Stereotactic Radiosurgery (SRS) using the X-Knife system represents a groundbreaking advancement in non-invasive neurosurgical care. The term “radiosurgery” might be misleading, as it involves no scalpel or incisions. Instead, SRS utilizes precisely focused, high-energy beams of ionizing radiation to target tumors and lesions within the brain and spine with surgical accuracy—hence the term "X-Knife" (referring to the 'knife-like' precision of X-rays).
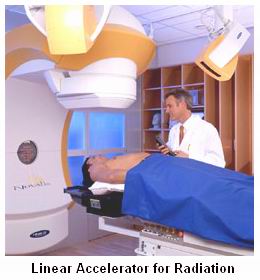
Developed in the late 1980s, X-Knife is based on a linear accelerator (LINAC) platform that uses sophisticated imaging guidance and immobilization technology to deliver intense radiation doses to well-defined targets while sparing adjacent normal tissues. It is particularly useful for treating tumors located in eloquent or surgically inaccessible regions of the central nervous system (CNS).
Unlike conventional radiotherapy, which involves multiple low-dose sessions over weeks, SRS delivers a single or a few high-dose treatments. This approach not only improves tumor control rates but also reduces treatment time and enhances patient comfort. It is an essential tool in the treatment of brain metastases, benign brain tumors, vascular malformations, and functional neurological disorders.
SRS using the X-Knife system is not a disease but a treatment strategy employed for various medical conditions, especially those involving the brain and spine. Understanding the underlying conditions that warrant this advanced therapy provides insight into its significance.
Common Conditions Treated with SRS (X-Knife)
1. Brain Metastases
-
Origin from primary cancers like lung, breast, kidney, colorectal, and melanoma.
-
Metastatic lesions are often multiple and located in critical areas of the brain.
2. Benign Brain Tumors
-
Vestibular Schwannomas (Acoustic Neuromas): Originating from the vestibular nerve, causing hearing loss and imbalance.
-
Meningiomas: Slow-growing tumors from the meninges, often found in the skull base.
-
Pituitary Adenomas: Hormone-secreting or compressive tumors within the sella turcica.
3. Arteriovenous Malformations (AVMs)
-
Congenital tangle of abnormal blood vessels that risk hemorrhage.
-
SRS causes gradual vessel occlusion without surgical risks.
4. Functional Disorders
-
Trigeminal Neuralgia: Debilitating facial pain often resistant to medication.
-
SRS targets the trigeminal nerve root to relieve pain.
5. Spinal Tumors
-
Both primary and metastatic spinal tumors can be treated.
-
Ideal for patients with tumors adjacent to the spinal cord where surgery poses high risk.
Risk Factors Leading to SRS Treatment
-
Inoperable or surgically risky tumor location.
-
Multiple brain lesions.
-
Recurrence after surgery or prior radiotherapy.
-
Advanced age or comorbid conditions.
-
Patient preference for non-invasive treatment.
The clinical presentation depends on the underlying disease process. Below are some key symptoms that may prompt SRS intervention:
Brain Metastases
-
Persistent or worsening headaches.
-
Seizures, especially new-onset in adults.
-
Cognitive decline, personality changes.
-
Focal neurological deficits (e.g., weakness, visual changes).
-
Nausea and vomiting due to raised intracranial pressure.
Benign Brain Tumors
-
Acoustic neuroma: Hearing loss, tinnitus, imbalance.
-
Pituitary adenomas: Hormonal disturbances (e.g., Cushing’s disease, acromegaly), vision loss due to optic chiasm compression.
-
Meningiomas: Symptoms based on location—seizures, vision issues, or motor impairment.
Arteriovenous Malformations
-
Sudden hemorrhagic stroke.
-
Seizures or persistent headaches.
-
Focal deficits from mass effect or microbleeds.
Trigeminal Neuralgia
-
Sudden, sharp, stabbing facial pain.
-
Triggered by talking, eating, or touch.
-
Refractory to medications in many patients.
Spinal Tumors
-
Localized back or neck pain.
-
Radicular pain radiating down the arms or legs.
-
Motor weakness, numbness, or paralysis.
-
Bowel or bladder dysfunction in severe cases.
Accurate diagnosis and target localization are essential for successful SRS planning. A combination of clinical, imaging, and sometimes histopathological evaluations is used.
Imaging Techniques
-
MRI (Magnetic Resonance Imaging): Gold standard for brain and spine evaluation.
-
CT Scan: Assists with bony anatomy and radiation planning.
-
MR Angiography or Digital Subtraction Angiography (DSA): Crucial for AVM diagnosis and mapping.
-
PET Scan: Helps in metabolic characterization, especially for metastatic lesions.
Functional Assessments
-
Neuropsychological testing for cognitive baselines.
-
Hormonal profile for pituitary lesions.
-
Visual field tests if optic pathway is involved.
Biopsy (if needed)
-
Often not required for radiologically classic benign tumors.
-
May be necessary for atypical or aggressive lesions.
SRS using the X-Knife system offers several therapeutic advantages:
1. Planning and Targeting
-
Utilizes frameless or frame-based stereotactic guidance.
-
Multiple high-energy beams converge on the target while sparing surrounding tissue.
2. Dose Delivery
-
Usually completed in one to five sessions.
-
Fractionated SRS may be used for larger or sensitive tumors.
3. Treatment Execution
-
Performed on an outpatient basis.
-
No incisions or anesthesia required.
-
Minimal to no recovery time compared to open surgery.
4. Post-Treatment Care
-
Follow-up MRI at 3–6 months.
-
Neurological monitoring.
-
Adjunctive medications if swelling or edema occurs.
While SRS is not a preventive treatment itself, long-term management and lifestyle adaptations can prevent complications or recurrences:
1. Monitoring Tumor Growth
-
Regular imaging is key for early detection of recurrence.
-
Tumors like meningiomas may need repeated imaging for years.
2. Symptom Management
-
Anti-inflammatory drugs to manage radiation-induced edema.
-
Anticonvulsants for seizure control.
-
Pain medications for trigeminal neuralgia or post-treatment discomfort.
3. Healthy Lifestyle
-
Avoid smoking and alcohol (especially in patients with brain tumors or AVMs).
-
Balanced diet and regular physical activity to support healing.
Though SRS is generally safe, some complications may arise:
Short-Term Side Effects
-
Fatigue
-
Nausea or headache
-
Mild skin irritation at the treatment site
Long-Term or Rare Complications
-
Radiation necrosis (dead tissue due to over-radiation)
-
Brain or spinal edema (swelling)
-
Temporary or permanent neurological deficits
-
Hearing loss (especially with vestibular schwannomas)
-
Hormonal dysfunction (if pituitary region treated)
Early intervention can minimize these risks. Use of advanced planning software helps reduce adverse outcomes.
For most patients, life after SRS is significantly improved:
1. Quality of Life
-
Minimal disruption to daily routine
-
Relief from tumor- or nerve-related symptoms
-
Rapid return to work or normal activities
2. Emotional Well-Being
-
Non-invasive nature reduces psychological stress compared to open surgery
-
Support from family, counseling, and patient groups helps recovery
3. Long-Term Follow-Up
-
Ongoing imaging and neurologist or oncologist visits
-
In some cases, repeat treatment may be necessary
4. Support Systems
Patients benefit from:
-
Rehabilitation therapy (if neurological symptoms persist)
-
Pain management clinics
-
Online and offline support groups
1. What is SRS (X-Knife)?
Stereotactic Radiosurgery (SRS) using the X-Knife system is a non-invasive radiation therapy technique designed to precisely target and destroy tumors or other abnormalities in the brain and spine without the need for traditional surgery. Despite the name, it does not involve any incisions. The X-Knife combines a linear accelerator (LINAC) with stereotactic imaging guidance to deliver high-dose, focused radiation beams to a specific area. It is used primarily to treat brain tumors, arteriovenous malformations (AVMs), and functional disorders like trigeminal neuralgia with sub-millimeter accuracy.
2. How does the X-Knife differ from Gamma Knife or CyberKnife?
While all three systems are designed for precise radiosurgery, they use different technologies. The X-Knife uses a LINAC (linear accelerator) and is ideal for both brain and spine treatments. Gamma Knife uses multiple cobalt-60 radioactive sources and is generally used only for brain conditions. CyberKnife, on the other hand, employs a robotic arm with a LINAC and is fully frameless, allowing for real-time tracking and adjustment. The X-Knife is particularly valued in hospitals that already use LINAC machines, making it a flexible and cost-effective alternative.
3. What conditions are treated using SRS with the X-Knife system?
SRS with the X-Knife is primarily used to treat brain tumors (both benign and malignant), metastatic brain lesions, acoustic neuromas, pituitary adenomas, meningiomas, and glioblastomas. It is also used for vascular abnormalities such as arteriovenous malformations (AVMs), as well as functional brain disorders like trigeminal neuralgia and certain forms of epilepsy. In some cases, X-Knife is employed for spinal tumors and recurrent cancers where conventional surgery or radiation has failed.
4. Is SRS (X-Knife) painful or invasive?
No, SRS with the X-Knife is non-invasive and painless. The procedure does not involve any surgical cuts or anesthesia. In most cases, a stereotactic head frame or custom-fitted mask is used to keep the patient immobile during the procedure, which may cause minor discomfort but not pain. Patients remain awake throughout the treatment and can typically return home the same day, making it a convenient option compared to traditional surgery.
5. How does the X-Knife system ensure accuracy in targeting tumors?
The X-Knife system achieves remarkable precision through a combination of stereotactic imaging, 3D treatment planning, and rigid patient immobilization. Before treatment, detailed imaging studies such as CT scans, MRI, or PET scans are used to map the exact size, shape, and location of the tumor. The radiation beams are then sculpted to match the contours of the target, minimizing exposure to surrounding healthy tissues. This accuracy allows clinicians to deliver high radiation doses in one or few sessions while reducing side effects.
6. How long does an X-Knife SRS procedure take?
The actual delivery of radiation typically takes between 30 minutes to 1 hour, depending on the complexity and size of the tumor. However, the entire visit—including patient setup, imaging verification, and post-procedure observation—may take 2 to 4 hours. Some patients may require a single high-dose session, while others might need fractionated SRS, which is delivered over multiple days. The treatment is performed on an outpatient basis, allowing most individuals to resume normal activities the same or next day.
7. What are the potential side effects of SRS with X-Knife?
Most patients tolerate X-Knife treatment well, with minimal side effects. Some common, usually temporary, side effects include headache, fatigue, nausea, or scalp irritation. Swelling around the treatment area may occur, which is sometimes managed with corticosteroids. In rare cases, depending on the treated area, patients may experience neurological changes, such as visual disturbances, weakness, or seizures. Long-term risks are minimal but may include radiation necrosis or late-onset changes in surrounding brain tissue, though these are uncommon with current techniques.
8. Is SRS (X-Knife) a cure for brain or spinal tumors?
SRS with the X-Knife is not always a definitive cure, but it can be highly effective in controlling tumor growth, reducing tumor size, and relieving symptoms. In cases of benign tumors or vascular malformations, it may completely eliminate the lesion over time. For malignant or metastatic tumors, SRS can significantly slow progression and improve survival and quality of life. It is also used for recurrent tumors when conventional options are limited. The effectiveness depends on the tumor type, size, and location.
9. Who is a candidate for SRS using the X-Knife system?
Ideal candidates include patients with well-defined tumors or lesions, typically less than 3–4 cm in diameter, and located in areas where surgical removal is risky or not possible. SRS is often considered for individuals who are not suitable for open surgery due to age, medical conditions, or tumor location. It may also be used as a supplemental treatment after surgery or as a salvage therapy for recurrent disease. A multidisciplinary evaluation is essential to determine if SRS is the appropriate option for a specific case.
10. What follow-up is required after X-Knife SRS treatment?
After treatment, patients will undergo routine follow-up imaging—usually MRI or CT scans—at regular intervals (every few months) to assess the tumor’s response to treatment. Clinical evaluations help monitor for any delayed side effects or tumor recurrence. In some cases, additional treatments may be recommended if the lesion does not fully resolve. Follow-up care is typically coordinated by a team of specialists, including radiation oncologists, neurosurgeons, and neurologists, to ensure comprehensive monitoring and long-term success.
The other Oncology Procedures are
Few Major Hospitals for treatment of SRS are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



