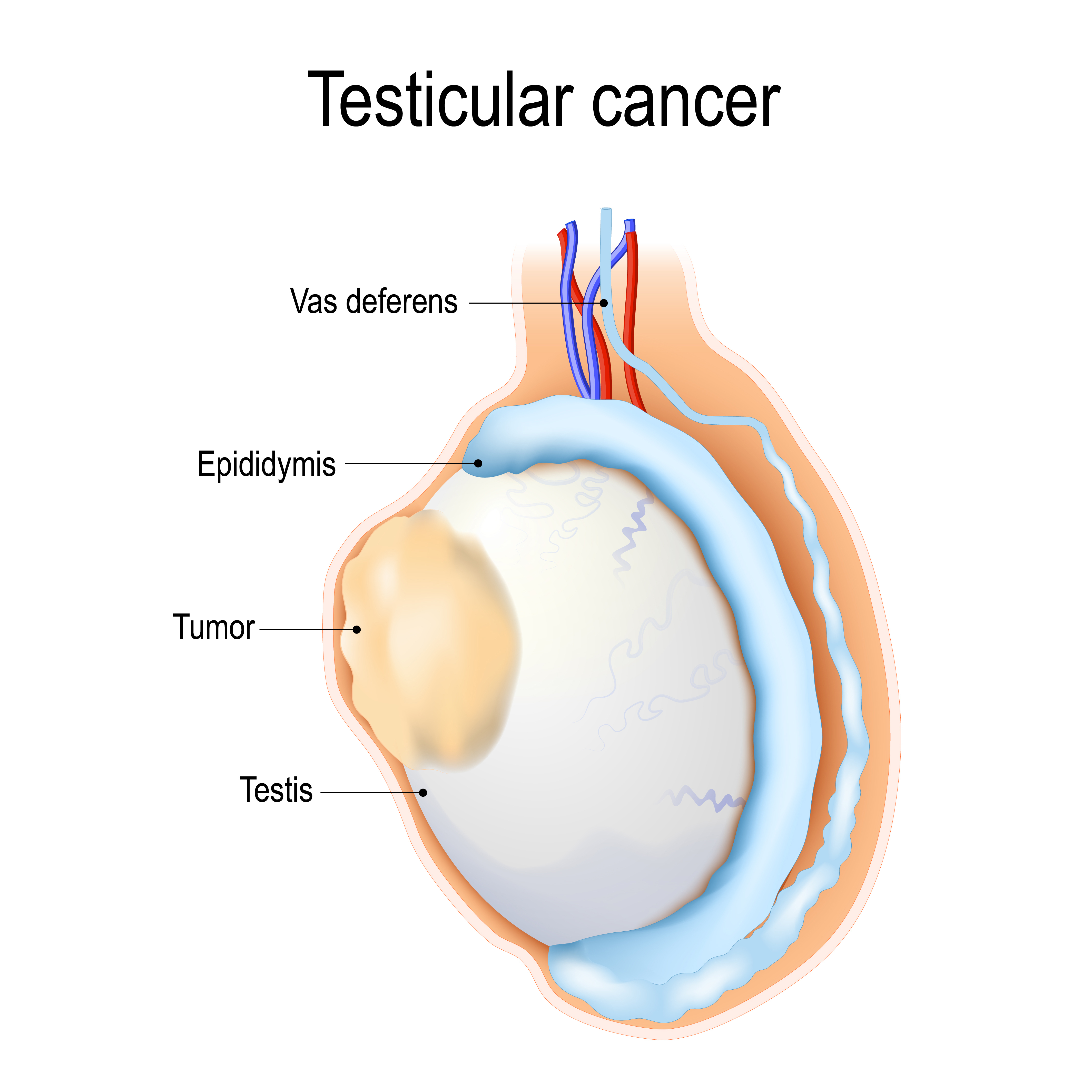
Testicular cancer is a rare form of cancer that originates in the male reproductive organs known as the testicles. The testicles are responsible for producing sperm and the hormone testosterone, which is essential for maintaining male reproductive health and secondary sexual characteristics. Though rare, testicular cancer is one of the most common cancers in men aged 15 to 35, with over 9,000 new cases reported annually in the United States alone.
Unlike many other cancers, testicular cancer is highly treatable, even when diagnosed at advanced stages. The survival rate for men diagnosed with testicular cancer is above 95%, making it one of the most successfully treatable cancers. The prognosis for men diagnosed early is even better, with survival rates nearing 99%.
Despite the positive outlook, testicular cancer remains a serious disease that requires early detection and appropriate treatment. Understanding its causes, symptoms, diagnosis, and treatment options is essential for men to recognize the signs of this disease and seek medical help promptly.
While the exact cause of testicular cancer is not fully understood, researchers have identified several risk factors that may increase the likelihood of developing the disease. These factors include genetic, environmental, and medical conditions that can predispose a man to testicular cancer.
-
Undescended Testicles (Cryptorchidism): One of the most significant risk factors for testicular cancer is a history of undescended testicles, a condition known as cryptorchidism. This occurs when one or both testicles fail to descend into the scrotum before birth. Even if the condition is surgically corrected, the risk of testicular cancer remains higher compared to men whose testicles descended normally.
-
Family History: Men who have a family history of testicular cancer are more likely to develop the disease. Having a father or brother who has had testicular cancer increases the risk, indicating a possible genetic predisposition.
-
Age: Testicular cancer predominantly affects young men, typically between the ages of 15 and 35. However, it can occur in men outside this age range, including older men. Still, the incidence is much lower among those over 50.
-
Race and Ethnicity: Testicular cancer is more common among Caucasian men than in men of African or Asian descent. Studies suggest that this racial disparity may be related to genetic factors, but the exact reasons are not yet clear.
-
Previous Testicular Cancer: Men who have previously had testicular cancer in one testicle are at a significantly higher risk of developing cancer in the other testicle. Although the risk is increased, most men with a history of testicular cancer go on to live cancer-free lives after treatment.
-
HIV/AIDS: Men with HIV or acquired immunodeficiency syndrome (AIDS) have a higher risk of testicular cancer, particularly when their immune systems are severely compromised. Research shows that the risk is elevated in men with HIV, especially if their immune systems are weakened due to the disease.
-
Environmental Factors: Exposure to certain environmental toxins, chemicals, and pesticides can increase the risk of testicular cancer. Occupations involving heavy exposure to such chemicals, as well as certain lifestyle factors, may also contribute to an increased risk.
-
Increased Estrogen Exposure: Men who have been exposed to high levels of estrogen in the womb (due to maternal hormonal treatments or other reasons) may be at greater risk of testicular cancer later in life.
Although these risk factors are associated with an increased risk of developing testicular cancer, many men with the disease do not have any identifiable risk factors. Additionally, some men with multiple risk factors may never develop cancer.
Testicular cancer is often referred to as a “silent” cancer, particularly in its early stages. This means that many men may not notice any symptoms until the disease has progressed. Regular self-exams are crucial for early detection. Common symptoms and signs of testicular cancer include:
-
A Lump or Swelling in the Testicle: The most noticeable and common symptom of testicular cancer is the presence of a lump or mass in the testicle. This lump is usually firm, and it may vary in size. Not all lumps are cancerous, as benign conditions like cysts or varicoceles can also cause swelling.
-
Pain or Discomfort in the Testicle: Some men experience pain or discomfort in the affected testicle. The pain can range from mild to severe and may be associated with swelling or tenderness. In some cases, the pain can also radiate to the groin or lower abdomen.
-
Heaviness in the Scrotum: A feeling of heaviness in the scrotum can also occur, particularly if the cancer has caused the testicle to enlarge.
-
Gynecomastia (Breast Tenderness or Swelling): Testicular cancer, particularly seminomas (a type of testicular cancer), can cause hormonal changes that lead to breast tenderness or swelling in men, a condition called gynecomastia.
-
Back Pain: As testicular cancer progresses, it may spread to lymph nodes in the abdomen, pelvis, or chest. When this happens, it can cause persistent lower back pain, which may worsen over time.
-
Abdominal or Groin Pain: Pain in the lower abdomen or groin can occur if the cancer has spread to lymph nodes or other areas near the testicles.
-
Fatigue and Unexplained Weight Loss: As with other cancers, testicular cancer may lead to general fatigue and unexplained weight loss, particularly in more advanced stages of the disease.
-
Changes in Testicle Size: The size of the testicles may change, either by enlarging or shrinking. In some cases, the enlargement is due to fluid accumulation (hydrocele), while in others, it is due to the presence of the tumor itself.
It’s important to remember that these symptoms can be caused by a variety of conditions other than cancer. However, if you notice any of these symptoms, it is important to consult a healthcare provider for further evaluation.
Diagnosing testicular cancer begins with a thorough medical history and physical examination. If testicular cancer is suspected, the following diagnostic procedures may be performed:
-
Physical Examination: The doctor will examine the scrotum, testicles, and surrounding areas for any lumps, swelling, or changes. They will also check for tenderness, signs of infection, or abnormalities in the lymph nodes.
-
Scrotal Ultrasound: A scrotal ultrasound is the most common imaging test used to evaluate a lump in the testicle. The ultrasound uses sound waves to create images of the testicles and surrounding tissues, helping doctors determine whether the mass is solid (which may indicate cancer) or fluid-filled (suggesting a benign condition such as a hydrocele).
-
Blood Tests: Blood tests are performed to check for elevated levels of tumor markers, which are substances produced by cancer cells. The most common tumor markers for testicular cancer include:
-
Alpha-fetoprotein (AFP)
-
Human chorionic gonadotropin (hCG)
-
Lactate dehydrogenase (LDH)
-
Elevated levels of these markers may suggest the presence of testicular cancer, though other conditions can also cause high levels.
-
CT Scan or MRI: If the cancer has spread, imaging tests such as a CT scan or MRI may be performed to assess the extent of the disease. These tests help doctors check the lymph nodes, chest, abdomen, and pelvis for signs of metastasis.
-
Biopsy: Biopsy is rarely performed for testicular cancer, as the disease is typically diagnosed through ultrasound and blood tests. However, in some cases, a biopsy may be done to confirm the diagnosis, especially if the lump appears to be benign or if additional tissue is needed for evaluation.
-
Lymph Node Biopsy: If cancer has spread to the lymph nodes, a biopsy may be performed to confirm metastasis and guide treatment.
Once the diagnosis is confirmed, doctors determine the stage of the cancer (the extent of its spread) to guide treatment options.
Testicular cancer treatment depends on the cancer’s type, stage, and location, as well as the patient’s overall health. The most common treatment options for testicular cancer include:
-
Surgery: The primary treatment for testicular cancer is the removal of the affected testicle (orchiectomy). This surgery is typically performed through an incision in the groin. Orchiectomy is a very effective method of removing the cancerous tumor, and it is often performed as the first line of treatment.
-
Chemotherapy: Chemotherapy is used to destroy cancer cells throughout the body and is often employed when the cancer has spread. It is most commonly used for non-seminomatous germ cell tumors (NSGCTs), which are more aggressive than seminomas. Chemotherapy drugs are typically administered through an intravenous (IV) drip, and multiple cycles may be required depending on the cancer’s stage.
-
Radiation Therapy: Radiation therapy is typically used for seminomas, a type of testicular cancer. It is usually directed at the lymph nodes in the abdomen, chest, or pelvis to kill any remaining cancer cells after surgery.
-
Surveillance: In some cases, particularly for early-stage testicular cancer, a watch-and-wait approach known as surveillance may be adopted. This involves monitoring the patient closely with regular follow-up visits, blood tests, and imaging tests to check for any signs of recurrence.
-
Stem Cell or Bone Marrow Transplant: In cases where the cancer has spread to other areas of the body and is resistant to chemotherapy, stem cell or bone marrow transplant may be considered. This treatment option is used in advanced cases of testicular cancer where other therapies have not been successful.
The treatment plan will vary depending on the type of testicular cancer, the stage of the disease, and the patient’s overall health. A combination of treatments may be used to achieve the best possible outcome.
While it’s impossible to completely prevent testicular cancer, there are steps that can help reduce the risk and manage the disease:
-
Self-Examination: Regular testicular self-exams are essential for detecting abnormalities early. Men should perform monthly self-exams to check for lumps, swelling, or changes in the size or shape of the testicles.
-
Early Detection: Early detection is key to successful treatment. Men who are at higher risk (such as those with a family history or a history of undescended testicles) should undergo regular check-ups and screenings with their healthcare provider.
-
Healthy Lifestyle: Eating a healthy diet, exercising regularly, and avoiding smoking and excessive alcohol consumption can help maintain overall health and reduce cancer risk.
-
Follow-Up Care: Regular follow-up care is essential after treatment for testicular cancer. This includes regular physical exams, blood tests, and imaging tests to monitor for recurrence.
While testicular cancer has a high cure rate, there are potential complications associated with the disease and its treatment:
-
Infertility: Testicular cancer treatments, especially chemotherapy and surgery, can affect fertility. Men who are concerned about fertility should discuss sperm banking options before starting treatment.
-
Hormonal Imbalance: Removing one testicle generally does not affect testosterone levels. However, if both testicles are removed, testosterone replacement therapy may be required.
-
Recurrence: There is always a risk of recurrence, particularly in more advanced cases or in patients who did not undergo aggressive treatment. Regular monitoring and follow-up care are crucial for early detection.
-
Emotional Impact: Cancer diagnosis and treatment can cause significant emotional distress. Support groups, therapy, and counseling can help patients and their families cope with the psychological impact of testicular cancer.
Life after testicular cancer treatment requires careful management and regular follow-ups:
-
Recovery and Rehabilitation: After surgery or chemotherapy, patients may need physical therapy to regain strength, especially if they experience long-term side effects from treatment.
-
Mental Health: Dealing with cancer and its treatment can take a toll on mental health. Counseling, support groups, and mental health professionals can help individuals cope with the emotional and psychological challenges.
-
Fertility Considerations: After treatment, men should discuss fertility options with their doctor. Sperm banking before treatment can provide an opportunity to have children in the future.
-
Regular Monitoring: Even after treatment, it’s important to have regular check-ups with an oncologist to monitor for recurrence and manage any ongoing health issues.
1. What is testicular cancer?
Testicular cancer is a type of cancer that develops in the testicles (the male reproductive glands that produce sperm and testosterone). It is relatively rare, but it is one of the most treatable types of cancer when detected early. Testicular cancer primarily affects younger men, usually between the ages of 15 and 35, but it can occur at any age.
2. What are the causes of testicular cancer?
The exact cause of testicular cancer is unknown, but certain risk factors can increase the likelihood of developing it, such as:
-
Undescended testicles (cryptorchidism): Men with this condition are at higher risk.
-
Family history: A family history of testicular cancer increases the risk.
-
Age: Most cases occur in men between the ages of 15 and 35.
-
Previous history of testicular cancer: Men who have had cancer in one testicle are at higher risk of developing it in the other testicle.
-
HIV infection: There is an increased risk among men with HIV.
3. What are the symptoms of testicular cancer?
Common symptoms of testicular cancer include:
-
A lump or swelling in one testicle.
-
Pain or discomfort in the testicle or scrotum.
-
A feeling of heaviness in the scrotum.
-
Pain or discomfort in the lower abdomen or groin area.
-
Unexplained back pain (in later stages, if cancer has spread).
-
Changes in the appearance or size of the testicle.
It is important to note that not all lumps or swelling are cancerous. A visit to the doctor is recommended for proper evaluation.
4. How is testicular cancer diagnosed?
Diagnosis of testicular cancer typically involves several steps:
-
Physical exam: The doctor will examine the testicles and scrotum to check for abnormalities.
-
Ultrasound: An ultrasound of the scrotum helps to assess the size and nature of the lump.
-
Blood tests: Tumor markers such as alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (hCG), and lactate dehydrogenase (LDH) may be elevated in testicular cancer.
-
CT scan or MRI: To check for any spread of cancer to nearby lymph nodes or other organs.
-
Biopsy: In rare cases, a biopsy may be done, though usually, the tumor is surgically removed for confirmation.
5. What are the different types of testicular cancer?
There are two main types of testicular cancer:
-
Germ cell tumors: These tumors arise from the cells that produce sperm. They account for about 95% of testicular cancer cases and are further classified into:
-
Seminomas: Slow-growing cancer that is typically diagnosed in men aged 25 to 45.
-
Non-seminomas: These tend to grow more quickly and affect younger men.
-
-
Stromal tumors: These are rare and arise from the tissue that supports the testicles, such as the cells that produce testosterone.
6. What is the treatment for testicular cancer?
The treatment for testicular cancer depends on the type, stage, and whether it has spread. Treatment options include:
-
Surgery (Orchiectomy): Removal of the affected testicle is typically the first step in treatment.
-
Chemotherapy: If the cancer has spread, chemotherapy may be used to kill cancer cells throughout the body.
-
Radiation therapy: Used primarily for seminomas that have spread to nearby lymph nodes.
-
Surveillance: For some cases, particularly if the cancer is localized and low-stage, careful monitoring may be recommended after surgery.
7. What is the survival rate for testicular cancer?
Testicular cancer has a high survival rate, especially when diagnosed early. The 5-year survival rate for localized testicular cancer is nearly 99%. Even for advanced stages, the survival rate remains high, with a 5-year survival rate of around 96%. The survival rate depends on factors such as the cancer stage, type, and overall health of the individual.
8. Can testicular cancer affect fertility?
Testicular cancer and its treatments, such as surgery, chemotherapy, and radiation, can affect fertility. Removal of one testicle typically does not affect fertility, as the remaining testicle can still produce sperm. However, chemotherapy and radiation can impact sperm production and reduce fertility. It is recommended that men consider sperm banking (cryopreservation) before starting treatment if they wish to have children in the future.
9. Can testicular cancer recur after treatment?
Yes, testicular cancer can recur, especially if it was diagnosed at an advanced stage. However, the recurrence rate is low, especially for localized cancers treated with surgery. Regular follow-up visits, including blood tests, ultrasounds, and scans, are crucial for monitoring and early detection of any recurrence.
10. How can I reduce my risk of testicular cancer?
While there is no guaranteed way to prevent testicular cancer, some steps may help reduce the risk:
-
Regular self-examination: Checking the testicles monthly for lumps or changes in size or shape can help detect cancer early.
-
Seek medical attention: If you notice any symptoms like lumps or discomfort, it is important to consult a doctor.
-
Manage underlying health conditions: Conditions like undescended testicles or HIV can increase the risk of testicular cancer, so managing these health issues with your doctor may help lower the risk.
-
Avoid exposure to toxins: Limiting exposure to environmental toxins and chemicals may also help reduce the risk.
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.