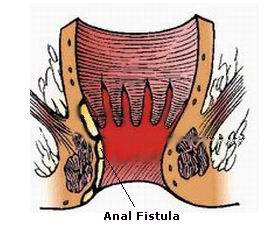
An anal fistula is an abnormal tunnel-like structure that forms between the skin near the anus and the inside of the anal canal. This condition often arises as a result of an infection in the anal glands, leading to the formation of an abscess. When the abscess does not heal completely, it can create a passage that connects the infected area to the skin near the anus.
Anal fistulas are common among individuals who experience complications from anal abscesses. They can be painful, uncomfortable, and distressing, often affecting the daily life and well-being of those who suffer from them. Anal fistulas can vary in severity, with some being minor and others leading to significant complications if left untreated.
This condition is more commonly found in men, but it can affect people of all genders and ages. Fortunately, modern medical advancements have provided effective treatment options to manage and alleviate symptoms. Understanding the causes, symptoms, diagnosis, and treatment options for anal fistulas is crucial for effective management.
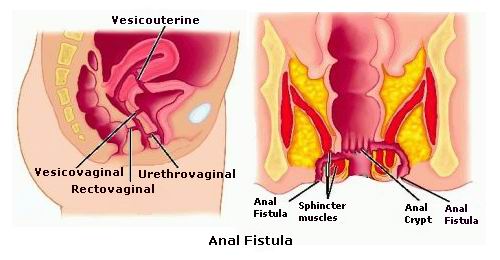
The development of an anal fistula typically begins when an infection occurs in the anal glands. These glands are small structures located in the lining of the anal canal that secrete fluids. When the glands become blocked, bacteria can accumulate, causing an infection known as an anal abscess. If the abscess does not heal properly, it can form a tunnel that extends to the skin near the anus, resulting in an anal fistula.
Common Causes:
-
Anal Abscesses: Most anal fistulas originate from an anal abscess, which is a pus-filled cavity that forms in the anal region due to blocked glands.
-
Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease or ulcerative colitis can increase the risk of developing anal fistulas due to inflammation in the intestines.
-
Infections: Certain sexually transmitted infections (STIs) like gonorrhea or tuberculosis may contribute to the development of anal fistulas.
-
Trauma: Any injury or surgical procedure in the anal or rectal area can increase the risk of fistula formation.
-
Cancer: In some cases, cancer near the anal region can lead to fistula development, though this is rare.
Risk Factors:
-
Gender: Anal fistulas are more common in men, particularly in those who have had an abscess.
-
Age: The condition is more frequently diagnosed in adults, though it can occur at any age.
-
Medical History: Individuals with IBD, particularly Crohn’s disease, have a significantly higher risk.
-
Previous Anal Surgery: Surgery involving the anal or rectal areas increases the risk of fistulas.
-
Poor Hygiene: Individuals who experience chronic infections or poor hygiene in the anal region are at greater risk.
The symptoms of an anal fistula can vary depending on its size and location. Some people may experience no symptoms at all, while others may have severe pain or discomfort.
Common Symptoms:
-
Pain: A dull, throbbing pain around the anus, particularly during bowel movements or while sitting.
-
Discharge: Pus or blood may drain from the opening of the fistula, which can be accompanied by an unpleasant odor.
-
Irritation: The skin around the anus may become irritated due to continuous drainage from the fistula.
-
Itching: Itching around the anus can be a result of the fistula or the drainage.
-
Swelling: The area around the anus may appear swollen or inflamed, especially during an active infection.
-
Fever: In some cases, an infection in the fistula can cause fever and chills.
Other Signs:
-
Recurrent Abscesses: People with anal fistulas often experience recurring abscesses in the same area, which may open up and drain on their own.
If you experience any of these symptoms, it’s important to seek medical attention, as untreated anal fistulas can lead to further complications and discomfort.
Diagnosing an anal fistula generally involves a physical examination and various diagnostic tests. Early detection is important for effective treatment and to prevent complications.
Diagnosis Process:
-
Physical Examination: The doctor will examine the perianal region for visible signs of a fistula. They may ask about your symptoms and medical history.
-
Digital Rectal Exam: During a digital rectal exam, the doctor will insert a finger into the rectum to check for abnormalities, tenderness, or signs of infection.
-
Imaging Tests: If the fistula cannot be clearly identified through physical examination, the doctor may recommend:
-
Endorectal Ultrasound: This technique uses sound waves to visualize the fistula and its structure.
-
MRI (Magnetic Resonance Imaging): MRI provides detailed images of the fistula’s course and helps determine its complexity.
-
Fistulography: A special dye is injected into the fistula to visualize its path on an X-ray.
-
The treatment for anal fistulas typically involves surgical intervention to remove or repair the fistula and ensure proper healing. The treatment chosen will depend on the size, location, and complexity of the fistula.
Common Treatment Options:
-
Fistulotomy: This is the most common surgical treatment for simple anal fistulas. The fistula tract is opened, allowing it to heal from the inside out.
-
Seton Placement: A seton is a surgical thread placed through the fistula tract to help drain it and promote healing. This option is used for more complex fistulas.
-
Flap Surgery: For complex fistulas, tissue from the surrounding area may be used to cover the fistula opening, allowing the tract to heal properly.
-
Fibrin Glue: Fibrin glue is injected into the fistula to close it off. This is a less invasive procedure but may not be effective for more complex fistulas.
-
Ligation of the Intersphincteric Fistula Tract (LIFT): This technique involves ligating (tying off) the fistula tract to promote healing while minimizing the risk of incontinence.
Non-Surgical Treatments:
-
Antibiotics: If the fistula is infected, antibiotics may be prescribed to treat the infection before surgery.
-
Pain Management: Over-the-counter or prescription pain medications may be recommended to manage discomfort associated with the condition.
While it’s not always possible to prevent the formation of an anal fistula, there are certain lifestyle changes and practices that can reduce the risk of developing one:
Preventative Measures:
-
Maintain Good Hygiene: Keeping the anal area clean and dry is essential for preventing infections that could lead to fistulas.
-
Diet and Fluid Intake: A healthy, high-fiber diet can prevent constipation, which can contribute to anal fissures and abscesses.
-
Prompt Treatment of Anal Abscesses: Early treatment of any anal abscesses can reduce the risk of developing a fistula.
If left untreated, anal fistulas can lead to several complications, including:
-
Infection: Untreated fistulas can lead to recurring abscesses, chronic infections, and systemic infections.
-
Incontinence: In some cases, surgical treatment can damage the sphincter muscles, leading to difficulty controlling bowel movements.
-
Recurrent Fistulas: Some anal fistulas can return after treatment, requiring additional procedures.
Living with an anal fistula can be challenging due to the discomfort and potential for ongoing symptoms. However, with the right treatment and care, most people can manage the condition effectively. It’s important to:
-
Follow Treatment Plans: Ensure regular follow-ups and adhere to prescribed treatments.
-
Manage Symptoms: Take steps to control pain, reduce inflammation, and prevent infections.
-
Mental Health Support: Dealing with an anal fistula can be emotionally taxing, so seeking mental health support or joining a support group can help manage the psychological impact.
1. What is an anal fistula?
An anal fistula is an abnormal tunnel or
passage that forms between the skin around the anus and the inside of the anal canal. It
typically occurs after an infection in the anal glands, leading to an abscess that drains
pus. Over time, the abscess may develop into a fistula, causing discomfort, pain, and
sometimes bleeding.
2. What causes an anal fistula?
The most common cause of an anal fistula is a previous anal abscess, which occurs when the anal glands become infected. Other causes may include:
-
Chronic inflammatory diseases, such as Crohn’s disease.
-
Trauma or injury to the anal area.
-
Cancer affecting the anal or rectal area.
-
Tuberculosis or other infections.
3. What are the symptoms of an anal fistula?
The symptoms of an anal fistula can vary depending on its severity and location. Common symptoms include:
-
Pain or discomfort around the anus.
-
Drainage of pus or blood from a small opening near the anus.
-
Itching or irritation in the affected area.
-
Foul-smelling discharge from the fistula.
-
Swelling or redness around the anus.
4. How is an anal fistula diagnosed?
To diagnose an anal fistula, the doctor will perform a physical examination of the anal area. This may include:
-
Digital rectal exam: The doctor may gently insert a gloved finger into the rectum to check for any abnormalities.
-
Anoscopy: A special instrument (anoscope) is inserted into the anus to view the internal opening of the fistula.
-
Imaging tests: In some cases, MRI or endorectal ultrasound may be used to get a clearer picture of the fistula's size, depth, and path.
5. How is an anal fistula treated?
Treatment for an anal fistula typically involves surgery to close the abnormal passage and prevent further infection. Common treatment options include:
-
Fistulotomy: The most common procedure where the fistula is cut open to allow it to heal.
-
Seton placement: A rubber band or thread is placed through the fistula to help drain any infection and allow it to heal gradually.
-
Flap surgery: A tissue flap from another part of the body is used to cover the fistula and promote healing.
-
Advancement flap surgery: Used for complex fistulas, this procedure involves moving tissue to close the fistula's internal opening.
6. Is surgery the only treatment for an anal fistula?
Surgery is the most effective treatment for an anal fistula, as it is designed to completely
eliminate the abnormal passage. However, some less invasive treatments, such as antibiotics, may be used to manage infection
or inflammation before surgery. In rare cases, a seton (a draining thread) may be used to manage the condition
without immediate surgery.
7. Are there any risks or complications with anal fistula surgery?
As with any surgery, there are risks associated with anal fistula treatment, including:
-
Infection at the surgical site.
-
Bleeding during or after surgery.
-
Incontinence: In some cases, surgery can damage the muscles around the anus, leading to temporary or permanent incontinence.
-
Recurrence of the fistula: Although rare, a fistula may return after surgery, requiring further treatment.
8. How long is the recovery time after anal fistula surgery?
Recovery time varies depending on the type of surgery performed. For a simple fistulotomy, patients can usually
return to normal activities within 2 to 4
weeks. However, for more complex procedures, such as flap surgery, recovery may take 4 to 6 weeks. During the recovery period, it is important to
follow the doctor’s instructions, including wound care, pain management, and avoiding
strenuous activities.
9. Can an anal fistula be prevented?
While it’s not always possible to prevent an anal fistula, certain measures can help reduce
the risk:
-
Good hygiene: Keeping the anal area clean and dry can help prevent infections.
-
Avoiding constipation: Straining during bowel movements can increase the risk of developing anal issues. Eating a high-fiber diet, staying hydrated, and using stool softeners can help prevent constipation.
-
Prompt treatment of abscesses: If you experience symptoms of an anal abscess, such as pain, swelling, or drainage, seek medical attention promptly to reduce the risk of developing a fistula.
10. Is an anal fistula covered by insurance?
Yes, the treatment for anal fistulas is generally covered by most insurance plans when
medically necessary. This typically includes diagnostic tests, outpatient surgery, and
post-operative care. It’s important to check with your insurance provider to confirm
coverage details, including co-pays and any out-of-pocket expenses.
The other general procedures are:
Few Major Hospitals for Treatment of Anal Fistula are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Anal Fistula | Hospitals Anal Fistula | Doctors Anal Fistula | Surgery Anal Fistula | Cost Of Anal Fistula | Treatment For Anal Fistula | Destinations For Anal Fistula | Risks Anal Fistula | Anal Fistula India | Anal Fistula Recovery | Anal Fistula Information | Anal Fistula Thailand | Anal Fistula Malaysia | Anal Fistula Abroad | Anal Fistula Overseas | Anal Fistula Low Cost | Anal Fistula Singapore | Ibs | Irritable Bowel Syndrome | Diverticulitis | Ulcerative Colitis | Tuberculosis | Gonorrhoea | Cancer Of The Rectum | Fistula | Fistulotomy | Rectal Flap Advancement | Seton Placement | Fibrin Glue
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



