Small intestine cancer, also known as small bowel cancer, is a rare but serious form of cancer that develops in the tissues of the small intestine—the long, narrow part of the digestive tract that lies between the stomach and the large intestine. Although the small intestine plays a crucial role in digestion and nutrient absorption and comprises a significant portion of the gastrointestinal tract, cancers in this region are relatively uncommon, accounting for less than 3% of all gastrointestinal cancers. This type of cancer can originate in any of the three parts of the small intestine: the duodenum, jejunum, or ileum, with the duodenum being the most commonly affected site.
There are several histological types of small intestine cancer, including adenocarcinoma, neuroendocrine tumors (carcinoid tumors), lymphomas, and gastrointestinal stromal tumors (GISTs). Each type varies in behavior, symptoms, and treatment approach. The rarity and anatomical complexity of the small intestine often make early diagnosis challenging, as the symptoms may be vague or mistaken for more common gastrointestinal conditions.
However, with advancements in diagnostic tools, surgical techniques, and targeted therapies, outcomes for patients with small intestine cancer have significantly improved. Raising awareness about this rare condition is essential for promoting early detection and timely medical intervention.
The precise cause of small intestine cancer is not always clear, but researchers have identified several risk factors that increase the likelihood of developing the disease:
Genetic and Hereditary Factors
-
Familial Adenomatous Polyposis (FAP): A hereditary condition where numerous polyps develop in the gastrointestinal tract, some of which may become cancerous.
-
Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer - HNPCC): An inherited condition that raises the risk of various gastrointestinal cancers, including those of the small intestine.
-
Peutz-Jeghers Syndrome: Characterized by benign polyps in the intestines and pigmented spots on the skin, increasing the risk of small bowel malignancies.
Chronic Inflammatory Conditions
-
Crohn’s Disease: Long-term inflammation of the gastrointestinal tract can cause cellular damage, potentially leading to cancer, especially adenocarcinoma.
-
Celiac Disease: Chronic inflammation due to gluten intolerance can increase the risk of intestinal lymphoma.
Dietary and Lifestyle Risk Factors
-
High intake of red or processed meats
-
Low-fiber diet
-
Smoking and excessive alcohol consumption
-
Exposure to environmental carcinogens (e.g., herbicides or industrial chemicals)
Other Risk Factors
-
Previous gastrointestinal surgeries
-
Long-standing ulcers or chronic infections
-
Immune system suppression, such as in organ transplant patients
Understanding these risk factors can lead to better surveillance, early detection, and even prevention in individuals at high risk.
The symptoms of small intestine cancer are often nonspecific and may resemble more benign gastrointestinal issues, which complicates early detection. However, persistent or worsening signs should prompt further investigation.
Common Symptoms Include:
-
Abdominal pain or cramping: Often intermittent and located in the middle or upper abdomen.
-
Nausea and vomiting: Especially if there is a partial blockage in the intestine.
-
Unexplained weight loss
-
Change in bowel habits: Diarrhea or constipation, depending on tumor location.
-
Blood in stool: May appear as red blood or black, tarry stools (melena).
-
Fatigue and weakness: Frequently caused by anemia due to internal bleeding.
-
Jaundice: Yellowing of the skin and eyes if the tumor affects bile ducts.
-
Bloating and gas
-
Early satiety: Feeling full after eating small amounts of food.
Because these symptoms can be easily misinterpreted as signs of ulcers, irritable bowel syndrome (IBS), or gastritis, many patients are diagnosed only after the disease has progressed.
Diagnosing small intestine cancer typically involves a combination of clinical evaluation, imaging studies, endoscopic procedures, and biopsy confirmation.
Step-by-Step Diagnostic Process:
A. Medical History and Physical Examination
A detailed history of symptoms, family history of cancer, and physical examination can guide further tests.
B. Laboratory Investigations
-
Complete Blood Count (CBC): May reveal anemia.
-
Liver Function Tests (LFTs): Elevated bilirubin in case of bile duct involvement.
-
Tumor Markers: Chromogranin A for NETs, or CEA for adenocarcinomas.
C. Imaging Studies
-
CT Scan or MRI: To detect mass lesions, lymph node involvement, or metastases.
-
Barium X-ray or small bowel follow-through: Highlights structural abnormalities.
-
PET-CT: Used to identify metastases or recurrence after treatment.
D. Endoscopy and Enteroscopy
-
Capsule Endoscopy: A swallowable camera records images as it travels through the GI tract.
-
Double Balloon Enteroscopy: Allows direct visualization and biopsy of the small bowel.
E. Biopsy
Histological confirmation of cancer is essential to determine the tumor type and guide treatment.
F. Staging
Staging is based on the TNM system (Tumor size, Node involvement, Metastasis), which determines prognosis and treatment strategy.
Treatment for small intestine cancer depends on the type, size, location, stage, and patient’s overall health. A multidisciplinary approach involving oncologists, gastroenterologists, and surgeons is essential for optimal outcomes.
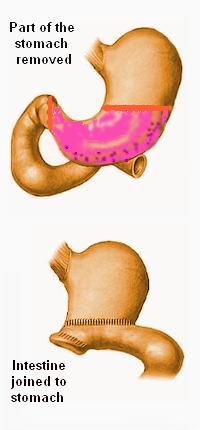
1. Surgical Treatment
-
Segmental Resection: Removal of the affected portion of the small intestine.
-
Whipple Procedure: Used for duodenal tumors, this major operation removes part of the pancreas, small intestine, and bile duct.
-
Lymphadenectomy: Removal of regional lymph nodes for accurate staging and better prognosis.
Surgery is the mainstay of treatment for localized tumors.
2. Chemotherapy
Chemotherapy is especially effective for:
-
Adenocarcinomas: Treated with regimens such as FOLFOX (5-FU, leucovorin, oxaliplatin).
-
Lymphomas: Treated with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone).
-
Often used post-surgery or in metastatic disease.
3. Radiation Therapy
-
Used in select cases to shrink tumors or relieve symptoms.
-
More common in lymphomas or NETs but rarely the primary treatment in adenocarcinomas.
4. Targeted Therapy
-
For GIST tumors, imatinib and sunitinib are effective.
-
Targets specific mutations in cancer cells without harming normal cells.
5. Immunotherapy
-
Particularly useful for tumors with MSI-H or dMMR markers.
-
Drugs such as pembrolizumab have shown promising results.
6. Palliative Care
In advanced stages, treatment may focus on pain relief, symptom control, and improving quality of life.
Prevention Strategies
While it’s not always possible to prevent small intestine cancer, especially in people with hereditary syndromes, certain measures may reduce risk:
-
Healthy Diet: High in fruits, vegetables, and fiber; low in processed meats.
-
Avoid Smoking and Alcohol: Both are linked to several gastrointestinal cancers.
-
Regular Screening: Especially in high-risk individuals with familial syndromes.
-
Managing Chronic Diseases: Treating Crohn’s disease and celiac disease proactively.
-
Genetic Testing and Counseling: Recommended for individuals with family history of gastrointestinal cancers.
Management Post-Treatment
-
Routine Follow-Up: Surveillance with imaging and blood tests every 3-6 months.
-
Nutritional Support: Managing malabsorption or nutrient deficiencies.
-
Psychosocial Support: Counseling and patient education to cope with emotional stress.
Complications can arise due to the cancer itself or from the treatment:
Tumor-Related Complications:
-
Intestinal Obstruction: Tumor blocks passage of food or waste.
-
Perforation: Weakening of the intestinal wall can cause leakage and infection.
-
Bleeding: Leads to anemia or life-threatening hemorrhage.
-
Metastasis: Commonly to the liver, lungs, or peritoneum.
Treatment-Related Complications:
-
Surgical risks: Infection, adhesions, leakage, and prolonged recovery.
-
Chemotherapy effects: Fatigue, nausea, neuropathy, bone marrow suppression.
-
Radiation effects: Diarrhea, radiation enteritis, infertility (in some cases).
-
Malnutrition and weight loss due to altered absorption.
Early identification and intervention can reduce the impact of these complications and improve patient outcomes.
A diagnosis of small intestine cancer brings emotional, physical, and practical challenges. With modern treatment options, many patients live longer and with a good quality of life.
Physical Wellbeing
-
Maintain a balanced diet rich in nutrients.
-
Follow a tailored exercise program.
-
Adhere to medication and follow-up schedules.
Emotional and Mental Health
-
Seek support from mental health professionals or support groups.
-
Stay connected with family and friends.
-
Participate in patient advocacy or awareness groups to stay empowered.
Rehabilitation and Survivorship
-
Work with a nutritionist or physical therapist post-surgery.
-
Keep a cancer survivorship plan with your care team.
-
Use telemedicine for easier follow-up and monitoring.
1. What is Small Intestine Cancer?
Small intestine cancer is a rare form of cancer that originates in the tissues of the small intestine, a long, coiled organ that connects the stomach to the large intestine. It plays a key role in digesting food and absorbing nutrients. This cancer can occur in various forms, such as adenocarcinoma, carcinoid tumors (neuroendocrine tumors), lymphomas, and sarcomas, each arising from different types of cells in the intestinal wall. Though less common than colon or rectal cancers, small intestine cancer can be aggressive and requires prompt medical attention once diagnosed.
2. What are the most common types of small intestine cancer?
There are four primary types of small intestine cancer, each with unique characteristics. Adenocarcinoma is the most common type and typically begins in the lining of the small intestine, particularly the duodenum. Neuroendocrine tumors, also known as carcinoid tumors, develop from hormone-producing cells and tend to grow slowly, often in the ileum. Lymphomas start in immune cells and can occur in individuals with weakened immune systems or chronic inflammation like Crohn’s disease. Sarcomas, including gastrointestinal stromal tumors (GISTs), arise from the muscle or connective tissue of the intestine. Identifying the exact type is crucial for determining the most effective treatment.
3. What causes small intestine cancer?
The exact cause of small intestine cancer is not fully understood, but several risk factors have been identified. These include genetic conditions such as Lynch syndrome and familial adenomatous polyposis (FAP), which increase the risk of gastrointestinal cancers. Chronic inflammatory diseases of the intestines, such as Crohn's disease and celiac disease, are also linked to higher incidence. Lifestyle factors like smoking, excessive alcohol consumption, and a diet high in red or processed meats may contribute to cancer development. Additionally, individuals who have had colon cancer or other gastrointestinal malignancies are at an increased risk.
4. What are the symptoms of small intestine cancer?
Symptoms of small intestine cancer are often vague and non-specific, which can lead to delays in diagnosis. Common signs include persistent abdominal pain, cramping, or discomfort, especially after eating. Unexplained weight loss, fatigue, and weakness may occur due to nutrient malabsorption or chronic blood loss. Nausea, vomiting, and bloating are also frequently reported, especially if a tumor causes intestinal obstruction. Some patients may notice blood in their stool or have dark, tarry stools (melena), which can indicate gastrointestinal bleeding. Because these symptoms overlap with other less serious conditions, medical evaluation is essential.
5. How is small intestine cancer diagnosed?
Diagnosing small intestine cancer involves a combination of imaging tests, endoscopic procedures, and laboratory analyses. Physicians typically start with a CT scan or MRI to visualize the abdomen and detect tumors or blockages. Capsule endoscopy, where a patient swallows a small camera to take pictures throughout the small intestine, is a valuable tool for visualizing difficult-to-reach areas. A biopsy, either during endoscopy or surgery, is required to confirm the cancer type. Additional tests, such as PET scans or blood tests for tumor markers, may be performed to determine the extent of spread and plan appropriate treatment.
6. What are the treatment options for small intestine cancer?
Treatment for small intestine cancer depends on the cancer type, location, stage, and the patient’s overall health. Surgery is usually the first line of treatment and is aimed at removing the tumor along with a margin of healthy tissue. In cases where surgery is not possible or if the cancer has spread, chemotherapy may be used to shrink the tumor or control its growth. Radiation therapy is sometimes used, particularly in lymphoma cases. Newer treatments, such as targeted therapy and immunotherapy, are increasingly being used for specific tumor types like GISTs or neuroendocrine tumors, especially when traditional therapies are not effective.
7. Is small intestine cancer curable?
Yes, small intestine cancer can be curable, especially when detected at an early stage and treated appropriately. Surgical removal of the tumor offers the best chance of a cure in localized cancers. However, the prognosis depends significantly on the cancer type and stage at diagnosis. Neuroendocrine tumors often have a more favorable outlook due to their slower growth rate, while advanced adenocarcinomas or lymphomas may require more aggressive treatment and have variable outcomes. With modern treatment strategies, including personalized therapies and close follow-up care, many patients can achieve long-term remission and improved quality of life.
8. What is the survival rate for small intestine cancer?
Survival rates for small intestine cancer vary widely depending on the type of tumor, its stage at diagnosis, and treatment effectiveness. For adenocarcinomas, the overall 5-year survival rate is approximately 30% to 40%, but this increases significantly if caught early. Neuroendocrine tumors have a better prognosis, with 5-year survival rates ranging from 60% to over 90%, depending on whether the tumor has spread. Lymphomas of the small intestine also have a relatively good survival rate, especially with responsive chemotherapy regimens. It is important to remember that these statistics are general estimates and individual outcomes may vary.
9. Can small intestine cancer be prevented?
While it is not always possible to prevent small intestine cancer, certain measures can reduce the risk. Maintaining a healthy lifestyle by eating a balanced diet rich in fruits, vegetables, and whole grains while limiting red and processed meats can be protective. Avoiding tobacco use and limiting alcohol consumption are also advisable. Managing chronic conditions like Crohn’s disease with medical supervision can lower cancer risk in affected individuals. For those with a family history of gastrointestinal cancers or inherited syndromes, genetic counseling and regular screening can help detect abnormalities at an earlier, more treatable stage.
10. What follow-up care is needed after treatment?
After completing treatment for small intestine cancer, regular follow-up care is essential to monitor for recurrence and manage any long-term side effects. Follow-up visits typically include physical examinations, imaging studies (such as CT scans), blood tests, and sometimes endoscopy, depending on the cancer type and initial treatment. Nutritional support may be necessary if a significant portion of the intestine was removed, affecting digestion or absorption. Patients are also encouraged to adopt healthy lifestyle habits to support recovery and reduce the risk of recurrence. A multidisciplinary team including oncologists, gastroenterologists, surgeons, and dietitians is often involved in ongoing care.
The other Oncology Procedures are
Few Major Hospitals for treatment of Small Intestine Cancer are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.