Skin cancer is the most common type of cancer, affecting millions of people each year globally. It arises from the uncontrolled growth of skin cells, particularly in areas exposed to the sun, though it can develop anywhere on the body. The skin serves as the body’s first line of defense against harmful environmental elements, but when this protective barrier is compromised, abnormal growth of skin cells can occur, leading to cancer.
Skin cancer includes three main types: Basal Cell Carcinoma (BCC), Squamous Cell Carcinoma (SCC), and Melanoma. BCC and SCC are referred to as non-melanoma skin cancers and are more common, accounting for the majority of cases. However, melanoma is the most aggressive form of skin cancer and can spread to other parts of the body, making early detection and treatment crucial.
Despite being the most frequently diagnosed cancer, skin cancer has one of the highest cure rates when detected early. Through advances in medical treatments and preventive measures, skin cancer can often be treated effectively, leading to high survival rates.
This comprehensive guide covers skin cancer’s causes, risk factors, symptoms, diagnosis, treatment options, and management strategies. By increasing awareness of skin cancer and its warning signs, early detection and better treatment outcomes can be achieved.
Skin cancer is primarily caused by DNA damage to skin cells, particularly by exposure to ultraviolet (UV) radiation. This radiation, whether from the sun or tanning beds, damages the skin’s DNA, triggering mutations that lead to abnormal cell growth and division.
Causes of Skin Cancer:
-
UV Radiation: The main cause of skin cancer is exposure to UV rays from the sun or artificial sources like tanning beds. UV radiation causes changes in the DNA of skin cells, particularly in the basal and squamous layers of the epidermis, which can lead to cancerous growths.
-
UVA Rays: These rays penetrate deeper into the skin and are associated with premature aging and DNA damage that contributes to skin cancer.
-
UVB Rays: These rays are responsible for sunburn and are known to directly damage DNA, causing mutations that can lead to skin cancer.
-
-
Genetic Mutations: Skin cells can accumulate genetic mutations that lead to uncontrolled cell growth. These mutations may occur due to UV radiation exposure or can be inherited from family members who have certain gene mutations (e.g., mutations in the p53 tumor suppressor gene).
-
Environmental and Chemical Exposure: Long-term exposure to certain chemicals, including industrial solvents, coal tars, and pesticides, increases the risk of skin cancer. Occupations like farming, mining, and construction may involve such exposures.
-
Chronic Inflammation: Conditions such as chronic dermatitis or chronic sunburn increase the risk of developing skin cancer in the affected areas due to ongoing DNA damage and inflammation.
Risk Factors for Skin Cancer:
While skin cancer can occur in anyone, several factors increase the risk of developing the disease. These include both genetic and environmental factors:
-
Skin Type and Pigmentation: Fair skin, light eyes, and red or blonde hair are associated with a higher risk of skin cancer. People with less melanin, the pigment that provides some protection against UV radiation, are more vulnerable to UV damage.
-
Family History: Having a family history of skin cancer, especially melanoma, significantly increases the risk of developing the disease. Certain inherited genetic mutations can predispose individuals to skin cancer.
-
Age: Skin cancer risk increases with age, particularly in people aged 50 and older, as cumulative sun exposure over a lifetime increases the chances of DNA damage.
-
Previous Skin Cancer: If you have had skin cancer once, you are at higher risk of developing it again, particularly in other areas of the skin.
-
Tanning Bed Use: The use of tanning beds is a major risk factor, especially for young people. Tanning beds emit concentrated UV radiation, which increases the likelihood of developing skin cancer later in life.
-
Weakened Immune System: Conditions like HIV/AIDS, or immunosuppressive drugs used for organ transplants, can weaken the immune system and increase the risk of skin cancer.
Skin cancer symptoms can vary depending on the type and stage of the cancer. While early skin cancer is often asymptomatic, noticeable changes in the skin are typically the first signs of the disease.
Early Symptoms of Skin Cancer:
-
New or Changing Moles: A new mole or a change in an existing mole’s size, shape, or color is one of the most common early signs of skin cancer.
-
Asymmetry: A mole or growth that is uneven in shape or does not have symmetrical borders may indicate melanoma.
-
Irregular Borders: Moles or lesions with jagged, blurred, or irregular edges may be suspicious.
-
Color Variation: A mole that has multiple colors (shades of brown, black, pink, white, or red) may be an early warning sign of melanoma.
-
Size Changes: A mole that continues to grow or exceed the size of a pencil eraser (about 6mm) should be examined by a healthcare professional.
-
Itching or Tenderness: Some skin cancers may cause the skin to itch, bleed, or become tender to the touch.
Later Symptoms:
-
Pain: If skin cancer spreads or if the tumor grows deeper into the skin, it may cause pain, discomfort, or sensitivity.
-
Bleeding or Crusting: A lesion that bleeds, crusts over, or doesn’t heal could be a sign of advanced skin cancer.
-
Open Sores: Skin cancers like basal cell carcinoma or squamous cell carcinoma may create sores that do not heal.
-
Changes in Sensation: Numbness, tingling, or a feeling of tightness around the skin cancer may occur if the tumor presses on nerves.
Specific Signs for Different Types of Skin Cancer:
-
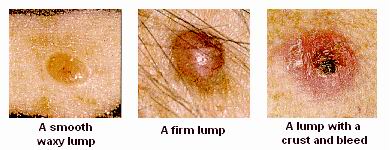
Basal Cell Carcinoma (BCC): BCC often appears as a small, shiny bump or a flat, pink area of skin that may bleed or form a scab.
-
Squamous Cell Carcinoma (SCC): SCC may appear as a red, scaly bump, ulcer, or a flat lesion with a crusty surface.
-
Melanoma: Melanoma may appear as a large, dark, irregularly shaped mole or growth. It may evolve over time, showing significant changes in shape, size, and color.
A thorough diagnosis of skin cancer is essential to determine the type, stage, and best course of treatment. The diagnostic process typically includes a physical examination, medical history review, and various tests.
Diagnostic Methods:
-
Skin Examination: The first step in diagnosing skin cancer is a full-body skin examination by a dermatologist, who will inspect all areas of the skin, including less visible areas like the scalp and between the toes.
-
Dermatoscopy: A dermatoscope is a specialized magnifying tool that allows the dermatologist to closely examine suspicious moles or skin lesions, often revealing more details than the naked eye can see.
-
Skin Biopsy: A biopsy is the gold standard for diagnosing skin cancer. A small sample of the skin lesion is removed and examined under a microscope to identify cancer cells.
-
Shave Biopsy: The surface layer of the tumor is shaved off for examination.
-
Punch Biopsy: A small, circular portion of the lesion is removed for deeper analysis.
-
Excisional Biopsy: The entire mole or lesion is excised for a more comprehensive assessment.
-
-
Lymph Node Biopsy: If skin cancer has spread to nearby lymph nodes, a biopsy of the lymph node may be performed to determine the extent of cancer spread.
-
Imaging Tests: In cases of advanced skin cancer, imaging tests such as CT scans, MRI, or PET scans may be used to check for cancer spread to other organs.
Treatment for skin cancer depends on the type, size, location, and stage of the cancer. Early-stage skin cancers are often highly treatable, and the treatment goal is to remove the tumor and prevent further growth.
Common Treatment Options:
-
Surgical Excision: The most common treatment for skin cancer is surgical removal of the tumor, along with a small margin of healthy tissue to ensure all cancerous cells are removed.
-
Mohs Surgery: A specialized surgical technique where thin layers of the skin are removed and examined under a microscope until no cancer cells remain. This is typically used for BCC and SCC, especially in areas where tissue preservation is crucial (e.g., face, ears).
-
Radiation Therapy: Radiation therapy is often used when surgery is not an option or to treat areas where cancer cells may remain. It is also used for cancers that have spread to other areas.
-
Cryotherapy: Cryotherapy involves freezing the skin cancer with liquid nitrogen, which destroys cancer cells. It is most commonly used for precancerous lesions or early-stage skin cancers.
-
Topical Chemotherapy: Topical creams like Imiquimod (Aldara) or 5-fluorouracil (5-FU) can be used to treat superficial skin cancers, including actinic keratosis or superficial BCC.
-
Photodynamic Therapy (PDT): PDT uses a photosensitizing agent applied to the skin followed by light exposure to destroy cancer cells.
-
Immunotherapy: Checkpoint inhibitors or other immunotherapy drugs, such as Pembrolizumab (Keytruda), may be used to treat advanced melanoma by stimulating the immune system to attack cancer cells.
While it is not always possible to prevent skin cancer, lifestyle changes and proactive measures can help reduce the risk and improve the management of the disease.
Preventive Measures:
-
Sun Protection: Avoid sun exposure between 10 a.m. and 4 p.m., when UV rays are the strongest. Always wear a broad-spectrum sunscreen with SPF 30 or higher and reapply every two hours.
-
Protective Clothing: Wear wide-brimmed hats, sunglasses, and protective clothing when outside.
-
Avoid Tanning Beds: Never use tanning beds or sunlamps, as they significantly increase the risk of skin cancer.
-
Regular Skin Checks: Perform monthly self-skin exams and schedule regular skin check-ups with a dermatologist, especially if you have a family history of skin cancer.
Managing Skin Cancer:
-
Follow-Up Care: After treatment, regular follow-up visits are essential to monitor for recurrence or new skin cancers.
-
Emotional and Psychological Support: A cancer diagnosis can have emotional and psychological impacts. Counseling, support groups, and stress management can improve quality of life during and after treatment.
While skin cancer is often treatable, complications can arise, especially in more advanced stages or aggressive forms like melanoma.
Potential Complications:
-
Recurrence: Skin cancer can return after treatment, particularly in people with a history of multiple skin cancers.
-
Metastasis: Melanoma, if not treated early, can spread to other parts of the body, including lymph nodes, liver, lungs, and brain.
-
Scarring: Surgical removal of skin cancer can lead to scarring, particularly in sensitive or visible areas like the face.
-
Lymphedema: If lymph nodes are removed during surgery, it can result in lymphedema, or swelling, in the affected limb or area.
Living with skin cancer requires ongoing monitoring, emotional support, and lifestyle adjustments to ensure the best quality of life post-treatment.
Coping with Skin Cancer:
-
Physical Rehabilitation: Skin cancer treatment may affect mobility or self-image, but rehabilitation and support can help improve confidence and physical well-being.
-
Psychosocial Support: Support groups, counseling, or therapy can help patients and families manage the emotional toll of cancer diagnosis and treatment.
-
Long-Term Monitoring: Regular check-ups, skin exams, and self-monitoring are key to detecting recurrence early and managing long-term health.
1. What is Skin Cancer?
Skin cancer is a type of cancer that begins in the cells of the skin. It occurs when abnormal cells in the skin grow uncontrollably, forming a tumor. The most common types of skin cancer are basal cell carcinoma, squamous cell carcinoma, and melanoma. Skin cancer is often caused by prolonged exposure to ultraviolet (UV) radiation from the sun or tanning beds, which damages the skin cells and leads to cancer.
2. What are the types of Skin Cancer?
The three most common types of skin cancer are:
-
Basal Cell Carcinoma (BCC): The most common and least dangerous form of skin cancer. It typically grows slowly and is highly treatable if detected early.
-
Squamous Cell Carcinoma (SCC): A more aggressive form of skin cancer that can spread to other parts of the body if not treated. It often appears as scaly, red patches or sores.
-
Melanoma: The most serious type of skin cancer, melanoma develops in the melanocytes, the cells that produce pigment. It can spread rapidly to other organs if not caught early.
3. What are the risk factors for Skin Cancer?
Several factors can increase the risk of developing skin cancer, including:
-
Excessive sun exposure or tanning bed use
-
Fair skin, light hair, and light eyes, which have less natural protection from UV radiation
-
A history of sunburns, especially during childhood
-
Family history of skin cancer or melanoma
-
Weakened immune system due to certain medical conditions or medications
-
Presence of many moles or abnormal moles, which can be more prone to developing into melanoma
4. How can I prevent Skin Cancer?
Skin cancer can often be prevented by taking measures to protect your skin from UV radiation. Recommended prevention strategies include:
-
Using sunscreen with broad-spectrum (UVA and UVB) protection and a SPF of 30 or higher
-
Wearing protective clothing such as hats, sunglasses, and long sleeves
-
Avoiding tanning beds
-
Seeking shade during peak sunlight hours (10 a.m. to 4 p.m.)
-
Regularly checking your skin for new or changing moles, and consulting a dermatologist for any concerns
-
Getting regular skin checks from a healthcare professional, especially if you have risk factors for skin cancer
5. What are the signs and symptoms of Skin Cancer?
Skin cancer may present itself in different ways depending on the type. Common signs and symptoms include:
-
Changes in the appearance of a mole: It may become larger, change color, or have irregular borders.
-
A new growth or bump on the skin that doesn’t heal.
-
Itching, tenderness, or pain at the site of the lesion.
-
Bleeding or oozing from a mole or growth.
For melanoma, the ABCDE rule is often used to evaluate moles: -
Asymmetry
-
Border irregularity
-
Color variation
-
Diameter greater than 6 mm
-
Evolving or changing over time
6. How is Skin Cancer diagnosed?
Skin cancer is usually diagnosed through a skin examination by a dermatologist. If a suspicious area is identified, a skin biopsy may be performed, where a small sample of the suspicious tissue is removed and sent to a lab for testing. Imaging tests, such as CT scans or MRIs, may be used if the cancer is suspected to have spread beyond the skin.
7. How is Skin Cancer treated?
Treatment for skin cancer depends on the type and stage of the disease. Common treatment options include:
-
Surgical excision: The cancerous tissue is surgically removed.
-
Mohs surgery: A precise, layer-by-layer removal of skin cancer cells, often used for BCC and SCC.
-
Cryotherapy: Freezing the cancerous tissue to destroy it, commonly used for superficial skin cancers.
-
Radiation therapy: High-energy radiation is used to target cancer cells, typically for non-surgical candidates or advanced cases.
-
Topical treatments: Medications applied directly to the skin, such as creams or ointments.
-
Immunotherapy and targeted therapy: New treatments that boost the immune system or target cancer cells specifically, often used for advanced melanoma.
8. What is the prognosis for Skin Cancer?
The prognosis for skin cancer depends on the type of cancer, its stage, and how early it is detected. Basal cell carcinoma and squamous cell carcinoma have high cure rates when treated early, and the survival rate is generally excellent. Melanoma, however, can be more aggressive and may spread to other parts of the body. Early detection and treatment significantly improve the prognosis for melanoma, with a high survival rate if detected before it spreads.
9. Can Skin Cancer spread to other parts of the body?
While basal cell carcinoma and squamous cell carcinoma typically remain localized and rarely spread to other parts of the body, melanoma can be much more aggressive and has the potential to spread to other organs, such as the liver, lungs, and brain. This is why early detection and treatment of melanoma are crucial for improving survival rates.
10. How often should I get checked for Skin Cancer?
It’s important to regularly check your skin for any changes, especially if you have risk factors for skin cancer. Self-exams should be done monthly to identify any new or changing moles. Additionally, annual skin checks by a dermatologist are recommended for individuals at higher risk, including those with a history of skin cancer, numerous moles, or a family history of skin cancer. Early detection is key to successful treatment.
The other Oncology Procedures are
Few Major Hospitals for treatment of Small Cell Lung Cancer are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



