A hemorrhoidectomy is a surgical procedure used to remove hemorrhoids—swollen blood vessels in the lower rectum or anus that can cause significant discomfort and bleeding. Hemorrhoids are a common condition, with many individuals experiencing symptoms like itching, pain, and bleeding during bowel movements. In some cases, conservative treatments such as dietary changes, medications, and lifestyle modifications are sufficient for managing hemorrhoids. However, for individuals with severe or persistent hemorrhoids that do not respond to non-surgical treatments, a hemorrhoidectomy may be necessary.
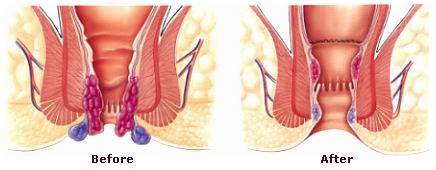
The procedure typically involves the removal of either internal or external hemorrhoids, or both, depending on the severity of the condition. Hemorrhoidectomy is usually performed when other treatment methods—such as creams, suppositories, or minimally invasive procedures—fail to provide relief.
There are different techniques for hemorrhoidectomy, including traditional open hemorrhoidectomy, closed hemorrhoidectomy, and stapled hemorrhoidopexy. The choice of technique depends on the surgeon’s preference, the type of hemorrhoids, and the severity of the condition.
Hemorrhoids develop when there is increased pressure on the veins in the rectal or anal area, leading to swelling. This can result from various factors, many of which are related to lifestyle and habits.
Causes of Hemorrhoids:
-
Chronic Constipation or Diarrhea:
-
Straining during bowel movements due to chronic constipation or prolonged diarrhea can put extra pressure on the rectal veins, causing them to enlarge and form hemorrhoids.
-
-
Pregnancy:
-
During pregnancy, the growing uterus places pressure on the veins in the pelvic area, leading to hemorrhoid formation. Hormonal changes can also weaken the veins, making them more prone to swelling.
-
-
Obesity:
-
Excess body weight, especially around the abdomen, can increase pressure on the veins in the rectal and anal areas, contributing to hemorrhoids.
-
-
Prolonged Sitting or Standing:
-
Spending long periods sitting or standing—particularly on the toilet—can lead to increased pressure on the veins of the rectum, promoting the formation of hemorrhoids.
-
-
Age:
-
As people age, the tissues supporting the rectal veins can weaken and stretch, increasing the risk of hemorrhoids.
-
-
Heavy Lifting:
-
Repeated heavy lifting or strenuous physical activity can cause significant pressure in the pelvic area, leading to hemorrhoids.
-
-
Low-Fiber Diet:
-
A diet that is low in fiber can contribute to constipation, which, in turn, increases the risk of developing hemorrhoids.
-
Risk Factors for Hemorrhoids:
-
Family History: A family history of hemorrhoids may increase the likelihood of developing the condition.
-
Sedentary Lifestyle: A lack of physical activity increases the risk of constipation and poor circulation, both of which can contribute to hemorrhoid formation.
-
High Alcohol Consumption: Excessive drinking can lead to dehydration and constipation, which increases the risk of hemorrhoids.
While hemorrhoidectomy is a surgical procedure, the symptoms leading to it are common in individuals with severe hemorrhoids. Symptoms may vary depending on whether the hemorrhoids are internal (inside the rectum) or external (around the anus).
Symptoms of Internal Hemorrhoids:
-
Rectal Bleeding:
-
The most common symptom of internal hemorrhoids is bright red bleeding during bowel movements. This may be noticed on toilet paper or in the toilet bowl.
-
-
Pain During Bowel Movements:
-
Internal hemorrhoids may cause discomfort or a feeling of fullness or pressure in the rectum, especially when passing stools.
-
-
Prolapse:
-
In more severe cases, internal hemorrhoids may prolapse, meaning they protrude out of the anus during bowel movements. This can cause irritation and pain.
-
Symptoms of External Hemorrhoids:
-
Pain or Itching Around the Anus:
-
External hemorrhoids can cause itching, discomfort, and painful swelling around the anus, especially when sitting or during bowel movements.
-
-
Swelling or Lump:
-
A painful lump near the anus may be felt. This is typically the result of blood clots forming in external hemorrhoids (thrombosed hemorrhoids).
-
-
Bleeding:
-
Although less common, external hemorrhoids can also cause bleeding, particularly if they are irritated or thrombosed.
-
General Symptoms:
-
Mucus Discharge: Some individuals with internal hemorrhoids may experience mucus discharge from the anus, especially if the hemorrhoids are prolapsed.
-
Feeling of Incomplete Bowel Movements: A sensation of incomplete evacuation after using the bathroom can occur in cases of prolapsed internal hemorrhoids.
If hemorrhoid symptoms become severe, cause significant pain, or do not improve with conservative treatments, a hemorrhoidectomy may be necessary.
The diagnosis of hemorrhoids and the need for surgery is typically made through a combination of physical examination, medical history, and specific diagnostic tests.
Diagnosis Process:
-
Physical Examination:
-
The doctor will first conduct a thorough examination of the anal and rectal areas to check for external hemorrhoids and any signs of internal hemorrhoids. This may involve visual inspection and a digital rectal exam to feel for any internal abnormalities.
-
-
Anoscopy:
-
An anoscope is a small tube with a light used to look inside the anus and rectum. It helps the doctor identify internal hemorrhoids that may not be visible externally.
-
-
Sigmoidoscopy or Colonoscopy:
-
If there is concern about other underlying conditions, such as colon cancer, a sigmoidoscopy or colonoscopy may be performed. These procedures allow for a detailed examination of the colon and rectum using a flexible tube with a camera.
-
Treatment for hemorrhoids typically starts with conservative methods such as lifestyle changes, dietary modifications, and topical treatments. However, in cases where these methods are ineffective, or for individuals with severe hemorrhoids, surgical intervention may be necessary.
Non-Surgical Treatments:
-
Dietary Changes:
-
A high-fiber diet can help reduce constipation and ease bowel movements, thus reducing the pressure on the rectal veins. Fiber-rich foods such as fruits, vegetables, and whole grains are recommended.
-
Drinking plenty of water is essential to avoid dehydration and constipation.
-
-
Topical Treatments:
-
Over-the-counter creams, ointments, and suppositories containing ingredients like hydrocortisone or witch hazel can provide temporary relief from pain, itching, and inflammation.
-
-
Sitz Baths:
-
Soaking the anal area in warm water (a sitz bath) several times a day can help soothe irritation and reduce swelling.
-
-
Stool Softeners:
-
Stool softeners can help reduce straining during bowel movements, which is a major cause of hemorrhoids.
-
Surgical Treatments (Hemorrhoidectomy):
When hemorrhoids become large, painful, or thrombosed, surgery may be required. The primary surgical treatment options are:
-
Traditional Hemorrhoidectomy:
-
The surgeon removes the hemorrhoid tissue through an incision around the anus. This is typically performed under general anesthesia, and the procedure may involve either an open or closed technique.
-
Open hemorrhoidectomy: The wound is left open to heal naturally.
-
Closed hemorrhoidectomy: The wound is stitched up after surgery.
-
-
Stapled Hemorrhoidopexy (PPH):
-
This is a newer, minimally invasive technique in which a stapler is used to remove part of the hemorrhoid and reposition it. It is generally associated with less pain and a quicker recovery compared to traditional hemorrhoidectomy.
-
-
Laser Surgery:
-
Laser surgery uses high-energy light to remove or shrink the hemorrhoid tissue. It’s less invasive but may not be suitable for all types of hemorrhoids.
-
Preventing hemorrhoids and minimizing their recurrence after surgery can significantly improve the quality of life. Here are some preventive measures:
Preventive Measures:
-
Maintain a High-Fiber Diet:
-
A high-fiber diet helps soften stools, reducing the risk of constipation and the need to strain during bowel movements. Include whole grains, fruits, vegetables, and legumes in your daily diet.
-
-
Exercise Regularly:
-
Regular physical activity, including walking, helps maintain bowel regularity and prevents constipation.
-
-
Stay Hydrated:
-
Drinking plenty of water keeps the stool soft and makes bowel movements easier to pass.
-
-
Avoid Straining:
-
Avoid prolonged sitting on the toilet and straining during bowel movements. Respond promptly to the urge to go to the bathroom.
-
-
Good Toilet Habits:
-
Use gentle toilet paper and avoid harsh wiping. Consider using wet wipes or a sitz bath to keep the area clean.
-
While hemorrhoidectomy is a common and generally safe procedure, it is not without potential risks and complications:
-
Infection:
-
As with any surgery, there is a risk of infection, though it is relatively rare. Proper wound care and hygiene after surgery help minimize this risk.
-
-
Bleeding:
-
Bleeding during or after surgery is a potential complication, especially in the first few days after surgery.
-
-
Incontinence:
-
In rare cases, damage to the anal sphincter muscles can lead to fecal incontinence, or the inability to control bowel movements.
-
-
Pain:
-
Post-surgical pain is common, but it can be managed with pain relievers and proper aftercare. Persistent pain should be reported to a healthcare provider.
-
-
Recurrence:
-
While surgery offers long-term relief, some patients may experience recurrence of hemorrhoids if lifestyle changes (such as diet and exercise) are not maintained.
-
After hemorrhoidectomy, most patients experience relief from hemorrhoid symptoms and can return to normal activities within a few weeks. However, there are some lifestyle adjustments and considerations for living with the condition post-surgery.
Post-Surgery Recovery:
-
Pain Management:
-
Over-the-counter pain medications, stool softeners, and warm sitz baths can help ease recovery.
-
-
Activity Restrictions:
-
Avoid heavy lifting, strenuous activities, and prolonged sitting for a few weeks after surgery to reduce pressure on the surgical site.
-
-
Dietary Adjustments:
-
Follow a fiber-rich diet to promote soft stools and prevent constipation. Drink plenty of water to keep stools hydrated.
-
-
Follow-up Care:
-
Regular follow-ups with the surgeon are important to monitor recovery and address any concerns such as bleeding, infection, or recurrence.
-
1. What is hemorrhoidectomy?
Hemorrhoidectomy is a surgical procedure used to remove hemorrhoids, which are swollen blood vessels in the rectum or anus that cause pain, bleeding, and discomfort. This procedure is typically recommended when conservative treatments such as topical medications, fiber supplements, or rubber band ligation are ineffective.
2. Why do I need a hemorrhoidectomy?
Hemorrhoidectomy may be necessary if hemorrhoids are severe, causing chronic pain, excessive bleeding, or prolapse (when the hemorrhoid protrudes outside the anus). If other treatments have failed or the hemorrhoids are too large to be treated with less invasive methods, surgery may be the best option to relieve symptoms.
3. How is a hemorrhoidectomy performed?
Hemorrhoidectomy is typically performed under general or spinal anesthesia. The surgeon removes the hemorrhoids using a scalpel, laser, or other surgical tools. The procedure may involve excising the hemorrhoids or stapling them back into place, depending on the severity and type of hemorrhoids. The surgery usually takes about 30 to 60 minutes.
4. What are the risks of hemorrhoidectomy?
Like any surgical procedure, hemorrhoidectomy carries some risks, including infection, bleeding, difficulty urinating, and blood clots. Other risks may include pain or discomfort during recovery and the potential for new hemorrhoids to form. Your surgeon will discuss the risks and help you understand how to minimize complications.
5. What can I expect after a hemorrhoidectomy?
After surgery, you will be monitored in a recovery room until the anesthesia wears off. Most patients experience some discomfort, pain, and swelling in the treated area after the procedure. Pain management, including prescribed medications, will help alleviate these symptoms. You may also need to take sitz baths to promote healing and prevent infection.
6. How long does it take to recover from a hemorrhoidectomy?
Recovery time varies by individual but typically takes about 1 to 2 weeks for initial recovery, with full healing taking up to 4 to 6 weeks. During the recovery period, it’s important to follow post-operative care instructions, including avoiding constipation, eating high-fiber foods, and staying hydrated to promote healing.
7. What should I avoid after hemorrhoidectomy surgery?
After hemorrhoidectomy, you should avoid straining during bowel movements, sitting for long periods, and engaging in heavy lifting or strenuous activities for at least 4-6 weeks. Following a high-fiber diet, drinking plenty of fluids, and taking stool softeners can help prevent constipation and reduce strain on the healing area.
8. Is hemorrhoidectomy painful?
Hemorrhoidectomy can be painful during the recovery period, especially for the first few days after surgery. However, pain can usually be managed with prescribed medications, sitz baths, and other comfort measures. Following your doctor’s recommendations for post-surgery care will help minimize discomfort and promote faster healing.
9. How successful is hemorrhoidectomy surgery?
Hemorrhoidectomy is considered highly effective, with most patients experiencing significant relief from symptoms. The success rate of the procedure is generally high, and it is effective at removing hemorrhoids that have not responded to non-surgical treatments. However, in rare cases, hemorrhoids can recur, especially if lifestyle changes aren’t made to prevent them.
10. Are there any alternatives to hemorrhoidectomy?
Yes, there are less invasive treatments for hemorrhoids, such as rubber band ligation, sclerotherapy (injection treatment), and infrared coagulation. These options may be effective for smaller hemorrhoids and can be performed in a doctor’s office. However, for large or severe hemorrhoids, hemorrhoidectomy may be the most effective solution.
The other general procedures are:
Few Major Hospitals for Hemorrhoidectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hemorrhoidectomy | Hospitals Hemorrhoidectomy | Doctors Hemorrhoidectomy | Surgery Hemorrhoidectomy | Cost Of Hemorrhoidectomy | Treatment For Hemorrhoidectomy | Destinations For Hemorrhoidectomy | Risks Hemorrhoidectomy | Hemorrhoidectomy India | Hemorrhoidectomy Recovery | Hemorrhoidectomy Information | Hemorrhoidectomy Thailand | Hemorrhoidectomy Malaysia | Hemorrhoidectomy Abroad | Hemorrhoidectomy Overseas | Hemorrhoidectomy Low Cost | Hemorrhoidectomy Singapore | Hemorrhoid | Protruding Hemorrhoid | Thrombosed External Hemorrhoid | Anoscope | Lower Colon | Sigmoid | Stapled Hemorrhoidectomy
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



