have undergone major gastrointestinal surgery, particularly if the surgery impacts their lifestyle or body image.
-
1. What is laparoscopic colon surgery?
Laparoscopic colon surgery, also known as minimally invasive colon surgery, involves the use of small incisions and a laparoscope (a thin tube with a camera and light) to perform colon surgery. The surgeon views the colon on a video screen and uses specialized instruments to remove or repair sections of the colon. This method is typically used for conditions like colon cancer, diverticulitis, and inflammatory bowel disease (IBD).
2. Why is laparoscopic colon surgery performed?
Laparoscopic colon surgery is often performed for the treatment of conditions such as:
-
Colon cancer: To remove cancerous sections of the colon.
-
Diverticulitis: Inflammation or infection of pouches in the colon.
-
Inflammatory bowel disease (IBD): Conditions like Crohn’s disease or ulcerative colitis that damage the colon.
-
Colon obstructions: Caused by tumors, scar tissue, or other blockages.
The goal of the surgery is to remove the diseased portion of the colon while preserving as much healthy tissue as possible.
3. How is laparoscopic colon surgery performed?
The procedure is done under general anesthesia. The surgeon makes small incisions in the abdomen, through which the laparoscope and specialized instruments are inserted. The surgeon uses the camera to view the colon and performs the surgery by removing the damaged portion and reattaching the healthy sections. In some cases, part of the colon may be temporarily diverted through a colostomy bag.
4. Is laparoscopic colon surgery painful?
The surgery is performed under anesthesia, so there is no pain during the procedure. Afterward, patients may experience mild to moderate discomfort or soreness in the abdomen, as well as bloating or gas. Pain is typically managed with medications and subsides within a few days.
5. How long does laparoscopic colon surgery take?
The surgery usually takes between 2 to 4 hours, depending on the extent of the surgery, the location of the problem in the colon, and the patient's overall health.
6. What is the recovery time after laparoscopic colon surgery?
Recovery time varies from patient to patient, but most individuals can leave the hospital in 2 to 3 days after surgery. Full recovery typically takes 4 to 6 weeks, during which time patients may need to avoid heavy lifting and strenuous activities. Most people can return to normal activities within 1 to 2 weeks, depending on their recovery progress.
7. What are the risks or complications of laparoscopic colon surgery?
As with any surgery, risks include infection, bleeding, blood clots, injury to surrounding organs, or leakage from the site where the colon is reconnected. However, laparoscopic surgery typically has fewer complications compared to traditional open surgery because of the smaller incisions and less trauma to surrounding tissue.
8. How should I prepare for laparoscopic colon surgery?
Preparation includes a thorough medical evaluation, including blood tests, imaging studies (such as CT scans or colonoscopy), and bowel preparation (such as fasting and cleansing the intestines). You may be asked to stop taking certain medications, like blood thinners, before the surgery. You should also arrange for someone to drive you home after the procedure.
9. What should I expect after laparoscopic colon surgery?
After surgery, you may experience discomfort or bloating, and you will be monitored closely for signs of complications, such as infection or bleeding. You may be given fluids through an IV initially, followed by a gradual reintroduction of solid foods. A special diet may be recommended during the recovery period. You will also need follow-up appointments to monitor healing and check for any complications.
10. Will I need a colostomy after laparoscopic colon surgery?
In most cases, a colostomy is not necessary, as the surgeon typically reconnects the healthy sections of the colon. However, in cases where the colon cannot be safely reconnected, a temporary or permanent colostomy may be required. Your surgeon will discuss this with you beforehand if it is a possibility.
The other Gastro procedures are
Few Major Hospitals for Laparoscopic colon surgery are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Laparoscopic Colon Surgery | Doctors For Laparoscopic Colon Surgery | Surgery Laparoscopic Colon Surgery | Cost Laparoscopic Colon Surgery | Treatment Laparoscopic Colon Surgery | Destinations Laparoscopic Colon Surgery | Risks Laparoscopic Colon Surgery | Laparoscopic Colon Surgery In India | Laparoscopic Colon Surgery Recovery | Laparoscopic Colon Surgery Information | Laparoscopic Colon Surgery Thailand | Laparoscopic Colon Surgery In Malaysia | Laparoscopic Colon Surgery Abroad | Laparoscopic Colon Surgery Donors | Laparoscopic Colon Surgery Overseas | Laparoscopic Colon Surgery Low Cost | Laparoscopic Colon Surgery In Singapore | Laparoscopic Colon Surgery In Argentina | Large Intestine | Colon | Abdominal Cavity | Colonoscopy | Barium Enema Tests
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


