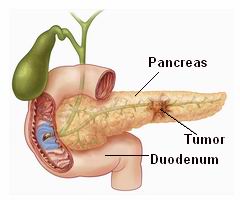
Pancreatic cancer is a highly aggressive cancer that originates in the pancreas, an essential organ located behind the stomach. The pancreas plays a vital role in both digestive and endocrine functions: it produces digestive enzymes and insulin. However, pancreatic cancer disrupts these functions by causing abnormal growth of cells in the pancreas. As the disease progresses, it can lead to severe complications, including damage to surrounding organs and systems.
The most common type of pancreatic cancer is exocrine pancreatic cancer, which accounts for around 95% of cases and typically originates in the ductal cells. There is also a rare form called endocrine pancreatic cancer (or pancreatic neuroendocrine tumors), which originates in hormone-producing cells of the pancreas.
Pancreatic cancer is notorious for being difficult to diagnose early because symptoms often do not appear until the cancer has advanced. By the time it is detected, the disease is often at an advanced stage, contributing to its poor prognosis. Despite advancements in medical treatment, the survival rate for pancreatic cancer remains low, making early detection and innovative therapies critical for improving patient outcomes.
This comprehensive guide will explore the causes, risk factors, symptoms, diagnosis, treatment options, management strategies, and the living experience with pancreatic cancer, providing valuable insights for patients, families, and caregivers.
Pancreatic cancer typically develops when cells in the pancreas undergo genetic mutations that disrupt normal cell growth and division. Several factors can influence the likelihood of developing these mutations, including genetic predisposition, environmental exposures, and lifestyle factors.
Causes of Pancreatic Cancer
-
Genetic Mutations:
-
The genetic changes that cause pancreatic cancer may occur in specific
genes responsible for regulating cell growth. The most commonly altered
genes in pancreatic cancer include KRAS,
TP53, CDKN2A, and
SMAD4. These mutations disrupt cell cycle regulation,
leading to the uncontrolled growth of abnormal cells in the pancreas.
-
Chronic Inflammation:
-
Conditions that cause chronic inflammation in the
pancreas, such as chronic pancreatitis, can increase
the risk of pancreatic cancer. Prolonged inflammation damages pancreatic
cells, promoting mutations that can lead to cancer development.
-
Family History and Inherited Genetic Mutations:
-
A family history of pancreatic cancer increases the risk of developing
the disease. Genetic conditions such as BRCA1 and BRCA2
mutations, Lynch syndrome, and
Peutz-Jeghers syndrome have all been linked to a higher
risk of developing pancreatic cancer.
-
Immune System Dysfunction:
-
Patients with autoimmune diseases or those with
immune system deficiencies may have a higher likelihood
of developing pancreatic cancer. The body's inability to regulate immune
responses can promote inflammation and cell mutations that contribute to
cancer development.
Risk Factors for Pancreatic Cancer
-
Age:
-
Age is one of the most significant risk factors for pancreatic cancer. It
is most commonly diagnosed in individuals over the age of
60, with the highest incidence in those over 70. The
risk increases as people age, likely due to the accumulation of genetic
mutations over time.
-
Gender:
-
Men are at a higher risk of developing pancreatic cancer than women. This
may be due to genetic, hormonal, or lifestyle factors. However, the
gender gap in incidence is narrowing.
-
Tobacco Use:
-
Smoking is the most significant modifiable risk factor
for pancreatic cancer. Smokers are twice as likely to
develop pancreatic cancer compared to non-smokers. The carcinogens in
tobacco smoke damage the DNA in pancreatic cells, leading to cancer.
-
Obesity and Diet:
-
Obesity is a well-established risk factor for pancreatic
cancer. Excess body fat promotes inflammation and insulin resistance,
both of which can increase the risk of cancer development. A diet high
in red and processed meats, sugary foods, and low in fruits and
vegetables is associated with a higher risk of pancreatic cancer.
-
Diabetes:
-
Type 2 diabetes, particularly when it is poorly
controlled, is linked to an increased risk of pancreatic cancer.
Diabetes contributes to chronic inflammation and altered glucose
metabolism, which can influence the growth of cancerous cells in the
pancreas.
-
Chemical and Environmental Exposure:
-
Long-term exposure to toxic chemicals, such as those
found in pesticides, herbicides, and
petroleum products, may increase the risk of pancreatic
cancer. Individuals working in industries involving chemicals or heavy
machinery may be at greater risk.
-
Chronic Pancreatitis:
-
Chronic pancreatitis is a long-term inflammation of the
pancreas, often caused by heavy alcohol use, gallstones, or other
conditions. It increases the risk of pancreatic cancer by causing damage
to the pancreas, leading to cell mutations over time.
Genetic Mutations:
-
The genetic changes that cause pancreatic cancer may occur in specific genes responsible for regulating cell growth. The most commonly altered genes in pancreatic cancer include KRAS, TP53, CDKN2A, and SMAD4. These mutations disrupt cell cycle regulation, leading to the uncontrolled growth of abnormal cells in the pancreas.
Chronic Inflammation:
-
Conditions that cause chronic inflammation in the pancreas, such as chronic pancreatitis, can increase the risk of pancreatic cancer. Prolonged inflammation damages pancreatic cells, promoting mutations that can lead to cancer development.
Family History and Inherited Genetic Mutations:
-
A family history of pancreatic cancer increases the risk of developing the disease. Genetic conditions such as BRCA1 and BRCA2 mutations, Lynch syndrome, and Peutz-Jeghers syndrome have all been linked to a higher risk of developing pancreatic cancer.
Immune System Dysfunction:
-
Patients with autoimmune diseases or those with immune system deficiencies may have a higher likelihood of developing pancreatic cancer. The body's inability to regulate immune responses can promote inflammation and cell mutations that contribute to cancer development.
-
Age:
-
Age is one of the most significant risk factors for pancreatic cancer. It is most commonly diagnosed in individuals over the age of 60, with the highest incidence in those over 70. The risk increases as people age, likely due to the accumulation of genetic mutations over time.
-
-
Gender:
-
Men are at a higher risk of developing pancreatic cancer than women. This may be due to genetic, hormonal, or lifestyle factors. However, the gender gap in incidence is narrowing.
-
-
Tobacco Use:
-
Smoking is the most significant modifiable risk factor for pancreatic cancer. Smokers are twice as likely to develop pancreatic cancer compared to non-smokers. The carcinogens in tobacco smoke damage the DNA in pancreatic cells, leading to cancer.
-
-
Obesity and Diet:
-
Obesity is a well-established risk factor for pancreatic cancer. Excess body fat promotes inflammation and insulin resistance, both of which can increase the risk of cancer development. A diet high in red and processed meats, sugary foods, and low in fruits and vegetables is associated with a higher risk of pancreatic cancer.
-
-
Diabetes:
-
Type 2 diabetes, particularly when it is poorly controlled, is linked to an increased risk of pancreatic cancer. Diabetes contributes to chronic inflammation and altered glucose metabolism, which can influence the growth of cancerous cells in the pancreas.
-
-
Chemical and Environmental Exposure:
-
Long-term exposure to toxic chemicals, such as those found in pesticides, herbicides, and petroleum products, may increase the risk of pancreatic cancer. Individuals working in industries involving chemicals or heavy machinery may be at greater risk.
-
-
Chronic Pancreatitis:
-
Chronic pancreatitis is a long-term inflammation of the pancreas, often caused by heavy alcohol use, gallstones, or other conditions. It increases the risk of pancreatic cancer by causing damage to the pancreas, leading to cell mutations over time.
-
The early stages of pancreatic cancer often do not cause noticeable symptoms, making it difficult to detect in its initial phases. When symptoms do appear, they are often vague and may be mistaken for other gastrointestinal issues. As the cancer progresses, however, it can cause a variety of specific signs and symptoms.
Early Symptoms:
-
Jaundice:
-
Yellowing of the skin and eyes (jaundice) is one of the
most common early symptoms of pancreatic cancer. This occurs when the
tumor obstructs the bile duct, preventing bile from
draining properly from the liver. As a result,
bilirubin accumulates in the bloodstream, leading to
jaundice.
-
Abdominal Pain:
-
Pain or discomfort in the upper abdomen or back is another common
symptom. The pain may start as a dull ache and progressively worsen as
the tumor grows and presses against surrounding tissues and organs.
-
Unexplained Weight Loss:
-
Significant weight loss without changes in diet or exercise is a hallmark
of pancreatic cancer. This occurs due to a combination of loss
of appetite, digestive problems, and the
body's increased metabolic demand as it fights cancer.
-
Loss of Appetite:
-
Many individuals with pancreatic cancer experience a loss of
appetite, which can be due to the tumor’s impact on
digestion or the general fatigue associated with the
disease.
-
Nausea and Vomiting:
-
Nausea and vomiting are common symptoms, especially if the tumor
obstructs the gastrointestinal tract or bile duct,
making it difficult for food to pass through the stomach and intestines.
Advanced Symptoms:
-
Fatigue:
-
Chronic fatigue is a common symptom of pancreatic cancer. This may result
from anemia (low red blood cell count),
malnutrition, or the body’s response to cancer.
-
Dark Urine and Light-Colored Stools:
-
Dark urine and pale stools are often signs of bile duct
obstruction due to a pancreatic tumor. The obstruction
leads to a buildup of bile, which can affect both the color of the stool
and urine.
-
New-Onset Diabetes:
-
Type 2 diabetes that develops suddenly, especially in
older adults without a prior history of the disease, can be a warning
sign of pancreatic cancer. This happens when the tumor interferes with
the pancreas’ ability to produce insulin.
Jaundice:
-
Yellowing of the skin and eyes (jaundice) is one of the most common early symptoms of pancreatic cancer. This occurs when the tumor obstructs the bile duct, preventing bile from draining properly from the liver. As a result, bilirubin accumulates in the bloodstream, leading to jaundice.
Abdominal Pain:
-
Pain or discomfort in the upper abdomen or back is another common symptom. The pain may start as a dull ache and progressively worsen as the tumor grows and presses against surrounding tissues and organs.
Unexplained Weight Loss:
-
Significant weight loss without changes in diet or exercise is a hallmark of pancreatic cancer. This occurs due to a combination of loss of appetite, digestive problems, and the body's increased metabolic demand as it fights cancer.
Loss of Appetite:
-
Many individuals with pancreatic cancer experience a loss of appetite, which can be due to the tumor’s impact on digestion or the general fatigue associated with the disease.
Nausea and Vomiting:
-
Nausea and vomiting are common symptoms, especially if the tumor obstructs the gastrointestinal tract or bile duct, making it difficult for food to pass through the stomach and intestines.
-
Fatigue:
-
Chronic fatigue is a common symptom of pancreatic cancer. This may result from anemia (low red blood cell count), malnutrition, or the body’s response to cancer.
-
-
Dark Urine and Light-Colored Stools:
-
Dark urine and pale stools are often signs of bile duct obstruction due to a pancreatic tumor. The obstruction leads to a buildup of bile, which can affect both the color of the stool and urine.
-
-
New-Onset Diabetes:
-
Type 2 diabetes that develops suddenly, especially in older adults without a prior history of the disease, can be a warning sign of pancreatic cancer. This happens when the tumor interferes with the pancreas’ ability to produce insulin.
-
Diagnosing pancreatic cancer typically involves a combination of imaging tests, blood tests, and a biopsy to confirm the presence of cancer and assess the extent of the disease. Early diagnosis can be challenging due to the lack of specific symptoms and the location of the pancreas.
Diagnostic Steps:
-
Medical History and Physical Examination:
-
The doctor will ask about the patient's symptoms, risk factors, and
medical history. A physical exam will help identify signs of
jaundice or abdominal masses that may
indicate pancreatic cancer.
-
Blood Tests:
-
Tumor markers: A blood test to measure levels of
CA 19-9, a tumor marker that is often elevated in
pancreatic cancer patients. However, this marker is not specific, and
elevated levels can also occur in other cancers and conditions.
-
Liver function tests: Blood tests can check for signs of
liver dysfunction or bile duct
obstruction, both of which can be caused by pancreatic
tumors.
-
Imaging Studies:
-
CT Scan (Computed Tomography): A CT scan provides
detailed images of the pancreas and surrounding organs, helping to
identify tumors, their size, and whether cancer has spread to other
areas.
-
MRI (Magnetic Resonance Imaging): An MRI is used for
further evaluation of the pancreas, bile ducts, and surrounding tissues.
It provides detailed images without the use of radiation.
-
Ultrasound: An abdominal ultrasound is a non-invasive
test that uses sound waves to detect tumors in the pancreas and
surrounding organs.
-
Endoscopic Ultrasound (EUS): This test involves
inserting a small ultrasound probe through the
endoscope into the stomach, allowing for detailed
imaging of the pancreas and the ability to perform a biopsy.
-
Biopsy:
-
A needle biopsy involves removing a small tissue sample
from the pancreas, guided by imaging techniques like ultrasound or CT
scan. This is the definitive method for diagnosing pancreatic cancer.
Medical History and Physical Examination:
-
The doctor will ask about the patient's symptoms, risk factors, and medical history. A physical exam will help identify signs of jaundice or abdominal masses that may indicate pancreatic cancer.
Blood Tests:
-
Tumor markers: A blood test to measure levels of CA 19-9, a tumor marker that is often elevated in pancreatic cancer patients. However, this marker is not specific, and elevated levels can also occur in other cancers and conditions.
-
Liver function tests: Blood tests can check for signs of liver dysfunction or bile duct obstruction, both of which can be caused by pancreatic tumors.
Imaging Studies:
-
CT Scan (Computed Tomography): A CT scan provides detailed images of the pancreas and surrounding organs, helping to identify tumors, their size, and whether cancer has spread to other areas.
-
MRI (Magnetic Resonance Imaging): An MRI is used for further evaluation of the pancreas, bile ducts, and surrounding tissues. It provides detailed images without the use of radiation.
-
Ultrasound: An abdominal ultrasound is a non-invasive test that uses sound waves to detect tumors in the pancreas and surrounding organs.
-
Endoscopic Ultrasound (EUS): This test involves inserting a small ultrasound probe through the endoscope into the stomach, allowing for detailed imaging of the pancreas and the ability to perform a biopsy.
Biopsy:
-
A needle biopsy involves removing a small tissue sample from the pancreas, guided by imaging techniques like ultrasound or CT scan. This is the definitive method for diagnosing pancreatic cancer.
The treatment for pancreatic cancer depends on the stage of the disease, the location of the tumor, and the patient’s overall health. Treatment options aim to control the disease, relieve symptoms, and improve quality of life.
Treatment Modalities:
-
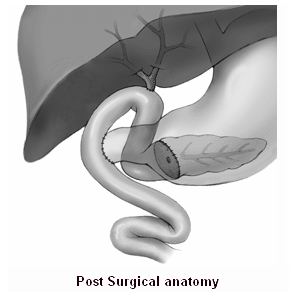
Surgery:
-
Surgery is the primary option for resectable pancreatic cancer. The most
common procedure is the Whipple procedure, which
involves removing the head of the pancreas, part of the small intestine,
bile duct, and sometimes the gallbladder.
-
If the cancer is located in the tail or body of the pancreas, a
distal pancreatectomy may be performed to remove those
parts of the pancreas.
-
In advanced cases, surgery may not be possible, and palliative
surgery may be performed to relieve symptoms such as
bile duct obstruction.
-
Chemotherapy:
-
Chemotherapy is often used after surgery (adjuvant therapy) to kill any
remaining cancer cells. It is also used for advanced pancreatic
cancer to shrink tumors and alleviate symptoms.
-
Drugs like gemcitabine, FOLFIRINOX, and
nab-paclitaxel are commonly used to treat pancreatic
cancer.
-
Radiation Therapy:
-
Radiation therapy is used in combination with chemotherapy to treat
localized pancreatic cancer. It may also be used to shrink tumors before
surgery or to relieve pain and other symptoms in advanced stages.
-
Targeted Therapy:
-
Targeted therapies such as erlotinib (Tarceva) target
specific molecules involved in the growth and survival of cancer cells.
These therapies aim to block the signals that promote cancer cell
division.
-
Immunotherapy:
-
Immunotherapy, such as immune checkpoint inhibitors, is
an emerging treatment for pancreatic cancer. These therapies aim to
enhance the body’s immune system to recognize and destroy cancer cells.
Surgery:
-
Surgery is the primary option for resectable pancreatic cancer. The most common procedure is the Whipple procedure, which involves removing the head of the pancreas, part of the small intestine, bile duct, and sometimes the gallbladder.
-
If the cancer is located in the tail or body of the pancreas, a distal pancreatectomy may be performed to remove those parts of the pancreas.
-
In advanced cases, surgery may not be possible, and palliative surgery may be performed to relieve symptoms such as bile duct obstruction.
Chemotherapy:
-
Chemotherapy is often used after surgery (adjuvant therapy) to kill any remaining cancer cells. It is also used for advanced pancreatic cancer to shrink tumors and alleviate symptoms.
-
Drugs like gemcitabine, FOLFIRINOX, and nab-paclitaxel are commonly used to treat pancreatic cancer.
Radiation Therapy:
-
Radiation therapy is used in combination with chemotherapy to treat localized pancreatic cancer. It may also be used to shrink tumors before surgery or to relieve pain and other symptoms in advanced stages.
Targeted Therapy:
-
Targeted therapies such as erlotinib (Tarceva) target specific molecules involved in the growth and survival of cancer cells. These therapies aim to block the signals that promote cancer cell division.
Immunotherapy:
-
Immunotherapy, such as immune checkpoint inhibitors, is an emerging treatment for pancreatic cancer. These therapies aim to enhance the body’s immune system to recognize and destroy cancer cells.
While pancreatic cancer cannot always be prevented, certain lifestyle changes and early detection strategies can help reduce risk and improve treatment outcomes.
Prevention Strategies:
-
Quit Smoking: Since smoking is the leading cause of pancreatic
cancer, quitting can significantly reduce your risk.
-
Maintain a Healthy Weight: Keeping a healthy weight and avoiding
obesity can lower your risk of developing pancreatic cancer.
-
Dietary Adjustments: A diet rich in fruits, vegetables, and
whole grains can lower the risk, while limiting red and processed meats can be
beneficial.
-
Exercise Regularly: Engaging in physical activity is linked to a
reduced risk of pancreatic cancer.
Management of Pancreatic Cancer:
-
Palliative Care: Palliative treatments help manage pain, nausea,
and other symptoms in patients with advanced pancreatic cancer.
-
Chemotherapy and Radiotherapy: Regular chemotherapy and
radiation sessions can help shrink tumors and prevent them from spreading.
-
Pain Management: Specialized medications, including opioids and
nerve blockers, may be required to manage chronic pain associated with
pancreatic cancer.
Quit Smoking: Since smoking is the leading cause of pancreatic cancer, quitting can significantly reduce your risk.
Maintain a Healthy Weight: Keeping a healthy weight and avoiding obesity can lower your risk of developing pancreatic cancer.
Dietary Adjustments: A diet rich in fruits, vegetables, and whole grains can lower the risk, while limiting red and processed meats can be beneficial.
Exercise Regularly: Engaging in physical activity is linked to a reduced risk of pancreatic cancer.
-
Palliative Care: Palliative treatments help manage pain, nausea, and other symptoms in patients with advanced pancreatic cancer.
-
Chemotherapy and Radiotherapy: Regular chemotherapy and radiation sessions can help shrink tumors and prevent them from spreading.
-
Pain Management: Specialized medications, including opioids and nerve blockers, may be required to manage chronic pain associated with pancreatic cancer.
As pancreatic cancer progresses, it can cause various complications that significantly affect the patient’s health and quality of life. These complications include:
-
Bile Duct Obstruction:
-
Tumors in the pancreas can block the bile duct, leading to jaundice, pain, and digestive issues.
-
-
Weight Loss:
-
Significant weight loss and malnutrition often occur in the later stages of pancreatic cancer due to poor nutrient absorption and the body's increased energy requirements.
-
-
Infections:
-
Pancreatic cancer weakens the immune system, making patients more susceptible to infections, particularly respiratory infections and urinary tract infections.
-
-
Blood Clots:
-
Pancreatic cancer patients are at higher risk of developing blood clots in the veins, which can lead to complications such as deep vein thrombosis (DVT) or pulmonary embolism.
-
Living with pancreatic cancer is challenging, but with the right treatment, support, and coping strategies, many patients can manage the disease effectively. While pancreatic cancer is difficult to treat, advancements in chemotherapy, radiation, and immunotherapy provide hope for improved survival rates and better quality of life.
Coping with the Emotional Impact:
-
Cancer affects not just the body but also the mind. It’s crucial
for patients to seek psychological support, whether through
counseling, support groups, or family
therapy.
Managing Physical Symptoms:
-
Pain management and nutrition are key to
maintaining quality of life. Patients should work with a healthcare provider to
develop a comprehensive care plan that addresses their physical, emotional, and
mental health needs.
Cancer affects not just the body but also the mind. It’s crucial for patients to seek psychological support, whether through counseling, support groups, or family therapy.
-
Pain management and nutrition are key to maintaining quality of life. Patients should work with a healthcare provider to develop a comprehensive care plan that addresses their physical, emotional, and mental health needs.
1. What is Pancreatic Cancer?
Pancreatic cancer is a type of cancer that begins in the pancreas, an organ located behind the stomach. The pancreas plays a key role in digestion and blood sugar regulation. Pancreatic cancer occurs when abnormal cells in the pancreas begin to grow uncontrollably, forming a tumor. It is often diagnosed at advanced stages due to its subtle symptoms in the early stages.
2. What are the symptoms of Pancreatic Cancer?
The symptoms of pancreatic cancer can vary depending on the tumor's location and stage of the disease. Common symptoms include:
-
Jaundice (yellowing of the skin or eyes)
-
Abdominal pain or discomfort, often in the upper abdomen or back
-
Unexplained weight loss
-
Loss of appetite
-
Nausea or vomiting
-
Fatigue
-
New-onset diabetes or changes in blood sugar levels
Since these symptoms can be attributed to other conditions, pancreatic cancer is often diagnosed in later stages.
3. What are the risk factors for Pancreatic Cancer?
Several factors can increase the risk of developing pancreatic cancer, including:
-
Age: The risk increases after the age of 60.
-
Smoking: Smoking is a significant risk factor for pancreatic cancer.
-
Family history: A family history of pancreatic cancer or certain genetic conditions increases the risk.
-
Chronic pancreatitis: Long-term inflammation of the pancreas may increase risk.
-
Diabetes: People with long-standing diabetes are at higher risk.
-
Obesity: Being overweight or obese is associated with an increased risk of pancreatic cancer.
-
Genetic mutations: Inherited gene mutations can predispose individuals to pancreatic cancer.
4. How is Pancreatic Cancer diagnosed?
Pancreatic cancer is diagnosed through a combination of tests, including:
-
Imaging tests: CT scans, MRI scans, or ultrasounds are commonly used to detect tumors in the pancreas.
-
Biopsy: A tissue sample may be taken from the tumor to confirm the presence of cancer cells.
-
Blood tests: Tests such as the CA 19-9 tumor marker test can help detect pancreatic cancer, though it is not definitive.
-
Endoscopic procedures: An endoscopy or endoscopic ultrasound may be used to obtain a closer look at the pancreas.
5. What are the stages of Pancreatic Cancer?
Pancreatic cancer is typically staged as follows:
-
Stage 1: The cancer is confined to the pancreas and is small.
-
Stage 2: The cancer may have spread to nearby tissues or lymph nodes.
-
Stage 3: The cancer has spread to larger areas around the pancreas, including major blood vessels.
-
Stage 4: The cancer has spread to distant organs such as the liver, lungs, or peritoneum (lining of the abdominal cavity).
The stage of the cancer helps determine the treatment options and the prognosis.
6. What are the treatment options for Pancreatic Cancer?
Treatment for pancreatic cancer depends on the stage of the disease, the location of the tumor, and the patient's overall health. Common treatment options include:
-
Surgery: If the tumor is localized and operable, surgical removal of the tumor or the entire pancreas (pancreaticoduodenectomy or Whipple procedure) may be performed.
-
Chemotherapy: Chemotherapy uses drugs to kill cancer cells and is often used in conjunction with surgery or for advanced cancer.
-
Radiation therapy: High-energy radiation is used to shrink tumors and alleviate symptoms.
-
Targeted therapy: Drugs that target specific proteins or genes involved in cancer growth.
-
Immunotherapy: Uses the body’s immune system to fight cancer cells.
In advanced stages, palliative care may be used to manage symptoms and improve quality of life.
7. Is surgery an option for all patients with Pancreatic Cancer?
Surgery is only an option for patients whose tumors are confined to the pancreas and have not spread to other organs or vital structures. This is more common in the early stages of pancreatic cancer. In cases where the cancer is too advanced or involves distant metastasis, surgery may not be recommended. For patients with inoperable tumors, other treatments like chemotherapy or radiation may be used to shrink the tumor and relieve symptoms.
8. What is the prognosis for Pancreatic Cancer?
The prognosis for pancreatic cancer depends on the stage at which it is diagnosed. Unfortunately, pancreatic cancer is often diagnosed at an advanced stage, which makes it more difficult to treat. The 5-year survival rate for all stages combined is low, but if diagnosed early and treated with surgery, the prognosis can improve significantly. Ongoing research into new treatments, such as targeted therapy and immunotherapy, holds promise for improving outcomes in the future.
9. Can lifestyle changes help prevent Pancreatic Cancer?
While there is no guaranteed way to prevent pancreatic cancer, certain lifestyle changes can lower the risk:
-
Quit smoking: Smoking is a major risk factor for pancreatic cancer.
-
Maintain a healthy weight: Avoiding obesity can reduce the risk of cancer.
-
Limit alcohol consumption: Excessive alcohol intake is associated with an increased risk of pancreatic cancer.
-
Eat a balanced diet: A diet rich in fruits, vegetables, and whole grains can promote overall health and potentially reduce cancer risk.
-
Exercise regularly: Physical activity can help maintain a healthy weight and improve overall well-being.
10. Are there any clinical trials or new treatments for Pancreatic Cancer? Yes, there are ongoing clinical trials testing new treatments for pancreatic cancer. These include experimental drugs, immunotherapies, and targeted therapies that aim to improve survival rates and reduce side effects. Patients may have the option to participate in clinical trials if standard treatments are not effective or if they are seeking new treatment options. It’s important for patients to discuss the possibility of participating in clinical trials with their oncologist to understand the potential risks and benefits.
The other Oncology Procedures are
Few Major Hospitals for Treatment of Pancreatic Cancer are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



