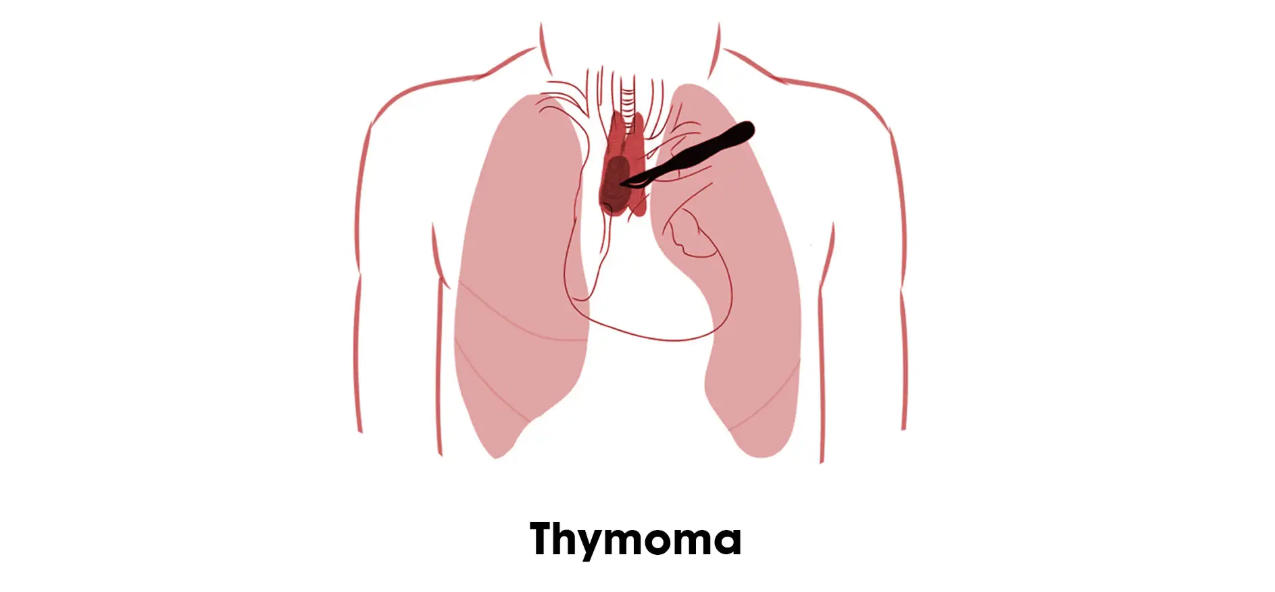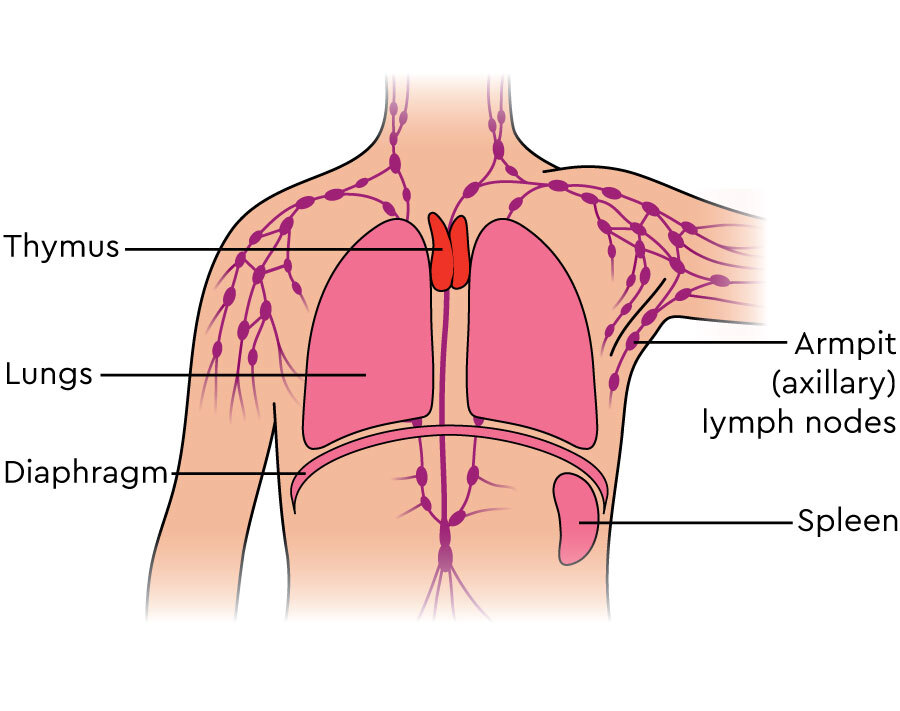
Thymoma and Thymic Carcinoma are two types of cancer that arise from the thymus, a small organ located in the chest, behind the sternum. The thymus plays a vital role in the immune system by producing and maturing T-cells, which are responsible for protecting the body from infections and abnormal cells. While the thymus is essential for normal immune function, cancer can develop within the thymus, causing the abnormal growth of cells.
Thymomas are typically slow-growing, well-contained tumors, whereas thymic carcinomas are rarer and more aggressive. The primary difference between these two types of tumors is their level of malignancy, with thymic carcinomas being more likely to spread to other areas of the body, leading to more complex treatment plans.
Thymomas often occur in middle-aged adults, particularly those between the ages of 40 and 60, but they can also affect younger and older individuals. Thymic carcinoma, on the other hand, is more likely to affect older individuals, though it can occur in a broader age range. Both types of tumors are relatively rare, and in some cases, they may go undetected for years due to their asymptomatic nature in early stages.
Thymoma and thymic carcinoma are often diagnosed during routine imaging or when the individual experiences symptoms related to autoimmune conditions. Though both cancers present treatment challenges, advancements in surgery, radiation, and chemotherapy have led to improved prognosis for many patients.
The exact causes of thymoma and thymic carcinoma remain unclear, but certain factors increase the likelihood of developing these cancers. Several risk factors have been identified through research, including genetic, environmental, and autoimmune-related factors:
-
Genetic Factors: While no specific gene mutation has been directly linked to thymoma or thymic carcinoma, certain genetic conditions increase susceptibility to these cancers. For example, individuals with Li-Fraumeni syndrome, a genetic disorder that predisposes individuals to various cancers, have a higher likelihood of developing thymic tumors. Similarly, individuals with Neurofibromatosis type 1 (NF1) may have an increased risk due to the association between NF1 and tumors of the thymus.
-
Autoimmune Diseases: The thymus gland is crucial for immune function, and its dysfunction is associated with several autoimmune diseases. Myasthenia Gravis, a neuromuscular disorder characterized by muscle weakness, is the most common autoimmune disease linked to thymoma. Other autoimmune conditions, such as lupus or rheumatoid arthritis, can also be associated with a higher incidence of thymoma and thymic carcinoma. The exact mechanism by which these autoimmune diseases contribute to thymic tumor development remains under investigation, but it is thought to involve immune system dysregulation.
-
Age: The incidence of thymoma and thymic carcinoma typically increases with age, especially after the age of 40. These cancers are more commonly diagnosed in middle-aged adults, though they can occur at any age. Thymic carcinoma, being a more aggressive form of cancer, is more likely to occur in individuals over the age of 60.
-
Gender: Thymoma tends to be more common in men than in women, whereas thymic carcinoma appears to affect both genders equally. This gender disparity in thymomas is likely due to a combination of genetic and environmental factors, including lifestyle choices like smoking and alcohol use.
-
Radiation Exposure: Individuals who have been exposed to high doses of radiation, particularly in the chest area, may have an increased risk of developing thymic carcinoma. People who have undergone radiation therapy for other cancers, such as breast cancer or lymphoma, are at higher risk for developing both thymoma and thymic carcinoma later in life.
-
Smoking and Alcohol Use: Smoking and excessive alcohol consumption are well-known risk factors for many cancers, including thymoma and thymic carcinoma. Smoking can damage the cells in the thymus gland and surrounding tissues, making them more susceptible to cancer. Similarly, heavy alcohol use can contribute to immune system dysfunction, which may increase the risk of developing these cancers, particularly in combination with radiation exposure.
-
Family History: A family history of thymoma or other types of cancer may increase the risk of developing these cancers, although familial cases of thymoma and thymic carcinoma are rare. Genetic predispositions linked to inherited cancer syndromes may contribute to an individual’s risk.
-
Environmental Factors: Exposure to certain industrial chemicals, such as asbestos and certain solvents, has been linked to an increased risk of cancers, including those of the thymus. Occupational exposure to these carcinogens increases the likelihood of developing thymoma or thymic carcinoma, although the evidence is still inconclusive.
Although these risk factors increase the likelihood of developing thymoma and thymic carcinoma, the majority of individuals with these risk factors will not develop the disease. Conversely, some people with no identifiable risk factors may still be diagnosed with these rare cancers.
The symptoms of thymoma and thymic carcinoma can be subtle, especially in the early stages when the tumors are small and localized. Thymomas tend to grow slowly, and many people experience few symptoms until the tumor has become quite large. Thymic carcinomas, being more aggressive, may present with symptoms earlier and can progress rapidly. Common symptoms and signs of these conditions include:
-
Chest Pain: As thymomas grow, they can press against nearby structures in the chest, causing discomfort or dull pain. This pain may become more noticeable with physical activity, breathing, or even coughing.
-
Persistent Cough: A chronic dry cough that persists for several weeks or worsens over time can be a sign of a thymic tumor, particularly if the tumor interferes with the respiratory system or causes obstruction in the airways.
-
Difficulty Breathing (Dyspnea): Difficulty breathing or shortness of breath can occur when the tumor obstructs the airways, especially if the tumor is large enough to block the passage of air or if it presses on surrounding structures like the lungs or major blood vessels.
-
Fatigue: Generalized fatigue or weakness is common in cancer patients and can occur in those with thymoma or thymic carcinoma. This can be a result of the cancer itself, as well as from treatments like chemotherapy or radiation therapy.
-
Weight Loss: Unexplained weight loss is a common symptom in many cancers, including thymoma and thymic carcinoma. This can occur due to the body's increased energy demands when fighting cancer and may also be exacerbated by difficulty swallowing or poor appetite.
-
Swelling in the Neck or Face: Thymomas, particularly those that grow larger, can cause swelling in the neck or face. This is due to pressure on the superior vena cava (the large vein that carries blood from the head and arms to the heart), leading to Superior Vena Cava Syndrome. This condition results in the swelling of the face, neck, and upper chest.
-
Hoarseness or Voice Changes: If the tumor involves the larynx (voice box), it may cause changes in voice quality, including hoarseness or a raspy voice. This is more common in thymic carcinoma than in thymoma due to its more aggressive nature.
-
Swallowing Difficulties (Dysphagia): As the tumor enlarges, it may cause difficulty swallowing, either by obstructing the esophagus or pressing on the muscles involved in the swallowing process. This symptom can also result from Myasthenia Gravis in patients with thymomas.
-
Nasal Regurgitation: A sensation that food or liquid is coming back up through the nose can occur if the tumor affects the area around the throat and pharynx.
-
Myasthenia Gravis Symptoms: In people with thymomas, symptoms of Myasthenia Gravis may appear or worsen, leading to muscle weakness, difficulty speaking, difficulty chewing or swallowing, and drooping eyelids.
If any of these symptoms persist, it is essential to seek medical attention. Early diagnosis of thymoma and thymic carcinoma can improve treatment outcomes and reduce complications.
Diagnosing thymoma and thymic carcinoma involves several tests and diagnostic procedures to determine the tumor’s size, location, and whether it has spread to other areas of the body. The process includes:
-
Physical Examination: A thorough physical examination by a healthcare provider can help identify signs of a thymic tumor, such as swelling in the neck, chest, or face. The doctor may also check for abnormal sounds or changes in the voice.
-
Imaging Tests:
-
Chest X-ray: A chest X-ray may reveal the presence of a mass or abnormal growth in the chest, prompting further investigation.
-
CT Scan (Computed Tomography): A CT scan is an essential imaging test for assessing the size, shape, and extent of the tumor. It helps doctors plan treatment and identify potential spread to lymph nodes or other organs.
-
MRI (Magnetic Resonance Imaging): MRI provides detailed images of soft tissues and can help evaluate tumor infiltration into surrounding structures.
-
PET Scan (Positron Emission Tomography): A PET scan is used to detect areas of cancer spread in the body, helping to identify distant metastases and guide treatment decisions.
-
-
Biopsy: A biopsy is a procedure where a small sample of tissue is removed from the tumor and examined under a microscope to confirm the diagnosis. This is the definitive method for diagnosing thymoma or thymic carcinoma and distinguishing between benign and malignant tumors.
-
Blood Tests: Blood tests may be performed to detect markers that suggest cancer, such as elevated levels of certain proteins. Additionally, tests to detect Myasthenia Gravis may be ordered if the patient has symptoms of the autoimmune disorder associated with thymoma.
-
HPV Testing: For patients with suspected HPV-related throat cancer (thymic carcinoma in the oropharynx), testing for the presence of the virus may be conducted.
Treatment options for thymoma and thymic carcinoma depend on the type of tumor, its size, location, and whether it has spread to other parts of the body. Common treatment options include:
-
Surgery: The primary treatment for both thymoma and thymic carcinoma is surgery. The goal is to remove the tumor along with surrounding tissues. Thymectomy (removal of the thymus) is the standard procedure for thymomas. In more advanced cases or with thymic carcinoma, more extensive surgery may be required, including the removal of nearby lymph nodes or structures.
-
Radiation Therapy: Radiation therapy uses high-energy rays to target cancer cells, usually after surgery to eliminate remaining cells. It can also be used as the primary treatment for tumors that are not surgically accessible or for tumors that have metastasized.
-
Chemotherapy: Chemotherapy uses drugs to kill or control cancer cells. It is typically used for thymic carcinoma, particularly in advanced stages, and is often combined with surgery and radiation for more aggressive cancers.
-
Targeted Therapy: Targeted therapies are drugs that attack specific molecules involved in the growth of cancer cells. These therapies are still being explored for thymoma and thymic carcinoma but show promise in treating more aggressive cancers that do not respond to conventional therapies.
-
Immunotherapy: Immunotherapy is a newer treatment that boosts the body’s immune system to fight cancer. It can be an option for patients with advanced thymic carcinoma who have not responded to other treatments.
-
Palliative Care: For patients with advanced thymic carcinoma or those who cannot undergo curative treatment, palliative care may be used to improve the quality of life. This includes pain management, nutritional support, and symptom relief.
While there are no specific methods to prevent thymoma and thymic carcinoma, certain strategies can help reduce risk and manage the condition:
-
Avoid Smoking: Smoking cessation is the most effective way to reduce the risk of thymoma and thymic carcinoma. Avoiding tobacco and smoking-related carcinogens is key to preventing these cancers.
-
Limit Alcohol: Reducing alcohol intake can lower the risk of these cancers, especially when combined with smoking cessation.
-
Regular Health Screenings: Regular check-ups and imaging tests are essential for people with a history of autoimmune diseases or those at higher risk for developing thymic tumors.
-
Management of Autoimmune Disorders: If you have autoimmune conditions like Myasthenia Gravis, work closely with your doctor to manage the disease and prevent complications associated with thymomas.
-
Infection: As with most cancers, there is a risk of infection during treatment, particularly after surgery or chemotherapy. The immune system may be weakened, leading to a higher susceptibility to infections.
-
Recurrence: Thymic carcinoma, in particular, is prone to recurrence after treatment. Ongoing monitoring is necessary to detect any signs of the cancer returning.
-
Respiratory Complications: Tumors in the thymus can affect the lungs and airway, leading to difficulty breathing, coughing, or pneumonia.
Living with thymoma or thymic carcinoma can be challenging, but many patients live normal lives after successful treatment. Regular follow-up visits, lifestyle changes, and emotional support are crucial components of long-term care:
-
Speech and Swallowing Therapy: Many patients who undergo surgery to remove part of the thymus or surrounding structures may experience difficulty speaking or swallowing. Rehabilitation and therapy can help restore these functions.
-
Psychosocial Support: Coping with a cancer diagnosis and its treatments can be emotionally difficult. Support groups, counseling, and mental health professionals can assist with adjusting to life after cancer.
-
Nutritional Support: Maintaining a balanced diet and managing weight loss during and after treatment is essential. Patients may need feeding tubes temporarily if swallowing becomes difficult.
-
Long-Term Monitoring: Regular follow-ups with imaging studies and physical exams are crucial for detecting recurrence and managing long-term side effects of treatment.
1. What is Thymoma and Thymic Carcinoma?
Thymoma and thymic carcinoma are types of cancer that develop in the thymus, a small organ located behind the breastbone, in the chest cavity. The thymus is responsible for producing T-cells, which are crucial for the immune system.
-
Thymoma is a less aggressive, slow-growing tumor that typically arises from the epithelial cells of the thymus.
-
Thymic carcinoma is a rarer, more aggressive form of thymus cancer that can spread to other parts of the body.
2. What are the symptoms of Thymoma and Thymic Carcinoma?
In the early stages, both thymoma and thymic carcinoma may not cause noticeable symptoms. However, common signs of these cancers include:
-
Chest pain or pressure
-
Persistent cough or coughing up blood
-
Difficulty breathing or shortness of breath
-
Fatigue or weakness
-
Swelling in the face or neck
-
Unexplained weight loss
Some patients may also experience symptoms related to autoimmune disorders, as thymomas can sometimes be associated with conditions like myasthenia gravis.
3. What causes Thymoma and Thymic Carcinoma?
The exact cause of thymoma and thymic carcinoma is not fully understood, but several risk factors have been identified, including:
-
Age: Most cases occur in adults aged 40-60 years.
-
Gender: Thymomas are more common in women, while thymic carcinoma tends to be more common in men.
-
Autoimmune diseases: Individuals with autoimmune diseases like myasthenia gravis or lupus are at an increased risk.
-
Genetics: A family history of thymoma or other cancers may increase the risk.
-
Radiation exposure: Previous radiation treatment in the chest area can increase the risk.
4. How are Thymoma and Thymic Carcinoma diagnosed?
Diagnosis involves several steps:
-
Physical exam: The doctor may check for signs of swelling or unusual masses in the chest.
-
Imaging tests: Chest X-rays, CT scans, and MRIs help visualize the thymus and detect tumors.
-
Biopsy: A biopsy is performed to obtain a tissue sample from the thymus for examination under a microscope to confirm cancer.
-
Blood tests: May help assess the presence of autoimmune disorders or markers associated with thymoma.
-
Endobronchial ultrasound (EBUS): This test helps obtain samples from nearby lymph nodes to check for cancer spread.
5. What are the treatment options for Thymoma and Thymic Carcinoma?
Treatment for thymoma and thymic carcinoma depends on the type, size, and stage of the cancer. Common treatment options include:
-
Surgery: The primary treatment for both thymoma and thymic carcinoma is surgery to remove the tumor (thymectomy). For early-stage thymoma, surgery may offer a good chance of a cure.
-
Radiation therapy: Used after surgery to target any remaining cancer cells, or as a primary treatment for inoperable tumors.
-
Chemotherapy: Typically used for thymic carcinoma or advanced thymoma that has spread. Drugs are used to kill cancer cells or shrink the tumor.
-
Targeted therapy or immunotherapy: May be used for advanced cases or those that are resistant to other treatments.
6. What is the prognosis for Thymoma and Thymic Carcinoma?
The prognosis for thymoma generally depends on the stage of the cancer at diagnosis.
Early-stage thymomas often have a good prognosis with surgery. The overall 5-year
survival rate for patients with thymoma is relatively high, especially for low-stage
cases.
Thymic carcinoma, being more aggressive, has a lower survival rate and is often harder
to treat. The prognosis is influenced by the stage at diagnosis, the extent of
metastasis, and the response to treatment.
7. Can Thymoma and Thymic Carcinoma be prevented?
Currently, there is no known way to prevent thymoma or thymic carcinoma. However, reducing risk factors like avoiding unnecessary radiation exposure and managing autoimmune diseases may help lower the likelihood of developing these cancers. Regular medical check-ups, especially for individuals with autoimmune conditions, can help detect these cancers early when they are most treatable.
8. What are the complications of Thymoma and Thymic Carcinoma?
Potential complications of thymoma and thymic carcinoma include:
-
Spread of cancer (metastasis): In advanced cases, the cancer can spread to other organs, such as the lungs, liver, or bones.
-
Autoimmune disorders: Thymomas can sometimes be associated with autoimmune conditions like myasthenia gravis, leading to difficulty in muscle control and breathing.
-
Recurrence: Even after treatment, these cancers may recur, requiring additional therapy and monitoring.
-
Treatment-related side effects: Chemotherapy, radiation, or surgery may lead to side effects like fatigue, nausea, or respiratory issues.
9. Is there any link between Thymoma and Myasthenia Gravis?
Yes, there is a well-established association between thymomas and myasthenia gravis (MG), an autoimmune disorder that affects the communication between nerves and muscles, leading to muscle weakness. Around 30-40% of people with thymoma also have MG. Treating the thymoma can sometimes improve symptoms of MG, and in some cases, removal of the thymus may alleviate the symptoms of myasthenia gravis.
10. What is the role of clinical trials in treating Thymoma and Thymic Carcinoma?
Clinical trials play an essential role in the ongoing research and treatment of thymoma and thymic carcinoma. New therapies, such as targeted treatments, immunotherapies, and combination approaches, are continually being tested to improve outcomes. Patients with thymoma or thymic carcinoma may be eligible for clinical trials, which offer access to cutting-edge treatments that are not yet widely available.
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.