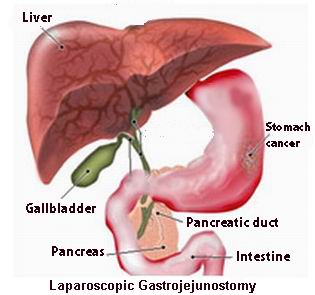
Laparoscopic Gastrojejunostomy (LGJ) is a minimally invasive surgical procedure that creates a bypass between the stomach and the jejunum (the middle part of the small intestine) to treat a variety of gastrointestinal conditions. This procedure is most commonly performed in cases where there is a blockage or obstruction in the duodenum (the first part of the small intestine) that prevents the normal passage of food and fluids from the stomach. By rerouting food from the stomach directly to the jejunum, this surgery allows for continued digestion, alleviating symptoms such as vomiting, malnutrition, and weight loss.
Laparoscopic gastrojejunostomy is performed using laparoscopic (keyhole) surgery, which involves making small incisions in the abdomen through which a camera and specialized instruments are inserted. This approach offers significant benefits over traditional open surgery, including smaller incisions, less postoperative pain, shorter hospital stays, and a faster recovery time.
The surgery is primarily indicated for patients with gastric outlet obstruction, gastric cancer, benign duodenal obstructions, or conditions that cause severe peptic ulcers. It may also be used in bariatric surgery to assist with weight loss by redirecting food intake.
Laparoscopic gastrojejunostomy is typically performed in patients suffering from diseases or conditions that cause blockages or dysfunction in the upper part of the digestive system, primarily the stomach and duodenum. Understanding the causes and risk factors for these conditions is key to identifying who may benefit from this procedure.
Common Causes Leading to Laparoscopic Gastrojejunostomy:
-
Gastric Outlet Obstruction:
-
The most common reason for performing gastrojejunostomy is a gastric outlet obstruction. This occurs when there is a blockage or narrowing in the pylorus (the opening between the stomach and duodenum), often due to benign or malignant tumors, ulcerations, or scarring. This obstruction can lead to symptoms such as nausea, vomiting, and weight loss, and surgery is often necessary to bypass the blockage.
-
-
Peptic Ulcer Disease:
-
Chronic peptic ulcers, particularly in the duodenum, can lead to the formation of strictures (narrowing) that cause gastric outlet obstruction. In severe cases, gastrojejunostomy can be used to bypass the damaged part of the gastrointestinal tract and provide relief.
-
-
Gastric Cancer:
-
Gastric cancer or adenocarcinoma of the stomach is another common indication for gastrojejunostomy. As the cancer progresses, it can block the pyloric channel or duodenum, making it difficult for food to pass through. Gastrojejunostomy is performed to bypass the tumor and restore normal digestion.
-
-
Bariatric Surgery (Weight Loss Surgery):
-
In some cases, gastric bypass or other bariatric surgeries may involve creating a gastrojejunostomy to aid in weight loss by restricting food intake and promoting malabsorption. This helps individuals with severe obesity achieve significant weight loss and improve their overall health.
-
-
Crohn’s Disease:
-
Crohn’s disease, a type of inflammatory bowel disease (IBD), can cause severe inflammation and scarring in the small intestine, leading to obstructions. When medical treatment fails, a gastrojejunostomy may be necessary to bypass the affected portion of the digestive tract.
-
Risk Factors for Conditions Requiring Gastrojejunostomy:
-
Age:
-
Older adults are more prone to developing gastric cancer, peptic ulcers, and other gastrointestinal conditions that may lead to the need for a gastrojejunostomy.
-
-
Smoking:
-
Smoking is a major risk factor for the development of peptic ulcers, gastric cancer, and other gastrointestinal issues. It also impairs the healing process after surgery.
-
-
Chronic Alcohol Use:
-
Excessive alcohol consumption is a risk factor for gastric ulcers, gastritis, and gastric cancer. Chronic alcohol use can contribute to inflammation and damage to the stomach lining, leading to obstruction.
-
-
Family History:
-
A family history of gastric cancer, ulcerative colitis, or Crohn’s disease can increase an individual’s risk of developing conditions that may require surgical intervention.
-
-
Diet:
-
A diet rich in processed meats, low in fiber, and high in salt can contribute to the development of gastric cancer and peptic ulcers, both of which may require gastrojejunostomy.
-
The conditions that necessitate a laparoscopic gastrojejunostomy typically present with gastrointestinal symptoms that interfere with digestion and nutrition. These symptoms can range from mild to severe, and surgery is often needed when conservative treatments do not provide adequate relief.
Common Symptoms Indicating the Need for Gastrojejunostomy:
-
Severe Abdominal Pain:
-
Patients may experience severe abdominal discomfort or cramping, especially after eating, due to gastric outlet obstruction or ulceration in the upper gastrointestinal tract.
-
-
Nausea and Vomiting:
-
One of the hallmark signs of gastric outlet obstruction is persistent nausea and vomiting. This occurs when food cannot pass through the stomach and into the intestines due to a blockage.
-
-
Bloating and Fullness:
-
A feeling of fullness or bloating after eating even small amounts of food is common. This can be particularly noticeable in patients with gastric cancer or duodenal ulcers, where the pyloric valve is obstructed.
-
-
Weight Loss:
-
Unintended weight loss is often associated with conditions like gastric cancer and peptic ulcers, especially when the patient is unable to eat properly or experiences difficulty with digestion and nutrient absorption.
-
-
Poor Appetite:
-
Loss of appetite, especially in patients with gastric cancer or chronic gastrointestinal conditions like Crohn’s disease, is common. This can lead to nutritional deficiencies and further exacerbates weight loss.
-
-
Anemia:
-
Chronic bleeding from ulcers or tumors can lead to iron-deficiency anemia, causing fatigue, weakness, and pallor. This is often a sign of an underlying gastrointestinal issue that may require surgical treatment.
-
The diagnosis for laparoscopic gastrojejunostomy involves evaluating the patient’s medical history, conducting a thorough physical examination, and using imaging and diagnostic tests to assess the underlying condition affecting the colon and stomach.
Diagnostic Procedures:
-
Endoscopy:
-
Endoscopy is often the first step in diagnosing conditions like gastric cancer or peptic ulcers. A flexible tube with a camera (endoscope) is inserted through the mouth to visually inspect the stomach and duodenum. Biopsy samples may also be taken during this procedure to assess the presence of cancer or other abnormalities.
-
-
Barium Swallow X-ray:
-
A barium swallow X-ray is often used to assess the swallowing function and gastric outlet obstruction. The patient swallows a contrast material (barium), which shows up on X-rays, allowing the physician to evaluate the passage of food through the gastrointestinal tract.
-
-
CT Scan:
-
A CT scan of the abdomen provides detailed images of the gastrointestinal tract and surrounding organs. It is used to assess the extent of an obstruction, tumor, or inflammation and to determine whether laparoscopic gastrojejunostomy is necessary.
-
-
Ultrasound:
-
Abdominal ultrasound may be used to evaluate the presence of any masses, fluid collections, or obstructions in the stomach and intestines. It can also help guide decision-making in patients with suspected gastric cancer or gastrointestinal inflammation.
-
-
Blood Tests:
-
Blood tests can help detect anemia (which may indicate bleeding from ulcers), infections, electrolyte imbalances, or tumor markers such as CEA (carcinoembryonic antigen) for colon cancer. Elevated levels of these markers can indicate the presence of malignancy.
-
Laparoscopic gastrojejunostomy is a surgical solution to bypass gastric outlet obstructions or other conditions that affect digestion and absorption in the upper gastrointestinal tract. Treatment typically involves removing or bypassing the obstruction and creating a new pathway for food to pass from the stomach to the jejunum.
Treatment Methods:
-
Gastrojejunostomy (Bypass Surgery):
-
The primary goal of laparoscopic gastrojejunostomy is to create a bypass between the stomach and the jejunum. The surgeon makes a small incision and connects the stomach to the small intestine, bypassing the obstructed area. This procedure restores normal digestion and alleviates symptoms of gastric outlet obstruction.
-
-
Gastrectomy with Gastrojejunostomy:
-
In cases of gastric cancer or extensive ulceration, a partial gastrectomy (removal of part of the stomach) may be necessary, followed by a gastrojejunostomy to ensure food can still pass through the digestive system.
-
-
Endoscopic Stent Placement:
-
In some cases, a stent (a small tube) can be placed in the stomach or duodenum to hold open an obstructed area. This can provide temporary relief before surgery, particularly in patients with gastric cancer.
-
-
Bariatric Surgery:
-
In bariatric surgery (weight-loss surgery), a gastrojejunostomy may be part of a procedure such as gastric bypass. This surgery reduces the stomach size and reroutes food to the jejunum to promote weight loss and improve metabolic health.
-
While gastrojejunostomy is often performed to treat underlying conditions, there are preventive measures and post-operative management strategies that can help optimize recovery and reduce complications.
Prevention Strategies:
-
Regular Screenings for Gastric Cancer:
-
For individuals at high risk of gastric cancer, such as those with a family history or previous peptic ulcers, regular screening (including endoscopy) is crucial for early detection and prevention of advanced disease.
-
-
Healthy Diet and Lifestyle:
-
A diet rich in fruits, vegetables, whole grains, and lean proteins can help prevent peptic ulcers, obesity, and other gastrointestinal issues. Limiting alcohol and avoiding smoking are key factors in maintaining a healthy digestive system.
-
-
Manage Underlying Conditions:
-
IBD, Crohn’s disease, and other chronic conditions should be well-managed with medication, regular check-ups, and lifestyle changes to prevent complications such as strictures and obstructions.
-
As with any surgery, laparoscopic gastrojejunostomy carries potential risks and complications that need to be addressed promptly.
Possible Complications:
-
Infection:
-
Infection at the surgical site is a risk with any invasive surgery. It can be minimized with proper sterile techniques and post-surgical care, including antibiotic therapy.
-
-
Bowel Obstruction:
-
Adhesions (scar tissue) may form after surgery, leading to intestinal obstruction. This can cause symptoms like pain, bloating, and vomiting, requiring further treatment or surgery.
-
-
Anastomotic Leak:
-
An anastomotic leak, where the new connection between the stomach and jejunum fails, can lead to leakage of stomach contents into the abdomen, resulting in infection or peritonitis.
-
-
Nutritional Deficiencies:
-
Because this surgery alters the normal digestive process, patients may have trouble absorbing nutrients, especially vitamins and minerals. Nutritional supplements may be required post-surgery.
-
Post-surgery, patients need to adjust their diet, lifestyle, and follow-up care to ensure successful recovery and prevent complications.
Post-Operative Care:
-
Dietary Changes:
-
Initially, patients may need to follow a liquid diet before transitioning to soft foods and eventually a regular diet. It is crucial to eat smaller meals and focus on nutrient-dense foods to prevent nutritional deficiencies.
-
-
Hydration and Nutritional Supplements:
-
Patients are advised to stay hydrated and take nutritional supplements (such as iron, calcium, and B vitamins) to prevent deficiencies due to altered nutrient absorption.
-
-
Follow-up Appointments:
-
Regular follow-up appointments with the surgeon are necessary to monitor healing, check for complications, and assess the patient's nutritional status.
-
-
Long-Term Lifestyle Modifications:
-
Maintaining a healthy weight, engaging in physical activity, and avoiding smoking and excessive alcohol are crucial for long-term health after surgery. Patients should adhere to their doctor’s advice regarding lifestyle and dietary modifications to improve recovery outcomes.
-
1. What is laparoscopic gastrojejunostomy?
Laparoscopic gastrojejunostomy is a minimally invasive surgical procedure in which a connection is made between the stomach and the jejunum (the second part of the small intestine). This procedure is used to bypass an obstructed or diseased portion of the stomach or duodenum, allowing food to pass from the stomach into the small intestine.
2. Why is laparoscopic gastrojejunostomy performed?
It is typically performed to treat conditions such as:
-
Peptic ulcers or gastric cancer that cause obstruction in the stomach or duodenum.
-
Chronic pancreatitis or pancreatic cancer that affects the duodenum.
-
Gastroparesis, a condition where the stomach does not empty properly.
The goal of the surgery is to restore normal digestive function by creating an alternative pathway for food.
3. How is laparoscopic gastrojejunostomy performed?
The procedure is done under general anesthesia. The surgeon makes small incisions in the abdomen through which a laparoscope (a long, flexible tube with a camera) is inserted. Specialized instruments are then used to create a bypass between the stomach and the jejunum, allowing food to pass directly into the small intestine.
4. Is laparoscopic gastrojejunostomy painful?
The procedure itself is painless since the patient is under general anesthesia. After the surgery, patients may experience mild to moderate abdominal discomfort, bloating, or gas, but these symptoms are usually managed with pain medication and subside within a few days.
5. How long does the surgery take?
Laparoscopic gastrojejunostomy typically takes about 2 to 3 hours, depending on the complexity of the case, the patient's health, and the surgeon’s experience.
6. What is the recovery time after laparoscopic gastrojejunostomy?
Recovery time varies, but most patients are able to leave the hospital within 3 to 5 days. Full recovery typically takes about 4 to 6 weeks. During the first few days after surgery, you will be encouraged to gradually increase your activity level and follow a special diet to promote healing.
7. What are the risks or complications of laparoscopic gastrojejunostomy?
As with any surgery, risks include infection, bleeding, leakage from the surgical site, injury to surrounding organs, or complications from anesthesia. These risks are minimal with laparoscopic techniques compared to traditional open surgery, but proper post-operative care is essential for optimal healing.
8. How should I prepare for laparoscopic gastrojejunostomy?
Preparation typically involves fasting for several hours before surgery, a thorough medical evaluation, and possibly bowel preparation (such as laxatives or enemas). You may need to stop taking certain medications, like blood thinners, before the procedure. Your surgeon will provide specific instructions.
9. What should I expect after laparoscopic gastrojejunostomy?
After surgery, you will be monitored in the recovery room and gradually reintroduced to liquids and then solid foods. You may experience mild abdominal discomfort, bloating, or nausea, which can be managed with medication. It’s essential to follow the post-operative care instructions, including dietary changes, to ensure a smooth recovery.
10. Will I be able to eat normally after laparoscopic gastrojejunostomy?
Initially, you will need to follow a liquid or soft food diet to give your body time to adjust to the new digestive pathway. Gradually, you will be able to return to solid foods, but you may need to make dietary adjustments, such as eating smaller, more frequent meals. Your doctor will provide guidance on the best foods to eat post-surgery.
The other Gastro procedures are:
Few major hospitals for Laparoscopy Gastrojejunostomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Laparoscopic Gastrojejunostomy | Doctors For Laparoscopic Gastrojejunostomy | Surgery Laparoscopic Gastrojejunostomy | Cost Laparoscopic Gastrojejunostomy | Treatment Laparoscopic Gastrojejunostomy | Destinations Laparoscopic Gastrojejunostomy | Risks Laparoscopic Gastrojejunostomy | Laparoscopic Gastrojejunostomy In India | Laparoscopic Gastrojejunostomy Recovery | Laparoscopic Gastrojejunostomy Information | Laparoscopic Gastrojejunostomy Thailand | Laparoscopic Gastrojejunostomy In Malaysia | Laparoscopic Gastrojejunostomy Abroad | Laparoscopic Gastrojejunostomy Donors | Laparoscopic Gastrojejunostomy Overseas | Laparoscopic Gastrojejunostomy Low Cost | Laparoscopic Gastrojejunostomy In Singapore | Laparoscopic Gastrojejunostomy In Argentina | Percutaneous Gastrojejunostomy | Chronic Bowel Obstruction | Gostronomy Tube
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


