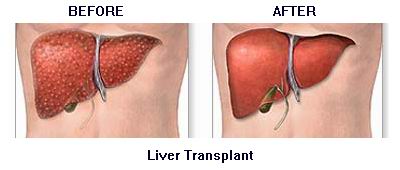
A liver transplant is a surgical procedure in which a diseased liver is replaced with a healthy liver from a donor. The liver is a vital organ responsible for numerous essential functions, including detoxifying harmful substances in the body, producing bile to aid digestion, storing energy, and producing important proteins such as albumin and clotting factors. When the liver becomes severely damaged or diseased, it can no longer perform these functions effectively, leading to liver failure.
Liver transplants are typically performed when other treatment options, such as medication or lifestyle changes, have failed to restore liver function. The two types of liver transplant are:
-
Deceased Donor Transplant:
-
This involves receiving a liver from a deceased donor who has been declared brain dead but whose liver is still functioning.
-
-
Living Donor Transplant:
-
In this case, a portion of a living person's liver (usually a family member or close relative) is transplanted into the recipient. The liver has the unique ability to regenerate, so both the donor's and recipient’s liver will grow back to full size over time.
-
Why a Liver Transplant is Needed
A liver transplant is necessary when the liver is no longer able to function due to:
-
Chronic liver disease (such as cirrhosis)
-
Liver cancer (when the cancer is confined to the liver)
-
Acute liver failure (a sudden loss of liver function)
The decision to undergo a liver transplant is made after assessing the severity of the liver condition, the patient’s overall health, and the availability of a suitable donor.
Liver transplants are typically performed to treat individuals with liver failure, caused by several medical conditions that severely damage the liver. Understanding the underlying causes and risk factors of liver disease can help in early detection and prevention.
Causes of Liver Failure
-
Chronic Hepatitis:
-
Hepatitis B and C are viral infections that cause chronic liver inflammation, eventually leading to cirrhosis (scarring of the liver), which can lead to liver failure.
-
-
Cirrhosis:
-
Cirrhosis is the scarring of the liver tissue caused by chronic liver damage. The leading causes of cirrhosis include chronic alcohol use, hepatitis infections, and fatty liver disease.
-
-
Fatty Liver Disease:
-
Non-alcoholic fatty liver disease (NAFLD) is associated with obesity, diabetes, and high cholesterol, where fat accumulates in the liver, leading to inflammation and damage. Over time, this can result in cirrhosis.
-
-
Liver Cancer:
-
Liver cancer, often associated with cirrhosis or chronic hepatitis, can require a liver transplant if it is localized to the liver and has not spread to other organs.
-
-
Genetic Disorders:
-
Conditions like Wilson’s disease, hemochromatosis, and alpha-1 antitrypsin deficiency can lead to liver failure due to abnormal accumulation of copper, iron, or proteins in the liver.
-
-
Autoimmune Liver Disease:
-
Conditions like autoimmune hepatitis occur when the immune system mistakenly attacks the liver, causing inflammation and liver damage over time.
-
-
Acute Liver Failure:
-
Sudden liver failure caused by a viral infection, drug overdose (especially acetaminophen), or toxins can result in a need for an emergency liver transplant.
-
Risk Factors for Liver Disease
-
Excessive Alcohol Consumption:
-
Long-term heavy drinking is a leading cause of cirrhosis and liver failure.
-
-
Obesity:
-
Being overweight increases the risk of fatty liver disease, which can eventually lead to cirrhosis and liver failure.
-
-
Viral Hepatitis:
-
Chronic hepatitis B and C infections are significant risk factors for developing cirrhosis and liver cancer.
-
-
Genetic Factors:
-
A family history of liver disease, such as hemochromatosis or Wilson’s disease, increases the risk of liver failure.
-
-
Exposure to Toxins:
-
Long-term exposure to environmental toxins or certain medications (such as acetaminophen overdose) can lead to liver damage.
-
When the liver begins to fail, it can lead to a variety of symptoms that progressively worsen over time. Early signs may be subtle, but as liver function deteriorates, symptoms can become more severe and life-threatening.
Common Symptoms of Liver Failure
-
Fatigue and Weakness:
-
One of the earliest signs of liver failure is constant fatigue and weakness, as the liver is unable to produce energy-regulating proteins effectively.
-
-
Yellowing of the Skin and Eyes (Jaundice):
-
Jaundice occurs when the liver can no longer process bilirubin, a byproduct of red blood cell breakdown. This results in a yellowish tint to the skin and eyes.
-
-
Abdominal Swelling (Ascites):
-
Fluid retention in the abdomen, also known as ascites, is a common sign of liver failure due to the liver's inability to process proteins that regulate fluid balance.
-
-
Nausea and Vomiting:
-
The buildup of toxins in the bloodstream due to liver dysfunction can cause nausea, vomiting, and loss of appetite.
-
-
Itchy Skin (Pruritus):
-
The accumulation of bile salts in the skin causes severe itching, which is common in liver disease.
-
-
Easy Bruising and Bleeding:
-
The liver produces clotting factors, and when its function declines, the body becomes more prone to bruising and bleeding easily.
-
-
Cognitive Changes (Hepatic Encephalopathy):
-
A severe liver condition can lead to hepatic encephalopathy, a state of confusion or altered consciousness due to the buildup of toxins in the brain.
-
-
Dark Urine:
-
Dark urine, often appearing amber or tea-colored, is a common sign of liver dysfunction and jaundice.
-
When to Seek Medical Attention
If you experience any of these symptoms—especially jaundice, fatigue, or abdominal swelling—it’s essential to seek medical attention immediately. Liver failure can progress rapidly, and a liver transplant may be required to save a patient's life.
Diagnosing liver failure involves a combination of clinical evaluation, blood tests, imaging studies, and sometimes a biopsy. The healthcare provider will consider the patient’s medical history, risk factors, and symptoms to determine the need for a liver transplant.
Diagnostic Tests for Liver Failure
-
Blood Tests:
-
Liver Function Tests (LFTs): Blood tests that measure the levels of liver enzymes, bilirubin, albumin, and clotting factors. Elevated levels of liver enzymes or bilirubin can indicate liver damage.
-
Coagulation Profile: A test that assesses the blood's ability to clot. Liver failure can lead to abnormal clotting.
-
-
Imaging Tests:
-
Ultrasound: A liver ultrasound can assess the size and texture of the liver and check for signs of cirrhosis or liver cancer.
-
CT Scan or MRI: These provide detailed images of the liver, helping to detect tumors or liver damage that could necessitate a transplant.
-
Elastography: A non-invasive imaging test to measure liver stiffness, indicating the degree of fibrosis or cirrhosis.
-
-
Liver Biopsy:
-
In some cases, a small tissue sample from the liver may be taken to assess the extent of damage and determine the underlying cause of liver failure.
-
-
MELD Score:
-
The Model for End-Stage Liver Disease (MELD) score is a system used to assess the severity of liver disease and prioritize patients on the transplant waiting list based on their risk of death.
-
Liver Transplant Surgery
A liver transplant is the only definitive treatment for liver failure when the liver cannot regenerate or recover on its own. The transplant involves the surgical removal of the diseased liver and its replacement with a healthy liver from either a deceased or living donor.
-
Deceased Donor Transplant:
-
This is the most common method, where a liver from a deceased donor is transplanted into the recipient. The donor liver must be a match based on blood type and other compatibility factors.
-
-
Living Donor Transplant:
-
In some cases, a living donor can donate a portion of their liver. The donor's liver regenerates over time, and the recipient’s liver grows to full size.
-
-
Immunosuppressive Medications:
-
After a liver transplant, patients must take immunosuppressive medications to prevent rejection of the new liver. These medications are typically required for the rest of the patient's life.
-
Non-Surgical Treatment Options
While a liver transplant is the most effective solution for liver failure, there are other medical options to manage the condition:
-
Medications for Liver Disease:
-
Antiviral drugs: Used to treat hepatitis B or C.
-
Diuretics: To manage fluid buildup (ascites) in patients with cirrhosis.
-
Beta-blockers: To reduce the risk of bleeding due to portal hypertension.
-
-
Liver Dialysis:
-
In some cases of acute liver failure, patients may need liver dialysis, a procedure that temporarily performs the functions of the liver while awaiting a transplant.
-
Prevention of Liver Disease Leading to Liver Transplant
-
Avoid Excessive Alcohol Consumption:
-
Limiting alcohol intake can reduce the risk of liver damage and cirrhosis.
-
-
Vaccination Against Hepatitis:
-
Vaccines are available for hepatitis A and B, which can prevent liver infection and the long-term effects of chronic hepatitis.
-
-
Healthy Diet and Exercise:
-
Maintaining a healthy weight, exercising regularly, and eating a balanced diet can reduce the risk of NAFLD (non-alcoholic fatty liver disease) and cirrhosis.
-
-
Regular Screening:
-
People with a family history of liver disease or those with chronic conditions like hepatitis should undergo regular liver function tests and screenings.
-
Post-Transplant Management
-
Medications:
-
Post-transplant patients will need to take immunosuppressive medications to prevent rejection of the new liver. Managing the dosage and monitoring side effects is essential.
-
-
Lifestyle Modifications:
-
Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, is important to maintain liver function and overall health.
-
-
Regular Follow-ups:
-
Frequent visits to the transplant center are necessary for blood tests, liver function tests, and to monitor for complications like rejection or infection.
-
While liver transplants are highly effective, complications can occur. These may include:
-
Rejection:
-
The immune system may attempt to reject the new liver. This can be controlled with immunosuppressive drugs.
-
-
Infection:
-
Immunosuppressive drugs increase the risk of infections, including bacterial, viral, and fungal infections.
-
-
Graft Failure:
-
In rare cases, the transplanted liver may fail, requiring a second transplant.
-
-
Cancer:
-
Post-transplant patients have an increased risk of developing cancers, particularly due to immunosuppressive medication.
-
After receiving a liver transplant, patients can experience a significant improvement in quality of life. However, they will need to make ongoing adjustments and lifestyle changes to maintain their health.
-
Adherence to Medication:
-
Lifelong adherence to immunosuppressive medications is necessary to prevent liver rejection and other complications.
-
-
Dietary Changes:
-
A healthy diet, rich in fruits, vegetables, and lean proteins, is crucial for supporting the new liver and maintaining overall health.
-
-
Mental Health Support:
-
Transplant recipients may face emotional and psychological challenges, including anxiety, depression, and post-traumatic stress. Psychological support and counseling can be helpful.
-
-
Regular Monitoring:
-
Continued follow-up appointments are critical for monitoring liver function, managing medications, and detecting complications early.
-
1. What is a liver transplant?
A liver transplant is a surgery in which a failing or damaged liver is replaced with a healthy liver from a donor. This procedure is usually recommended for people with chronic liver diseases, liver failure, or liver cancer that cannot be treated by other means.
2. Who needs a liver transplant?
Individuals with liver failure, cirrhosis, acute liver failure, or certain forms of liver cancer may require a liver transplant. The liver’s functions such as detoxification, protein production, and regulation of metabolism become severely impaired when it fails, leading to the need for a transplant.
3. What are the common causes of liver failure?
Some of the most common causes of liver failure include:
-
Chronic alcohol abuse
-
Hepatitis B or C
-
Non-alcoholic fatty liver disease (NAFLD)
-
Liver cancer
-
Genetic disorders like hemochromatosis or Wilson’s disease
4. What are the risks involved in a liver transplant?
While liver transplant surgeries have a high success rate, there are potential risks, including:
-
Rejection of the new liver
-
Infection due to immunosuppressive drugs
-
Complications from the surgery, like bleeding
-
Liver dysfunction or failure after transplant
-
Blood clots and bile duct issues
5. How long is the waiting list for a liver transplant?
The waiting list varies depending on factors such as the urgency of the transplant, blood type, and the patient's overall health. It could take anywhere from a few months to several years. The time on the list depends largely on the availability of suitable donor livers.
6. What is the success rate of liver transplants?
Liver transplants generally have a high success rate. The one-year survival rate is approximately 85-90%, and the five-year survival rate is around 70-75%. Success rates improve with careful post-transplant care, including proper medication adherence and regular check-ups.
7. What are the post-surgery care requirements for liver transplant recipients?
Post-surgery care is crucial for the success of the transplant. It includes:
-
Taking immunosuppressive medications to prevent liver rejection
-
Regular blood tests to monitor liver function
-
Avoiding infections by practicing hygiene and avoiding crowded places
-
Healthy lifestyle choices, including a balanced diet and regular exercise
8. Can a liver transplant be rejected?
Yes, the body may reject the transplanted liver if it identifies it as foreign. This is why patients must take immunosuppressive drugs for life to help prevent rejection. However, rejection is usually treatable if caught early and managed properly.
9. How long does a liver transplant surgery take?
Liver transplant surgery typically lasts between 6 to 12 hours, depending on the complexity of the case. The time varies based on the patient's condition and whether a living donor or deceased donor is used.
10. How long will a liver transplant last?
The new liver can last for many years, but its longevity depends on several factors, including the patient’s age, overall health, lifestyle, and how well they adhere to post-surgery care instructions. On average, a transplanted liver lasts 10-20 years, but some patients may require a second transplant after many years.
The other Gastro procedures are:
Few Major Hospitals for Liver Transplant are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Liver Transplant | Doctors For Liver Transplant | Surgery Liver Transplant | Cost Liver Transplant | Treatment Liver Transplant | Destinations Liver Transplant | Risks Liver Transplant | Liver Transplant In India | Liver Transplant Recovery | Liver Transplant Information | Liver Transplant Thailand | Liver Transplant In Malaysia | Liver Transplant Abroad | Liver Transplant Donors | Liver Transplant Overseas | Liver Transplant Low Cost | Liver Transplant In Singapore | Liver Transplant In Argentina | Liver Transplant | Liver Failure | Acute Liver Failure | Chronic Hepatitis With Cirrhosis | Biliary Cirrhosis | Sclerosing Cholangitis | Wilson’s Disease | Hepatologist | Liver Specialist | Liver Cancer
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


