Laparoscopic duodenal closure is a surgical procedure used to close perforations, treat ulcers, and address other significant complications within the duodenum. The duodenum is a vital part of the digestive system that receives partially digested food from the stomach and aids in nutrient absorption. However, when the duodenum is compromised by disease, trauma, or infection, the result can be a perforation, which can lead to life-threatening conditions like peritonitis (infection of the abdominal cavity).
Laparoscopic surgery is preferred over traditional open surgery because it is minimally invasive, requiring only a few small incisions rather than a large abdominal incision. This technique significantly reduces recovery time, postoperative pain, and complications.
How Laparoscopic Duodenal Closure Works
-
Small Incisions: The surgeon creates a few small incisions, typically about 0.5 to 1.5 cm, in the abdominal wall.
-
Insertion of Laparoscope: A laparoscope (a flexible tube with a light and camera) is inserted through one of the incisions. This device allows the surgeon to view the inside of the duodenum and surrounding organs on a monitor.
-
Closing the Perforation: Specialized surgical tools are used to repair the perforation in the duodenum. Depending on the size and location of the hole, the surgeon may use sutures, staples, or other techniques to close the perforation.
-
Restoration of Function: Once the perforation is closed, the surgeon will ensure that there are no other complications and that the duodenum is functioning properly. The remaining healthy sections of the duodenum may also be reconnected (anastomosis) if a significant portion was removed.
-
Post-Operative Care: After the procedure, patients are monitored in the hospital for a few days before being sent home with instructions for recovery and follow-up care.
The laparoscopic approach is favored for its ability to offer precise closure of the duodenal perforation with minimal damage to surrounding tissues, reduced blood loss, and a quicker recovery time compared to traditional open surgery.
The primary reason for laparoscopic duodenal closure is the presence of duodenal perforation. The duodenum can become compromised due to various underlying conditions, each with its own causes and risk factors.
Causes of Duodenal Perforation and Ulceration
-
Peptic Ulcers:
-
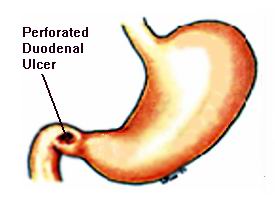
Peptic ulcers are the most common cause of duodenal perforations. These ulcers are open sores that develop on the lining of the duodenum, often due to Helicobacter pylori infection or the prolonged use of NSAIDs (nonsteroidal anti-inflammatory drugs). When left untreated, ulcers can erode deeper into the duodenal wall, leading to perforation.
-
-
Duodenal Cancer:
-
Duodenal cancer, although rare, can lead to perforation if the tumor erodes through the intestinal wall. Surgery may be necessary to remove the cancerous tissue and repair the perforated area.
-
-
Trauma or Injury:
-
Physical trauma to the abdomen, such as from accidents or blunt force injuries, can result in damage to the duodenum. This may lead to a perforation that requires surgical intervention to prevent infection or further complications.
-
-
Inflammatory Bowel Disease (IBD):
-
Conditions like Crohn’s disease or ulcerative colitis cause chronic inflammation in the gastrointestinal tract, including the duodenum. In some cases, this inflammation can lead to ulcers or perforations.
-
-
Infections:
-
Certain infections in the abdominal area can result in duodenal damage, which may lead to perforation if left untreated.
-
-
Surgical Complications:
-
In some cases, prior surgeries, particularly those involving the stomach or intestines, may lead to complications such as anastomotic leaks, perforations, or fistulas, requiring closure procedures.
-
Risk Factors for Duodenal Perforations and Ulcers
Several factors increase the risk of developing duodenal perforations or ulcers:
-
Helicobacter pylori infection: This bacterial infection is a leading cause of peptic ulcers, which can lead to perforations if untreated.
-
Long-term use of NSAIDs: Regular or excessive use of pain-relieving medications such as aspirin or ibuprofen can increase the risk of duodenal ulcers.
-
Cigarette smoking: Smoking weakens the protective lining of the stomach and duodenum, making it more susceptible to ulcer formation.
-
Excessive alcohol consumption: Alcohol can irritate the duodenal lining and contribute to the development of ulcers.
-
Stress: Although stress does not directly cause ulcers, it can exacerbate symptoms and delay healing.
-
Chronic use of corticosteroids: Long-term use of corticosteroid medications can increase the likelihood of developing ulcers in the gastrointestinal tract.
Symptoms that may lead to the need for laparoscopic duodenal closure are often related to duodenal ulcers or perforations. These conditions can cause the following:
Symptoms of Duodenal Perforation or Ulceration
-
Severe Abdominal Pain:
-
Intense, sharp pain, often localized in the upper abdomen, is the hallmark symptom of a duodenal ulcer or perforation. The pain may worsen after eating or when the stomach is empty.
-
-
Nausea and Vomiting:
-
Persistent nausea, sometimes accompanied by vomiting, is a common symptom, particularly in cases of duodenal perforation or obstruction.
-
-
Bloating and Abdominal Distension:
-
A swollen, bloated abdomen can occur, especially if there is a perforation, as digestive contents leak into the peritoneal cavity.
-
-
Rectal Bleeding:
-
Black, tarry stools or visible blood in the stool can indicate gastrointestinal bleeding due to an ulcer or perforation.
-
-
Fever:
-
Fever, often accompanied by chills, may indicate an infection caused by a perforation in the duodenum, which can lead to peritonitis.
-
-
Fatigue and Weakness:
-
Chronic blood loss from ulcers can lead to anemia, causing fatigue, weakness, and pallor.
-
-
Loss of Appetite:
-
A diminished appetite, often due to pain or discomfort while eating, is a common sign of duodenal problems.
-
When to Seek Medical Attention
If you experience severe abdominal pain, black stools, vomiting blood, or persistent nausea, seek immediate medical attention. A duodenal perforation can be a medical emergency that requires prompt surgical intervention.
Before undergoing laparoscopic duodenal closure, a series of diagnostic tests are typically performed to confirm the presence of duodenal perforations or ulcers.
Diagnostic Tests for Duodenal Conditions
-
Physical Examination:
-
A thorough physical exam is performed to assess the patient's abdominal tenderness, bloating, and any signs of peritonitis.
-
-
Endoscopy:
-
Upper Endoscopy (Gastroscopy): An upper endoscopy allows direct visualization of the duodenum to identify ulcers, perforations, or inflammation. Biopsies can also be taken during this procedure to test for infections or cancer.
-
-
Imaging Tests:
-
CT Scan: A CT scan of the abdomen is commonly used to identify duodenal perforations, abscesses, and fluid collections within the abdominal cavity.
-
X-ray: An abdominal X-ray can show free air in the abdomen, which is often a sign of a perforated duodenal ulcer.
-
MRI: MRI can provide detailed images of the duodenum and surrounding tissues, especially in patients with complex conditions like Crohn’s disease.
-
-
Blood Tests:
-
Blood tests can detect signs of infection (elevated white blood cells), anemia (low red blood cells), and dehydration due to vomiting and fluid loss.
-
-
Barium Swallow or Enema:
-
A barium swallow or enema may be used to help identify abnormalities in the duodenum or any areas that are not functioning properly.
-
Laparoscopic duodenal closure is the primary treatment for repairing perforations or ulcers in the duodenum. However, there are other treatments that may be used in conjunction with or prior to surgery.
Laparoscopic Duodenal Closure Procedure
-
Resection and Closure:
-
If a perforation is present, the surgeon will repair it by suturing or stapling the hole closed. The goal is to prevent further leakage of digestive contents into the abdominal cavity.
-
-
Anastomosis:
-
If a portion of the duodenum needs to be removed due to ulceration or cancer, the remaining healthy parts of the duodenum are reconnected through a process called anastomosis.
-
-
Temporary Stoma:
-
In cases where the duodenum cannot be safely reconnected, a temporary colostomy or ileostomy may be performed. This creates an opening through the abdominal wall where stool is collected in a bag until the intestine has healed.
-
-
Drainage:
-
In cases of abscesses or fluid accumulation, a drain may be inserted to remove the infected fluid and prevent further complications.
-
Non-Surgical Treatment Options
-
Medications:
-
Proton Pump Inhibitors (PPIs): To reduce stomach acid and promote healing of ulcers.
-
Antibiotics: To treat infections, particularly in cases of perforations or infected ulcers.
-
Antacids: To neutralize stomach acid and reduce irritation.
-
-
Dietary Changes:
-
For patients with duodenal ulcers, a bland, low-acid diet may be recommended to reduce irritation in the digestive tract and promote healing.
-
While
some conditions may not be preventable, adopting a healthy lifestyle and following medical advice can reduce the risk of duodenal perforations and other related complications.
Preventive Measures
-
Helicobacter pylori Eradication:
-
Treating H. pylori infection with a full course of antibiotics can reduce the risk of ulcers and perforations.
-
-
Avoid Long-Term Use of NSAIDs:
-
Limiting the use of NSAIDs can help prevent damage to the duodenal lining and reduce the risk of ulcers.
-
-
Healthy Lifestyle:
-
Quitting smoking, limiting alcohol consumption, and eating a balanced diet rich in fruits, vegetables, and fiber can help prevent gastrointestinal issues.
-
-
Stress Management:
-
While stress does not directly cause ulcers, it can exacerbate symptoms. Practicing relaxation techniques like meditation or yoga can help reduce stress.
-
Post-Surgery Management
-
Regular Follow-Ups:
-
After surgery, follow-up visits are essential to ensure proper healing and to detect any recurrence of ulcers or perforations.
-
-
Dietary Modifications:
-
Gradual introduction of solid foods is necessary post-surgery. Patients may need to follow a special diet for several weeks to ensure healing.
-
-
Physical Activity:
-
Gentle physical activity, like walking, can help improve circulation and prevent complications such as blood clots during recovery.
-
Though laparoscopic duodenal closure is considered a safe and effective treatment, there are potential complications to be aware of:
-
Infection:
-
Infection at the surgical site or in the abdominal cavity can occur, especially if there was a perforation or abscess before surgery.
-
-
Bleeding:
-
There is a risk of bleeding during or after the procedure, particularly if blood vessels are damaged during surgery.
-
-
Leakage at the Reconnection Site:
-
A rare but serious complication where the reconnection of the duodenum leaks, which can lead to further complications like peritonitis.
-
-
Scar Tissue Formation (Adhesions):
-
Scar tissue can develop after surgery, which may cause a blockage or discomfort in the intestines.
-
After laparoscopic duodenal closure, patients will need to make certain lifestyle adjustments to ensure a smooth recovery and prevent future complications.
Dietary Adjustments:
-
Patients will need to avoid spicy, fatty, or acidic foods and focus on easily digestible, nutrient-dense meals to promote healing.
Regular Exercise:
-
Once cleared by a healthcare provider, incorporating light physical activity into daily routines can aid in recovery and help prevent complications.
Ongoing Medical Care:
-
Regular check-ups and follow-up appointments are essential to monitor the success of the surgery and detect any potential issues early on.
1. What is laparoscopic duodenal closure?
Laparoscopic duodenal closure is a minimally invasive surgical procedure where the duodenum (the first part of the small intestine) is closed, usually to treat perforations, ulcers, or other conditions causing damage. The surgery involves using a laparoscope, a small camera inserted through tiny incisions in the abdomen, to view and repair the duodenum.
2. Why is laparoscopic duodenal closure performed?
This procedure is performed to treat perforations or ulcers in the duodenum caused by conditions such as peptic ulcers, trauma, or certain diseases like Crohn’s disease. It helps prevent further damage, infection, and complications, and restores the function of the duodenum.
3. How is laparoscopic duodenal closure performed?
The surgery is performed under general anesthesia. Small incisions are made in the abdomen, and a laparoscope (a long, flexible tube with a light and camera) is inserted to view the duodenum. Specialized instruments are used to close the perforation or ulcer, often using sutures or staplers. The surgeon uses the laparoscope to guide the procedure with high precision.
4. Is laparoscopic duodenal closure painful?
The surgery is performed under general anesthesia, so there is no pain during the procedure. After surgery, patients may experience mild discomfort, abdominal pain, and bloating, but this is typically well-managed with pain medications. The pain usually subsides within a few days to weeks.
5. How long does laparoscopic duodenal closure take?
The procedure typically takes between 1 to 2 hours, depending on the complexity of the case and the location of the perforation or ulcer.
6. What is the recovery time after laparoscopic duodenal closure?
Recovery time varies but generally takes 1 to 2 weeks for the initial healing phase. Most patients can return to normal activities within 2 to 4 weeks. However, it may take a few months for the duodenum to heal completely. Patients are often advised to follow a special diet and avoid heavy lifting for the first few weeks.
7. What are the risks or complications of laparoscopic duodenal closure?
As with any surgery, risks include infection, bleeding, injury to surrounding organs, and complications related to anesthesia. In rare cases, the duodenum may not heal properly, or the closure may reopen, requiring further treatment. However, laparoscopic surgery typically results in fewer complications than traditional open surgery.
8. How should I prepare for laparoscopic duodenal closure surgery?
Preparation includes fasting for several hours before the surgery, undergoing imaging tests such as X-rays or CT scans, and stopping certain medications like blood thinners. Your doctor will provide specific instructions on how to prepare and what to expect before the surgery.
9. What should I expect after laparoscopic duodenal closure surgery?
After surgery, you will be monitored in a recovery room for a short period. You may experience mild discomfort, bloating, and a sore throat from the anesthesia tube. You will be encouraged to gradually resume eating and drinking, starting with liquids. Your doctor will provide instructions on diet and activity restrictions during the recovery period.
10. Can laparoscopic duodenal closure be repeated if necessary?
In some cases, further surgery may be needed if the perforation or ulcer recurs, or if complications develop. However, laparoscopic duodenal closure is highly effective in treating duodenal issues, and with proper post-operative care, most patients experience long-term success. If complications occur, your doctor will evaluate the best course of action.
The other Gastro procedures are:
Few Major Hospitals for Laparoscopic Duodenal Closure are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Laparoscopic Duodenal Closure | Doctors For Laparoscopic Duodenal Closure | Surgery Laparoscopic Duodenal Closure | Cost Laparoscopic Duodenal Closure | Treatment Laparoscopic Duodenal Closure | Destinations Laparoscopic Duodenal Closure | Risks Laparoscopic Duodenal Closure | Laparoscopic Duodenal Closure In India | Laparoscopic Duodenal Closure Recovery | Laparoscopic Duodenal Closure Information | Laparoscopic Duodenal Closure Thailand | Laparoscopic Duodenal Closure In Malaysia | Laparoscopic Duodenal Closure Abroad | Laparoscopic Duodenal Closure Donors | Laparoscopic Duodenal Closure Overseas | Laparoscopic Duodenal Closure Low Cost | Laparoscopic Duodenal Closure In Singapore | Laparoscopic Duodenal Closure In Argentina | Duodenal Perforation | Duodenal Ulcer | Perforated Duodenal Ulcer | Graham Patch | Omental Patch | Surgical Emergency
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


