A hernia occurs when an organ or tissue pushes through a weak spot or opening in the surrounding muscle or connective tissue. This condition can develop in various areas of the body, but it most commonly affects the abdominal wall, groin, and upper thigh. While many individuals may develop a hernia at some point in their lives, the most common types are inguinal, femoral, umbilical, hiatal, and incisional hernias.
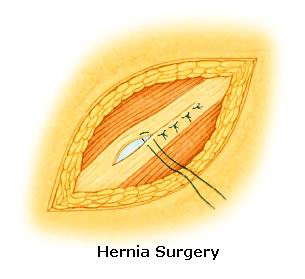
A hernia repair or herniorrhaphy is the surgical procedure used to correct a hernia. The goal of this surgery is to push the bulging tissue back into place and reinforce the weakened muscle or connective tissue wall. In most cases, the surgery is straightforward and highly successful in restoring normal anatomy and function. Laparoscopic hernia repair has become a widely preferred method due to its minimally invasive nature, smaller incisions, and faster recovery times compared to traditional open surgery.
Hernia repair is crucial to avoid complications such as bowel obstruction, strangulation (cut-off blood supply), or the hernia's growth, which may lead to more significant health risks. The decision to opt for surgery is influenced by factors like the hernia's size, symptoms, and the patient’s overall health. Modern hernia repair techniques now involve mesh reinforcement, which reduces the recurrence rates significantly.
Causes of Hernias
Hernias are primarily caused by increased pressure in the abdominal cavity combined with a weakness or defect in the surrounding muscle or connective tissue. Factors contributing to this pressure or weakness include:
-
Increased Abdominal Pressure
-
Straining during bowel movements due to constipation or chronic diarrhea.
-
Heavy lifting or intense physical activity that increases intra-abdominal pressure.
-
Chronic coughing due to conditions like asthma or smoking.
-
Pregnancy: The growing uterus adds pressure to the abdominal wall.
-
-
Weak Muscles or Connective Tissue
-
Congenital weakness: Some individuals are born with weaker abdominal muscles, making them more prone to hernias.
-
Previous surgeries: Abdominal surgeries, especially those involving large incisions, can weaken the muscles and increase the risk of hernias.
-
Age: With age, the muscles naturally weaken and become more prone to injury.
-
Injury: A physical injury or trauma to the abdomen can create a gap in the muscle wall.
-
Risk Factors for Hernia
Several factors may increase the risk of developing a hernia:
-
Obesity: Extra weight places more pressure on the abdominal muscles, increasing the risk of hernias.
-
Family History: A family history of hernias can predispose individuals to develop them.
-
Lifestyle: Smoking can reduce tissue strength and hinder the healing process, increasing the risk of hernias.
-
Chronic conditions: Certain conditions, such as chronic obstructive pulmonary disease (COPD) or cystic fibrosis, which involve frequent coughing, can lead to hernias.
-
Gender: Inguinal hernias, which occur in the groin area, are more common in men than in women.
Hernias often cause noticeable symptoms, but in some cases, individuals may experience no symptoms at all, particularly if the hernia is small. Common signs and symptoms of a hernia that may prompt surgery include:
1. Visible Lump or Bulge
A lump or bulge near the abdomen, groin, or upper thigh is often the first sign of a hernia. The lump may become more prominent when standing, bending over, or coughing. For inguinal hernias, the bulge may be noticeable in the groin, while umbilical hernias cause a bulge near the belly button.
2. Pain or Discomfort
Pain or discomfort, especially while lifting, bending, or coughing, is a common symptom. The pain may be dull and achy or sharp and intense. Some hernias may cause acute pain, particularly if they are large or have developed complications like strangulation.
3. Burning or Aching Sensation
Some individuals experience a burning or aching sensation at the site of the hernia, particularly when pressure is applied.
4. Nausea or Vomiting
If a hernia becomes incarcerated (trapped) or strangulated (cut-off blood supply), it can cause severe symptoms like nausea, vomiting, and constipation, indicating that immediate surgical intervention is required.
5. Discomfort when Lifting or Bending
People with a hernia often experience increased pain when they strain during physical activities like lifting, twisting, or bending.
6. Feeling of Fullness or Pressure
A sensation of fullness or pressure in the abdomen is common, particularly with hiatal hernias, where the stomach pushes through the diaphragm into the chest cavity.
The diagnosis of a hernia typically involves a combination of a thorough physical examination and imaging tests to assess the severity and location of the hernia.
1. Physical Examination
The doctor will conduct a visual and manual examination of the suspected area, typically while the patient is standing or coughing to make the hernia bulge more noticeable. The doctor may ask the patient to cough or strain to evaluate how the hernia changes during increased intra-abdominal pressure.
2. Imaging Tests
To determine the size, location, and potential complications, the following imaging tests may be used:
-
Ultrasound: This imaging technique uses sound waves to create an image of the hernia, helping to assess the bulging tissue.
-
CT Scan: A CT scan can help identify the presence of a hernia, particularly in complicated cases, and is used when the hernia is not easily visible.
-
X-ray: An X-ray may be performed if there’s suspicion of bowel obstruction or other internal complications.
3. Endoscopy or Colonoscopy
For hiatal hernias, an endoscopy or colonoscopy may be performed to view the internal lining of the esophagus or abdomen and assess how the hernia is affecting the gastrointestinal tract.
Once diagnosed, the treatment for a hernia depends on its size, location, and severity. In many cases, surgery is required to repair the hernia. Treatment options include:
1. Open Hernia Surgery
Open hernia surgery involves making a large incision near the hernia site. The surgeon then pushes the protruding tissue back into place and reinforces the abdominal wall using sutures or a mesh patch. This traditional approach may be recommended for larger hernias or cases where laparoscopic surgery is not feasible.
2. Laparoscopic (Minimally Invasive) Surgery
Laparoscopic hernia repair is a minimally invasive procedure that involves making several small incisions through which a camera (laparoscope) and surgical tools are inserted. The surgeon uses the laparoscope to view the hernia and repair it using small instruments. The advantages of laparoscopic surgery include:
-
Smaller incisions and minimal scarring.
-
Shorter recovery times.
-
Reduced risk of infection and less postoperative pain.
3. Robotic-Assisted Hernia Surgery
In some cases, robotic-assisted surgery may be used, which allows for greater precision in surgery. This technique is similar to laparoscopic surgery but involves a robot-controlled system to assist the surgeon.
4. Mesh Repair
In both open and laparoscopic hernia repair, mesh is commonly used to reinforce the abdominal wall and reduce the risk of recurrence. The mesh acts as a barrier that supports the weakened tissue, preventing the hernia from returning.
5. Non-Surgical Treatments
In some cases, particularly with small hernias that are not causing pain or complications, doctors may recommend watchful waiting. Conservative measures such as lifestyle changes, weight management, and avoiding heavy lifting may help prevent the hernia from worsening.
Prevention
While not all hernias can be prevented, certain lifestyle changes can help reduce the risk:
-
Maintain a healthy weight: Excess body weight puts added pressure on the abdominal muscles, increasing the risk of hernias.
-
Increase fiber intake: A high-fiber diet helps prevent constipation and reduces the need for straining during bowel movements.
-
Exercise regularly: Strengthening the abdominal muscles through exercise can help prevent hernias from forming.
-
Avoid heavy lifting: Proper lifting techniques and avoiding heavy lifting can help reduce the risk.
-
Quit smoking: Smoking can weaken the tissues and increase the risk of hernias.
Post-Operative Care
After hernia repair surgery, patients are advised to:
-
Rest and avoid heavy physical activity for several weeks.
-
Use stool softeners to avoid straining during bowel movements.
-
Follow a high-fiber diet to promote regular, easy bowel movements.
While hernia repair is generally safe, some complications can arise:
-
Infection: Infection at the surgery site is a possible complication, particularly if proper wound care is not followed.
-
Recurrence: In some cases, the hernia may recur, especially if mesh is not used, or if the patient resumes heavy lifting too soon after surgery.
-
Chronic Pain: Some patients experience long-term discomfort or pain at the surgical site.
-
Injury to Surrounding Organs: Rarely, the surgeon may accidentally damage surrounding organs such as the intestines or bladder during surgery.
-
Blood Clots: Although rare, blood clots may form post-surgery, particularly in
the legs, leading to deep vein thrombosis (DVT).
Post-surgery, most patients recover well and can return to their daily activities within 4-6 weeks. However, lifestyle changes and routine check-ups are necessary to ensure a full recovery and prevent hernia recurrence:
-
Avoid heavy lifting and high-impact activities for several weeks.
-
Maintain a healthy lifestyle with regular exercise, a balanced diet, and proper weight management.
-
Follow up with your doctor for regular check-ups to monitor healing and detect any signs of recurrence early.
With proper care and management, most people can live a full and active life after hernia repair surgery.
1. What is hernia repair surgery?
Hernia repair surgery is a procedure to fix a hernia, which occurs when an internal organ or tissue pushes through a weakened area in the surrounding muscle or connective tissue. The surgery aims to push the protruding tissue back into place and strengthen the muscle or tissue to prevent recurrence.
2. Why do I need hernia repair surgery?
Hernia repair surgery is recommended when a hernia causes pain, swelling, or discomfort, or if it becomes larger over time. If the hernia is incarcerated (cannot be pushed back in) or strangulated (blood flow is cut off), it becomes a medical emergency that requires immediate surgery. Surgery is often necessary if conservative treatments like lifestyle changes or medication don’t work.
3. What are the different types of hernia repair procedures?
There are two main types of hernia repair procedures:
-
Open surgery: A single larger incision is made, and the hernia is repaired. This is the traditional method.
-
Laparoscopic (minimally invasive) surgery: Several small incisions are made, and a camera (laparoscope) is used to guide the repair. This technique typically results in less pain and a faster recovery.
4. What causes a hernia?
Hernias can be caused by a combination of increased pressure in the abdomen and a weakened area in the abdominal wall. Common causes include heavy lifting, obesity, pregnancy, constipation, or a prior surgical incision. Some people may also have a congenital weakness in their muscles that predisposes them to hernias.
5. How long does it take to recover from hernia repair surgery?
Recovery time depends on the type of surgery and individual health. For laparoscopic surgery, most patients can return to light activities within 1 to 2 weeks, with full recovery typically taking about 4 to 6 weeks. Open surgery usually requires a longer recovery period of 4 to 6 weeks before returning to normal activities.
6. What are the risks of hernia repair surgery?
While hernia repair surgery is generally safe, risks include infection, bleeding, injury to surrounding tissues or organs, recurrence of the hernia, and complications from anesthesia. However, these risks are relatively low, especially when performed by an experienced surgeon.
7. Can a hernia come back after surgery?
While the goal of hernia repair surgery is to prevent recurrence, there is a small risk that the hernia may come back, particularly if the repair site weakens over time. Factors such as obesity, heavy lifting, or failure to follow post-operative care instructions can increase the risk of recurrence.
8. Is hernia repair surgery painful?
Some discomfort and pain are expected after hernia repair surgery, particularly in the first few days following the procedure. However, the pain can usually be managed with prescribed pain medication and by following your doctor’s post-operative care instructions. Laparoscopic surgery typically results in less pain than open surgery.
9. What should I expect during the surgery?
Hernia repair surgery is typically performed under general anesthesia, meaning you will be asleep during the procedure. The surgeon will either make a single larger incision (open surgery) or several smaller incisions (laparoscopic surgery) to access the hernia. The protruding tissue will be pushed back into place, and the muscle wall will be reinforced, often with a mesh patch to prevent future hernias.
10. Are there any lifestyle changes I need to make after surgery?
After surgery, you should avoid heavy lifting and strenuous activities for several weeks to allow the area to heal properly. Eating a high-fiber diet to prevent constipation is also important, as straining during bowel movements can put pressure on the healing area. Follow-up visits with your surgeon are essential to monitor recovery and ensure that the hernia doesn’t recur.
The other general procedures are:
Few Major Hospitals for Hernia Repair are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hernia Repair | Hospitals Hernia Repair | Doctors Hernia Repair | Surgery Hernia Repair | Cost Of Hernia Repair | Treatment For Hernia Repair | Destinations For Hernia Repair | Risks Hernia Repair | Hernia Repair India | Hernia Repair Recovery | Hernia Repair Information | Hernia Repair Thailand | Hernia Repair Malaysia | Hernia Repair Abroad | Hernia Repair Overseas | Hernia Repair Low Cost | Hernia Repair Singapore | Herniorrhaphy
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



