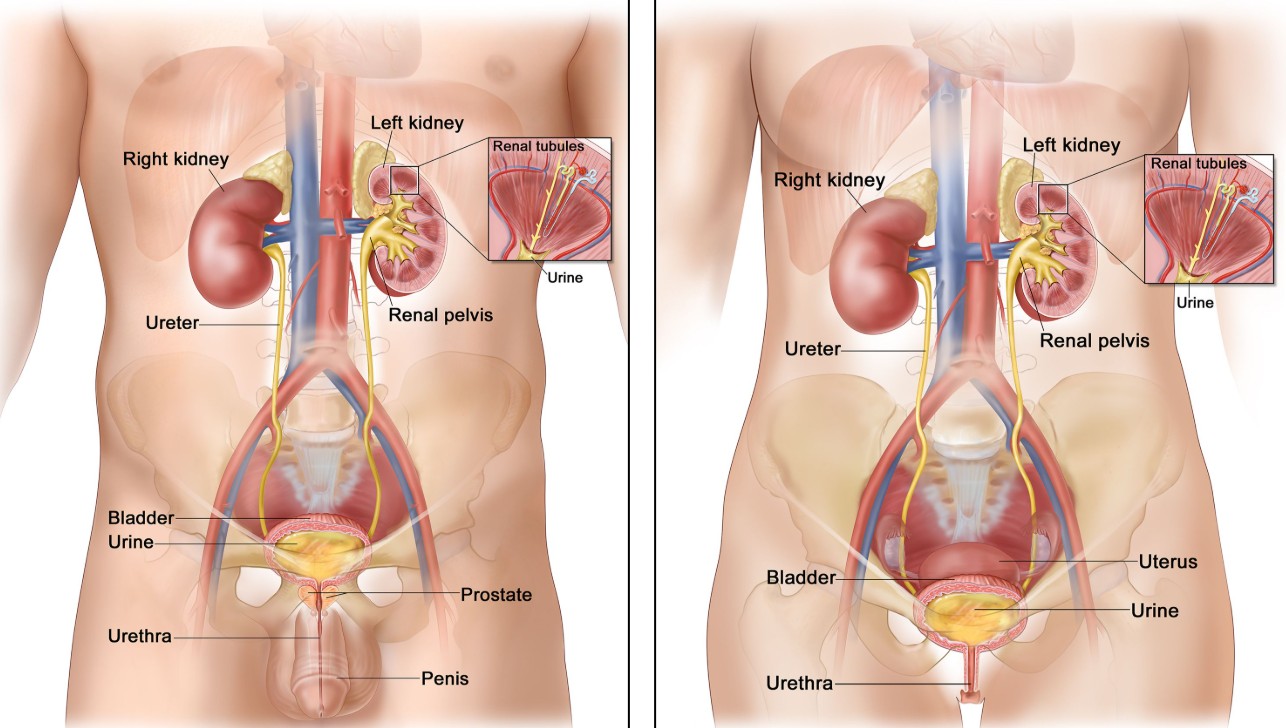
Transitional Cell Cancer (TCC), also referred to as urothelial carcinoma, is a type of cancer that arises from the transitional epithelium, the layer of cells that lines much of the urinary tract. While transitional cell cancer most commonly affects the bladder, it can also develop in the renal pelvis (the part of the kidney where urine collects before moving into the ureter) and ureters (the tubes that carry urine from the kidneys to the bladder).
Transitional cell cancer of the renal pelvis and ureter is rare, comprising about 5-10% of all urothelial cancers, but it is still an important condition to understand, especially since it shares similar risk factors and treatment strategies with bladder cancer. The cancer typically starts as a small tumor that may remain localized but can grow and spread to other parts of the urinary tract if left untreated. This form of cancer is challenging due to its symptoms often being mistaken for other, more common conditions, such as kidney stones or urinary tract infections.
Early detection and treatment are essential for improving the prognosis, as TCC in these areas can be aggressive and has the potential to metastasize to surrounding tissues and organs, such as the bladder, lungs, or lymph nodes. Fortunately, when detected early, the cancer is treatable through a combination of surgery, chemotherapy, and radiation therapy. This article will cover the causes, risk factors, symptoms, diagnosis, and treatment options for transitional cell cancer of the renal pelvis and ureter, as well as provide important information on how to manage and live with the condition.
Transitional cell cancer (TCC) of the renal pelvis and ureter develops when the cells lining these parts of the urinary tract begin to grow uncontrollably. The exact cause is not entirely clear, but several factors increase the risk of developing this type of cancer. Understanding these risk factors can help identify individuals who may be more susceptible to developing TCC.
-
Smoking: Smoking is the leading cause of transitional cell cancer in the urinary tract. The harmful chemicals found in tobacco smoke can enter the bloodstream and reach the kidneys, bladder, and ureters, causing genetic mutations in the cells lining the urinary tract. Smokers are two to three times more likely to develop TCC than non-smokers, and the risk increases with the amount and duration of smoking.
-
Chemical Exposure: Occupational exposure to certain chemicals, particularly those used in the manufacturing of dyes, rubber, textiles, and petroleum products, can significantly increase the risk of developing TCC. Chemicals such as aromatic amines, which are found in the workplace environment, are carcinogenic and have been shown to cause cancer in the urinary system. Individuals who work in industries like rubber manufacturing, printing, or oil refining are at an elevated risk.
-
Chronic Urinary Tract Infections: Long-standing urinary tract infections (UTIs), particularly when recurrent, can cause persistent irritation and inflammation of the urinary tract lining. Over time, this irritation can lead to cellular changes that increase the likelihood of developing TCC. Individuals who have had frequent kidney or bladder infections may have a higher risk of developing cancer in the renal pelvis or ureters.
-
Previous Cancer Treatment: People who have undergone radiation therapy for cancers such as lymphoma, prostate cancer, or cervical cancer, especially if they received radiation to the pelvic region, are at a higher risk of developing transitional cell cancer in the renal pelvis and ureters. The radiation exposure can damage healthy cells, leading to cancer development years later.
-
Age and Gender: The incidence of TCC in the renal pelvis and ureter increases with age. It is most commonly diagnosed in adults over the age of 50. Additionally, men are more likely to develop this cancer than women, which may be attributed to higher rates of smoking and exposure to industrial chemicals in men.
-
Genetic Factors: Family history plays a role in the development of transitional cell cancer. If a close family member, such as a parent or sibling, has had urothelial cancer, an individual’s risk of developing the disease is higher. Genetic mutations associated with inherited syndromes like Lynch syndrome (hereditary nonpolyposis colorectal cancer) may also predispose individuals to develop cancer in the urinary tract, including the renal pelvis and ureter.
-
Chronic Kidney Disease and Dialysis: Individuals with chronic kidney disease, particularly those undergoing long-term dialysis, are at an increased risk of developing TCC in the renal pelvis. Dialysis patients often have a history of repeated infections, kidney stones, and the introduction of foreign substances into the body, all of which can contribute to cancer development in the urinary tract.
-
Diet: While diet is not a direct cause of transitional cell cancer, certain dietary habits can increase risk. Diets that are high in fats, low in fiber, or lacking in antioxidants can contribute to the development of cancer. A healthy diet rich in fruits, vegetables, and whole grains may help lower the risk of cancer.
The symptoms of transitional cell cancer in the renal pelvis and ureter may be subtle in the early stages and often mimic those of other, more common conditions, making diagnosis challenging. As the tumor grows or spreads, more noticeable symptoms can develop. Common signs and symptoms include:
-
Hematuria (Blood in Urine): Hematuria, or blood in the urine, is the most common symptom of transitional cell cancer. This may be visible to the naked eye (gross hematuria) or detected only under a microscope (microscopic hematuria). The presence of blood in the urine is a red flag and should prompt further investigation.
-
Painful or Frequent Urination (Dysuria): Difficulty or pain while urinating can occur, particularly if the tumor is obstructing the ureter or bladder. This is often accompanied by a frequent need to urinate, which may be mistaken for a urinary tract infection.
-
Flank Pain or Lower Abdominal Pain: Pain or discomfort in the lower back or abdomen is common as the tumor presses against the kidney, ureter, or other nearby organs. The pain may be intermittent or constant, depending on the size and location of the tumor.
-
Fatigue: As with many types of cancer, individuals with transitional cell cancer may experience unexplained fatigue or weakness. This is often due to the body’s immune response to the tumor or the effects of cancer treatments.
-
Weight Loss: Unintentional weight loss without any known cause can be a sign of cancer. This is especially true if accompanied by loss of appetite or persistent nausea.
-
Swelling in the Abdomen or Legs: Swelling or edema can occur in advanced stages of the disease, particularly if the cancer has spread to lymph nodes or other areas. This swelling can be more noticeable in the abdomen or lower legs.
-
Nausea and Vomiting: As the cancer grows and obstructs the urinary tract, nausea and vomiting may occur, particularly if the kidney function is impaired.
-
Breathing Difficulty: If the cancer spreads to the lungs or affects the superior vena cava, it can lead to shortness of breath or difficulty breathing. This is a serious complication and requires immediate medical attention.
If any of these symptoms persist for more than a few days, it is important to seek medical attention for proper evaluation and diagnosis. Early detection significantly increases the chances of successful treatment.
To diagnose transitional cell cancer of the renal pelvis and ureter, several diagnostic procedures are used. These tests help doctors determine the type, size, and spread of the cancer:
-
Urinalysis: A urinalysis can detect the presence of blood or abnormal cells in the urine. It is often the first test performed if hematuria is reported.
-
Cystoscopy and Ureteroscopy: These procedures allow doctors to visually inspect the urinary tract, including the bladder and ureters, using a flexible tube with a camera (cystoscope or ureteroscope). During this procedure, tissue samples (biopsy) can be taken for further analysis.
-
Imaging Tests:
-
CT Scan (Computed Tomography): A CT scan is commonly used to assess the size and location of the tumor. It provides detailed images of the kidneys, renal pelvis, and ureters and helps determine if cancer has spread to surrounding tissues or organs.
-
MRI (Magnetic Resonance Imaging): MRI is used to obtain detailed images of soft tissues and is helpful for determining the tumor's extent, especially when dealing with complex cases.
-
Ultrasound: An ultrasound may be used as a non-invasive way to detect abnormal masses or tumors in the urinary tract. It helps doctors visualize kidney function and other structures.
-
Intravenous Pyelogram (IVP): An IVP involves injecting contrast dye into a vein to highlight the urinary system on X-rays. This test helps visualize abnormalities in the renal pelvis and ureters.
-
-
Biopsy: A biopsy involves removing a small sample of tissue from the tumor for examination under a microscope. This is the most definitive way to diagnose transitional cell cancer and determine whether it is benign or malignant.
-
Urine Cytology: Urine cytology involves examining a urine sample under a microscope to identify cancer cells. While it is not always conclusive, it can provide valuable information in suspicious cases.
Treatment for transitional cell cancer of the renal pelvis and ureter depends on the stage of the cancer, the location, and whether it has spread. The primary treatment options include:
-
Surgical Removal: The main treatment for localized TCC is surgery. The goal is to remove the tumor and surrounding tissues, which may include the affected kidney or parts of the ureter. In some cases, a nephrectomy (removal of the kidney) or partial nephrectomy may be required.
-
Chemotherapy: Chemotherapy uses powerful drugs to kill cancer cells. It is often used for advanced-stage TCC or if the cancer has spread to surrounding tissues. Chemotherapy can be administered before or after surgery and may be combined with radiation therapy.
-
Radiation Therapy: Radiation therapy is sometimes used in combination with surgery or chemotherapy. It is particularly useful for tumors that cannot be removed surgically or for cases of recurrence.
-
Immunotherapy: Immunotherapy boosts the body's immune system to recognize and destroy cancer cells. This is a newer treatment option for TCC, especially for cancers that are resistant to chemotherapy or radiation.
-
Targeted Therapy: Targeted therapy involves drugs that specifically target cancer cells by interfering with the molecules that promote cancer cell growth. This approach is used for more advanced or recurrent cases.
While it is not always possible to prevent transitional cell cancer, certain lifestyle changes can reduce the risk:
-
Quit Smoking: Smoking is the most significant preventable risk factor for transitional cell cancer. Quitting smoking can greatly reduce the risk of developing TCC and improve overall health.
-
Limit Alcohol Intake: Reducing or eliminating alcohol consumption may help lower the risk of TCC, especially when combined with smoking cessation.
-
Occupational Safety: For individuals working in industries with exposure to carcinogens (e.g., asbestos, chemical solvents), using proper protective equipment can help reduce the risk of developing urinary tract cancers.
-
Regular Screening: People at higher risk, such as those with a family history of urinary tract cancer or those with chronic kidney disease, should undergo regular checkups and imaging studies to detect any abnormalities early.
The treatment of transitional cell cancer can lead to several complications:
-
Infection: Surgery, chemotherapy, and radiation can weaken the immune system, making patients more susceptible to infections. Infections may arise after surgery or as a result of urinary tract obstruction.
-
Urinary Issues: Tumors affecting the renal pelvis or ureter may lead to issues such as obstruction, difficulty urinating, or frequent infections. Surgery to remove the tumor may lead to temporary or permanent changes in urinary function.
-
Recurrence: Transitional cell cancer is prone to recurrence, particularly if it was not fully removed or if it had spread to nearby tissues. Regular follow-up visits are crucial for monitoring for signs of recurrence.
Living with transitional cell cancer of the renal pelvis and ureter requires ongoing management and support. After treatment, patients will need regular follow-ups to monitor for recurrence and manage side effects of treatment. Common aspects of life after TCC include:
-
Physical Rehabilitation: After surgery or treatment, some patients may need rehabilitation to regain strength, especially if they have experienced complications or changes in urinary function.
-
Emotional Support: A cancer diagnosis can be emotionally taxing, and patients may benefit from counseling or support groups to cope with the psychological impact of the disease and its treatment.
-
Diet and Nutrition: Maintaining a balanced diet is essential, especially for patients who may have difficulty swallowing or eating due to surgery or treatment side effects. Nutritional support may be necessary for those who have lost weight or who are recovering from surgery.
-
Long-Term Follow-Up Care: Ongoing medical care, including imaging tests and physical exams, is essential for detecting any recurrence or new symptoms related to TCC.
1. What is transitional cell cancer of the renal pelvis and ureter?
Transitional cell cancer (TCC), also known as urothelial carcinoma, is a type of cancer that arises in the transitional cells lining the renal pelvis (the area where urine collects in the kidney) and the ureter (the tube that carries urine from the kidneys to the bladder). This form of cancer is a rare but aggressive type of urothelial cancer, which also affects other parts of the urinary tract, including the bladder.
2. What are the causes and risk factors for transitional cell cancer of the renal pelvis and ureter?
Several factors increase the risk of developing transitional cell cancer in the renal pelvis and ureter:
-
Tobacco use: Smoking is the most significant risk factor for TCC of the urinary tract.
-
Chronic bladder infections or inflammation.
-
Exposure to chemicals: Long-term exposure to certain industrial chemicals, particularly those used in the dye, rubber, and leather industries.
-
Previous radiation therapy: If you’ve had radiation treatment for other cancers, especially in the pelvic area.
-
Age and gender: It is more common in individuals over the age of 50 and is more frequently diagnosed in men.
-
Family history: A family history of urothelial cancer increases the likelihood of developing this disease.
-
Chronic kidney disease or dialysis: Patients on long-term dialysis have an increased risk of developing cancer in the renal pelvis.
3. What are the common symptoms of transitional cell cancer of the renal pelvis and ureter?
Symptoms of transitional cell cancer can vary depending on the location and size of the tumor. Common symptoms include:
-
Hematuria (blood in the urine): The most common symptom, which may cause urine to appear pink or red.
-
Painful urination or a sense of urgency or frequency.
-
Flank pain: Pain in the side or lower back, particularly in the area of the kidneys or ureter.
-
Unexplained weight loss and fatigue.
-
Swelling in the legs or abdomen, which could indicate the spread of cancer.
4. How is transitional cell cancer of the renal pelvis and ureter diagnosed?
The diagnosis of TCC typically involves a combination of:
-
Imaging tests: CT scans, ultrasound, and MRI can identify tumors in the renal pelvis and ureter.
-
Cystoscopy: A procedure where a camera is inserted into the urinary tract to view the bladder and ureter.
-
Urine cytology: This test checks for cancer cells in the urine.
-
Biopsy: A sample of the tumor may be taken during a procedure like a ureteroscopy or surgery to confirm the diagnosis.
-
Intravenous pyelogram (IVP): A special X-ray that uses a contrast dye to evaluate the kidneys, ureters, and bladder.
5. What are the stages of transitional cell cancer of the renal pelvis and ureter?
Staging of TCC is based on how far the cancer has spread:
-
Stage 0: The cancer is confined to the inner lining of the renal pelvis or ureter (non-invasive).
-
Stage I: The cancer has spread to the deeper layers of the renal pelvis or ureter but has not reached the lymph nodes or other organs.
-
Stage II: The tumor has spread beyond the kidney or ureter to the fatty tissue surrounding the urinary tract.
-
Stage III: Cancer has spread to nearby lymph nodes or other tissues around the renal pelvis or ureter.
-
Stage IV: The cancer has spread to distant organs, such as the lungs, liver, or bones.
6. What treatment options are available for transitional cell cancer of the renal pelvis and ureter?
Treatment for TCC of the renal pelvis and ureter depends on the stage and extent of cancer. Common treatment options include:
-
Surgery: The primary treatment for localized TCC is the removal of the affected kidney (nephrectomy) or ureter (ureterectomy).
-
Chemotherapy: Often used for advanced or metastatic cancer, especially for cancers that have spread beyond the renal pelvis and ureter.
-
Radiation therapy: In some cases, radiation is used to shrink tumors or kill remaining cancer cells after surgery.
-
Immunotherapy: For more advanced stages, treatments that stimulate the immune system to attack cancer cells may be used.
-
Targeted therapy: Newer treatments that target specific molecular mechanisms in cancer cells, often used in combination with other therapies.
7. What is the prognosis for transitional cell cancer of the renal pelvis and ureter?
The prognosis for TCC depends on the stage and location of the cancer at diagnosis:
-
Early-stage cancer: If caught early and localized to the renal pelvis or ureter, the 5-year survival rate is high, especially after surgery.
-
Advanced-stage cancer: If the cancer has spread to nearby tissues or distant organs, the prognosis is more guarded, with a lower survival rate. However, treatments like chemotherapy and immunotherapy can improve survival and quality of life.
Overall, the 5-year survival rate for all stages is approximately 50%, but this can vary widely depending on the stage and treatment response.
8. Can transitional cell cancer of the renal pelvis and ureter be prevented?
While there is no guaranteed way to prevent TCC, some steps can reduce the risk:
-
Quit smoking or never start, as tobacco use is the most significant risk factor for this cancer.
-
Limit exposure to toxic chemicals, especially in occupational settings, by following safety guidelines.
-
Hydrate well: Drinking plenty of water helps flush toxins from the urinary tract, potentially lowering the risk of urinary tract cancers.
-
Regular health screenings: People with a family history of urothelial cancer or those undergoing long-term dialysis may benefit from more frequent monitoring and early detection.
9. What are the possible complications of transitional cell cancer of the renal pelvis and ureter?
Complications of TCC can include:
-
Metastasis: Cancer spreading to distant organs such as the liver, lungs, or bones.
-
Urinary obstruction: Tumors in the renal pelvis or ureter may block the flow of urine, leading to kidney damage or infection.
-
Kidney failure: Advanced TCC may impair kidney function if the tumor obstructs the renal system.
-
Recurrence: TCC can recur after treatment, especially if the cancer is not completely removed or if it was diagnosed at a late stage.
10. How can I cope with the emotional impact of transitional cell cancer?
A cancer diagnosis can be emotionally challenging, and coping strategies include:
-
Seek professional counseling: Talking to a therapist can help manage anxiety, depression, and other emotional challenges.
-
Join a support group: Connecting with others who have gone through similar experiences can provide emotional support and coping strategies.
-
Focus on self-care: Practices such as exercise, meditation, or hobbies can improve mental well-being.
-
Talk to your family and friends: Having a strong support system is essential during treatment and recovery.
-
Stay informed: Learning about your condition and treatment options can help reduce fear and increase your sense of control.
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.